-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2021; 10(2): 13-24
doi:10.5923/j.ajdv.20211002.01
Received: Oct. 14, 2021; Accepted: Oct. 26, 2021; Published: Oct. 30, 2021

Effect of Skin Diseases in Modernized Life
Shahriar Hussain Chowdhury 1, Mahbubur Rashid 1, Md Rahimullah Miah 2, Chowdhury Shadman Shahriar 3, Tasnia Tabassum 1
1Department of Dermatology and Venereology, North East Medical College and Hospital, Affiliated with Sylhet Medical University, Sylhet, Bangladesh
2Department of IT in Health, North East Medical College and Hospital, Affiliated with Sylhet Medical University, Sylhet, Bangladesh
3USMLE Student, USA and Ex-student of North East Medical College, Affiliated with Sylhet Medical University, Sylhet, Bangladesh
Correspondence to: Md Rahimullah Miah , Department of IT in Health, North East Medical College and Hospital, Affiliated with Sylhet Medical University, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

More or less everyone suffers from skin diseases worldwide. The skin is a vital part of the body for the clear-sightedness of health and attractiveness. The skin performs as a covering for the body surface area and enhances loveliness. The skin is the largest multifunctional organ of the whole body. The aim of this study is to find the explicit tools that measure the effect of a skin disease in rationalized life. Skin disease related qualitative and quantitative data were obtained from the outpatient from the department of dermatology and venereology, North East Medical College of Bangladesh, while secondary health data were collected from diverse sources. Key dermal protecting instruments provided at the above-mentioned hospital and its challenges with gaps in individual’s existing life for patient management are highlighted. The study shows about 3841 patients were diagnosed with average age 44.5 years from the period of January to December 2019, where female is about 52% and male 48%. The study also represents about 18.54% of patients were affected by Tinea corporis, which is the highest skin disease patients in the outpatient hospital. The study also demonstrates other skin diseases including 13.95% by Scabies, 8.44% by Seborrheic dermatitis, 5.99% by acne vulgaris, 5.75 by urticaria, and 5.05% by contact dermatitis successively. Treatment model of identified skin diseases illustrates the controlling parameters with majority of interventions in clinical practices. Dermatological knowledge is crucial for healthcare with scientific novelties but such knowledge is below par. The study suggests the future research trajectories with alternative treatment options from skin disease to foster national health management and therapeutic strategies concerning Sustainable Development Goals 2030.
Keywords: Skin disease, Treatment, Healthcare and Rationalized life
Cite this paper: Shahriar Hussain Chowdhury , Mahbubur Rashid , Md Rahimullah Miah , Chowdhury Shadman Shahriar , Tasnia Tabassum , Effect of Skin Diseases in Modernized Life, American Journal of Dermatology and Venereology, Vol. 10 No. 2, 2021, pp. 13-24. doi: 10.5923/j.ajdv.20211002.01.
Article Outline
1. Introduction
- Hundreds of skin disease can affect in the existence lives surroundings, which contributed 1.79% to the global burden of disease [1,2]. Day by day the global burden of disease spreads in regional, national and local levels due to expansion of CASSID (Common Acute Sensor Sudden Infections and Disorders) [3]. Dermatophytic infections are the most common fungal infections affecting 20%–25% population globally. [20]. The skin is the largest organ of the individual’s body in terms of surface area. When there is a problem with this skin, it has a serious effect on the whole body, then the person feels uncomfortable and gradually suffers from skin disease. More or less everyone suffers from different types of skin diseases worldwide. Such diseases are more common in summer and differ from region to region. In addition, living in an unclean and densely populated environment is one of the leading causes of skin diseases. Skin conditions are varied and can often be confused due to obvious symptoms. Skin situations are diverse and can often be muddled due to noticeable signs. Skin diseases are largely interrelated to genetics, aging, allergic, hormones or exposure to sun, toxic chemicals or processed sensors. Tinea versicolor, scabies, seborrheic dermatitis, acne vulgaris, urticaria, contact dermatitis, premature ejaculation and eczema are skin diseases associated with a great recurrence rate [21,25,26,27,43]. Skin disease places significant psychosocial burden on a patient’s wellbeing that can result in psychosocial effects seriously affect their lives [30,31]. Skin contact between infants and parents contributes not only to infants’ learning their boundaries, but also positively affects the insolences of caregivers, which serves to generate feelings of well-being and self-esteem [32,33]. With advances in generic, conjugal and specific instruments measuring quality of life, there is now a greater appreciation of how skin diseases affect children and adults [34,35]. Patients with real and perceived imperfections in important body image areas, such as the face, scalp, hands, and genital area, are prone to distress [36,37]. Patients with body dysmorphic disorder, acne, psoriasis, and particularly men and women with facial conditions are more likely to have reactive depression and be at risk of suicide [38,39]. The cosmetic use of bleaching products had a huge impact on our dermatological practice [40]. On the other hand, the novel coronavirus affects many organs, including the skin, whose manifestations are a consequence of the disease itself, as well as the preventative measures taken to avoid the infection [41]. During this pandemic that has affected most of the world, many skin diseases have emerged. Excessive a cosmetic nuisance, skin disease can produce anxiety, depression, and other psychological problems that affect patients’ lives in ways equal to arthritis or other deactivating illnesses. An obligation for the effects of sex, age, living status, diet system and location of lesions is important, as well as the bidirectional relationship between skin disease, mental health and psychological distress.The study aims to find out the new innovations with interdisciplinary approaches to solve the core challenges of dermatological disease in daily life.
2. Materials and Methods
2.1. Study Site
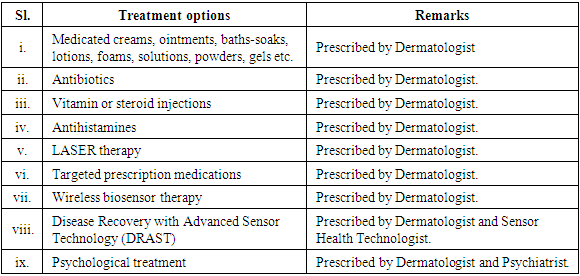
- A prospective with descriptive cross-sectional study was conducted at the Department of Dermatology, North East Medical College Hospital, affiliated with Sylhet Medical University of Bangladesh on 12 months from January 2019 to December 2019. Patients with different skin diseases were both males and females with different age-group. The study followed materials and methods of the necessities related to dermatological disease from the OPD (Out Patient Department). The methods included sample size and design, data collection, data compilation, data analysis and interpretation, and ethical consideration demonstrated consecutively as below:
 | Figure 1. Department of Dermatology, North East Medical College, Sylhet, Bangladesh |
2.2. Data Collection
- The data were collected through OPD observational patient survey among 3841 patients. Secondary data were obtained from journals, books, daily news, internet and other sources. Data collected from common dermatological diseases are seborrheic dermatitis, acne vulgaris, tinea corporis, scabies, contact dermatitis, pityriasis versicolor, urticaria, vitiligo, premature ejaculation, miliaria, impetigo, psoriasis, eczema, photodermatitis and other diseases within the stipulated time. The common diagnostic procedure for detecting the type of skin disease included: (a) physical examination, (b) skin biopsy, and (c) patch test and (d) disease severity assessment [28,29].
2.3. Data Compilation
- Patient’s medical history with information about skin diseases, domestic and occupational exposures, frequency of outbreaks and sick leave was recorded. All collected quantitative skin disease related data from primary and secondary sources were checked for accuracy and validity from the hospital research centre and related sources were also tested.
2.4. Data Analysis and Interpretation
- All compiled and managed health data were involved in the preparation of the data master sheet and cohesive into appropriate systems used in the findings, discussion and other sections consecutively. All collected data intended for analysis and interpretation using update analysis software like MS Excel 2019, SPSS version 27 and R programming ver. 3.6.
2.5. Ethical Consideration
- Each ethical issue was consulted with the patients concerning the skin study and informed written consent were added. The study was approved by the Ethical Committee of North East Medical College and Hospital, affiliated with Sylhet Medical University, Sylhet, Bangladesh. The methods were carried out in accordance with the relevant research guidelines and ethical regulations.
3. Results
3.1. Gender
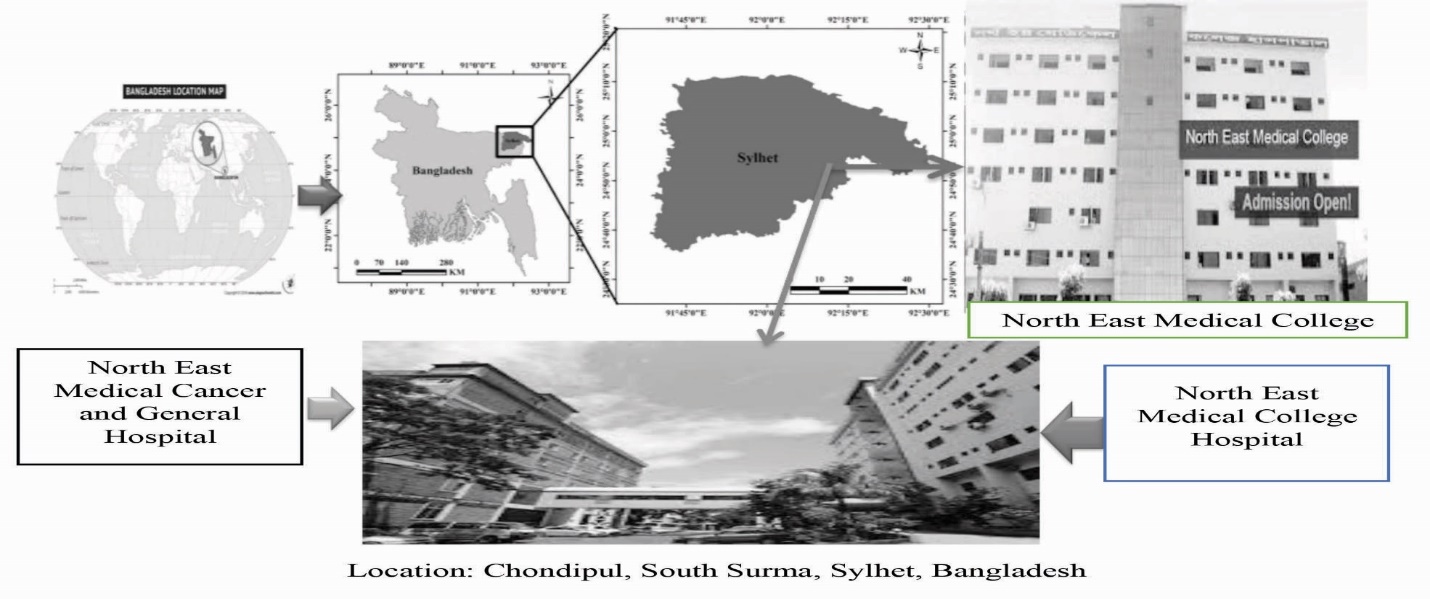
- The study represents that 52% of female and 48% of male out of total patients, which as shown in Figure 2. With respect to dermatological disease, females are frequently affected in infectious diseases, while females are more susceptible to pigmentary disorders, influenced hair diseases, emotional difficulties, particularly autoimmune and sensitive skin diseases.
 | Figure 2. The quantity of skin disease patients among male and female |
3.2. Age
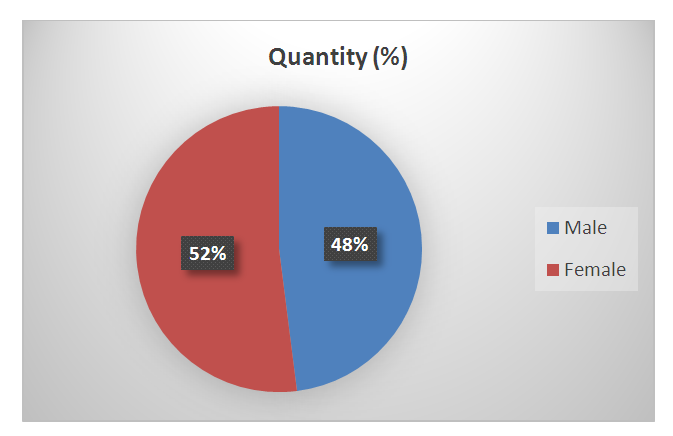
- The study shows that the age gradation is 11-20 years is maximum (28.1%) and above 80+ is minimum (0.23%), which as shown in Figure 3. Besides, 14% patients are at the age of 1 to 10 years, 22.71% in 21-30 years, 16.61% in 31-40 years, 8.37% in 41-50 years, 4.98% in 51-60 years, 2.76% in 61-70 years and 1.45% in 71-80 years respectively. The curve showed the trends line with equation of polynomial order.
 | Figure 3. Different age distribution of skin disease patients |
3.3. Patients Distribution
- The study represents that the patient’s distribution is more in the month of March round the year, where minimum in November, which as shown in Figure 4. Other months also distributed patients with dermatological diseases. The curve showed the trends line with linear equation.
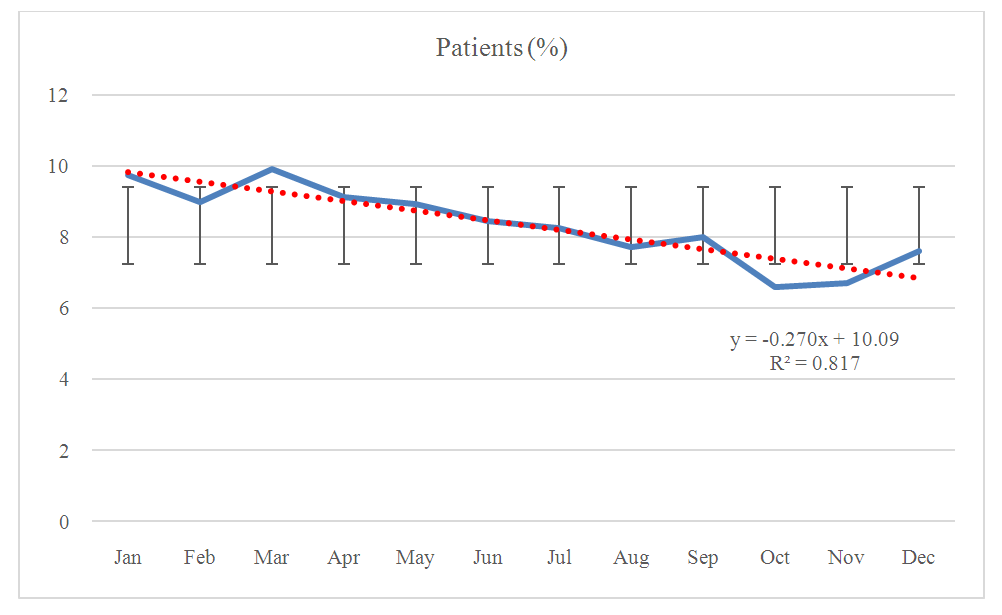 | Figure 4. Month wise skin disease patients from January to December |
3.4. Top-Ten Affected Diseases
- From the study, the top-ten skin diseases identified from different patients at the department of dermatology, North East Medical College, Sylhet. These are Tinea Corporis, Scabies, Seborrheic Dermatitis, Acne Vulgaris, Urticaria, Contact Dermatitis, Premature Ejaculation, Eczema, Photodermatitis and Pityriasis versicolor. Out of them, the highest patients were in Tinea Corporis (18.54%) and Scabies is the second top-skin disease (13.95%), which as shown in Figure 5.
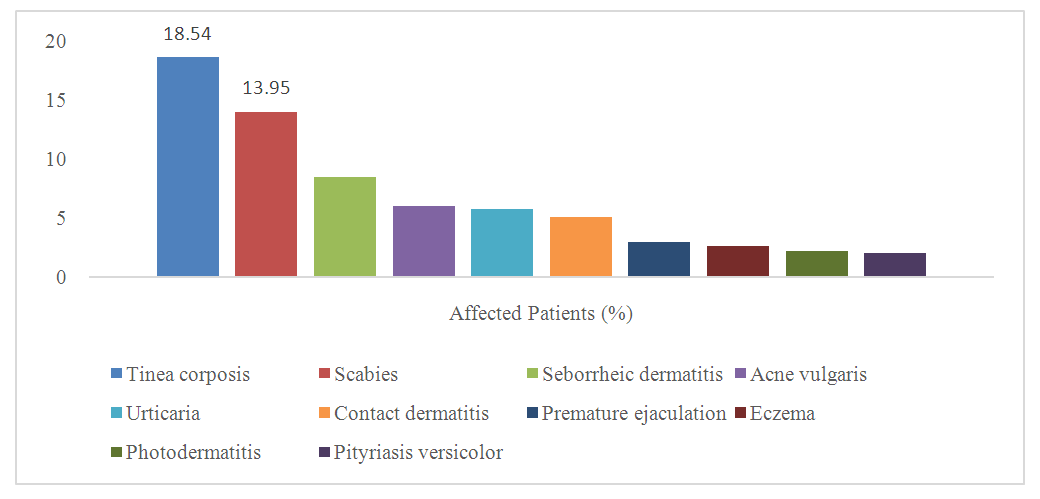 | Figure 5. Top-ten affected dermatological diseases |
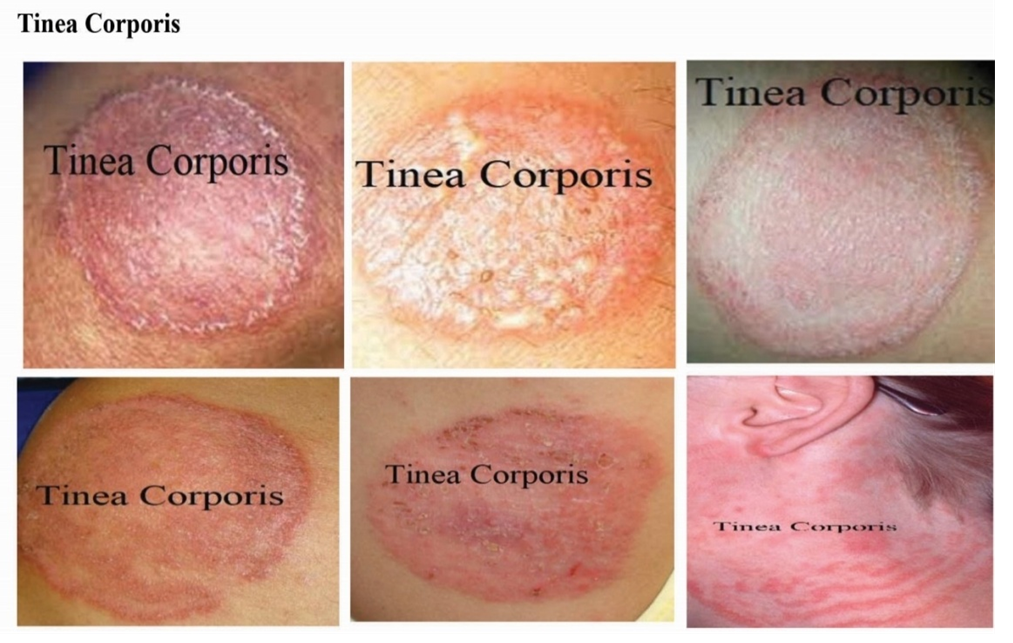 | Figure 6. Identified skin disease symptoms on Tinea Corporis |
 | Figure 7. Identified skin disease symptoms on Scabies |
 | Figure 8. Identified skin disease symptoms on Seborrheic Dermatitis |
 | Figure 9. Identified skin disease symptoms on Acne Vulgaris |
 | Figure 10. Identified skin disease symptoms on Contact Dermatitis. |
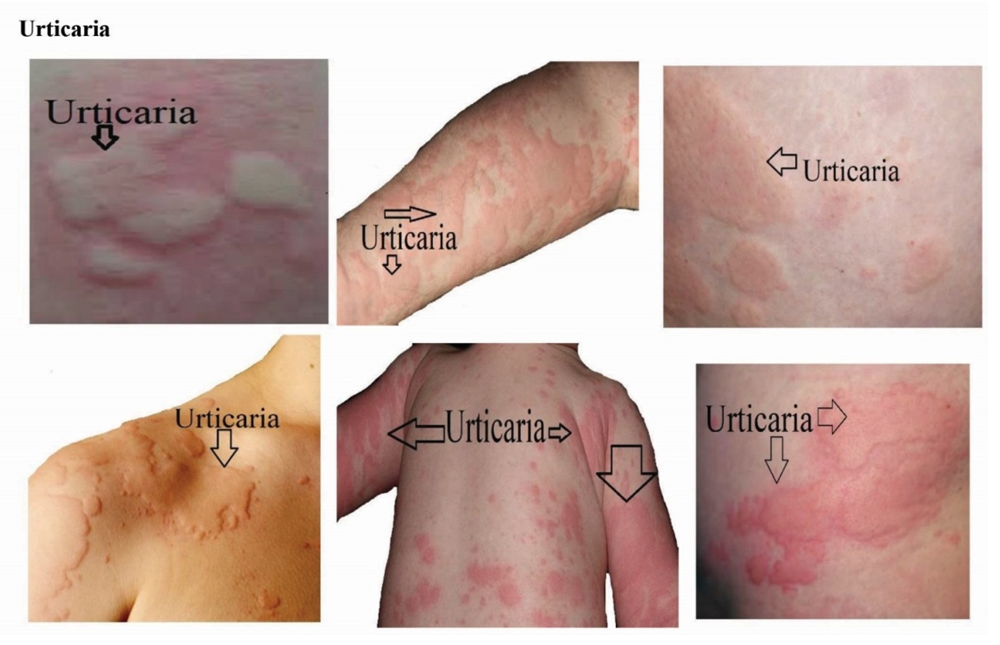 | Figure 11. Identified skin disease symptoms on Urticaria |
4. Discussion
- The study indicates on the impact of dermatological diseases in our daily life through the survey of outpatients at the department of dermatology of North East Medical College Hospital in Sylhet, Bangladesh. Skin diseases are a key health problem distressing a vital part of living people, who are mentally and physically challenged in the community [22]. Patient education is a significant part of patient-care laying at the vital of clinical dermatology [23]. Positive education promotes their pleasures as a ‘gold standard’ and results in enhanced outcomes and commitments [24,56]. Education interventions cover a broad range of approaches that may be directed at the parents, family and community [15]. These interventions, which can include audiovisual tools, printed literature, lectures, demonstrations and interactive session formats are aimed to changing behavior by increasing knowledge or skills and thereby empowering self-management. They can be delivered by various individual members of the healthcare team, by multidisciplinary teams or as self-directed learning. They may be combined with psychological interventions. A systematic review [8] and randomized [9-13] controlled trials involving education intervention in adolescent and adult patients reported significant benefits. These included improved severity and self-care, increased knowledge of treatments and reduced need for medical help. There is some evidence that education intervention in addition to standard therapy improves atopic eczema disease control [14]. These interventions should be delivered by suitably trained personnel. The most effective educational process still needs to be researched. Health education measures have proved to be effective in the case of patients with occupational skills disorders in the sense of behavior prevention and condition prevention [19]. Images of skin of color are understated in plenty dermatology educational resources for searching further improvement with resident’s knowledge and better serve for patients [18]. The following discussion enhances the daily life for the management of dermatological diseases.
4.1. Dermatological Disease Management
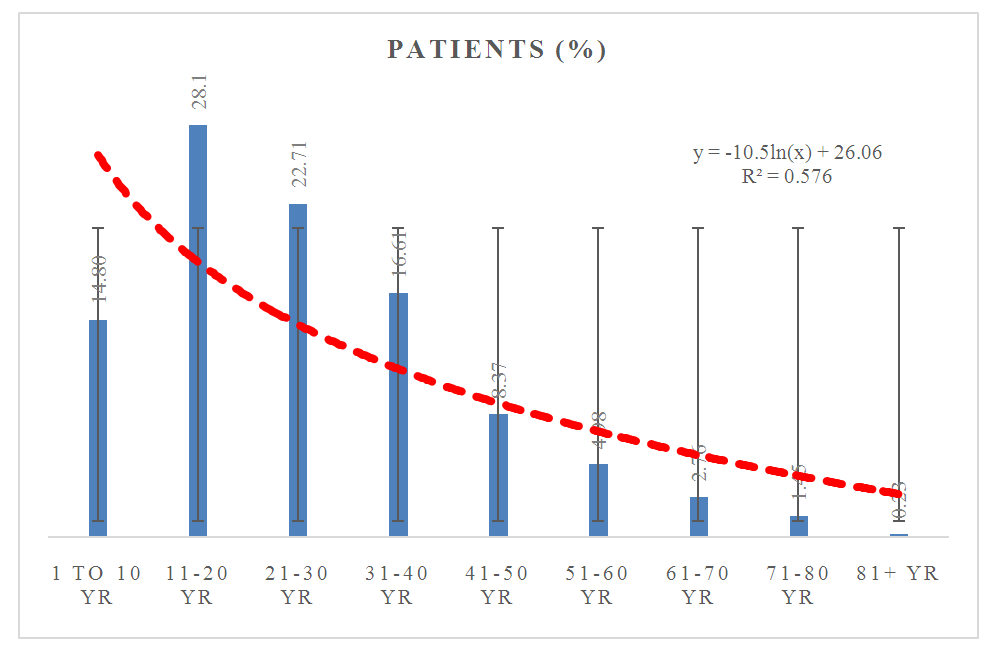
- Treatment includes diverse parameters to manage dermatological diseases. Awareness on the effect of chemical, physiological and biophysical differences between the skin of individual patients help dermatologists change the proper approach not only for the dermatological disease management but also to accurately take care of modern cosmetic issue in-body environment, nutritional support and dietary [42,44,45]. Skin disease management relates with the functions on clinical dilemma as a protective physical barrier by absorbing ultraviolet radiation, tracking wireless sensor particle and avoiding microorganism invasion and chemical penetration at a fixed GPS location, which as shown in Figure 12. Treating skin disorders with different options shows in Table 1. Some skin diseases recover with ice-block and DRAST (Disease Recovery with Advanced Sensor Technology) due to tightly closed eyes, changeable GPS locations and silent voice mood [55].
|
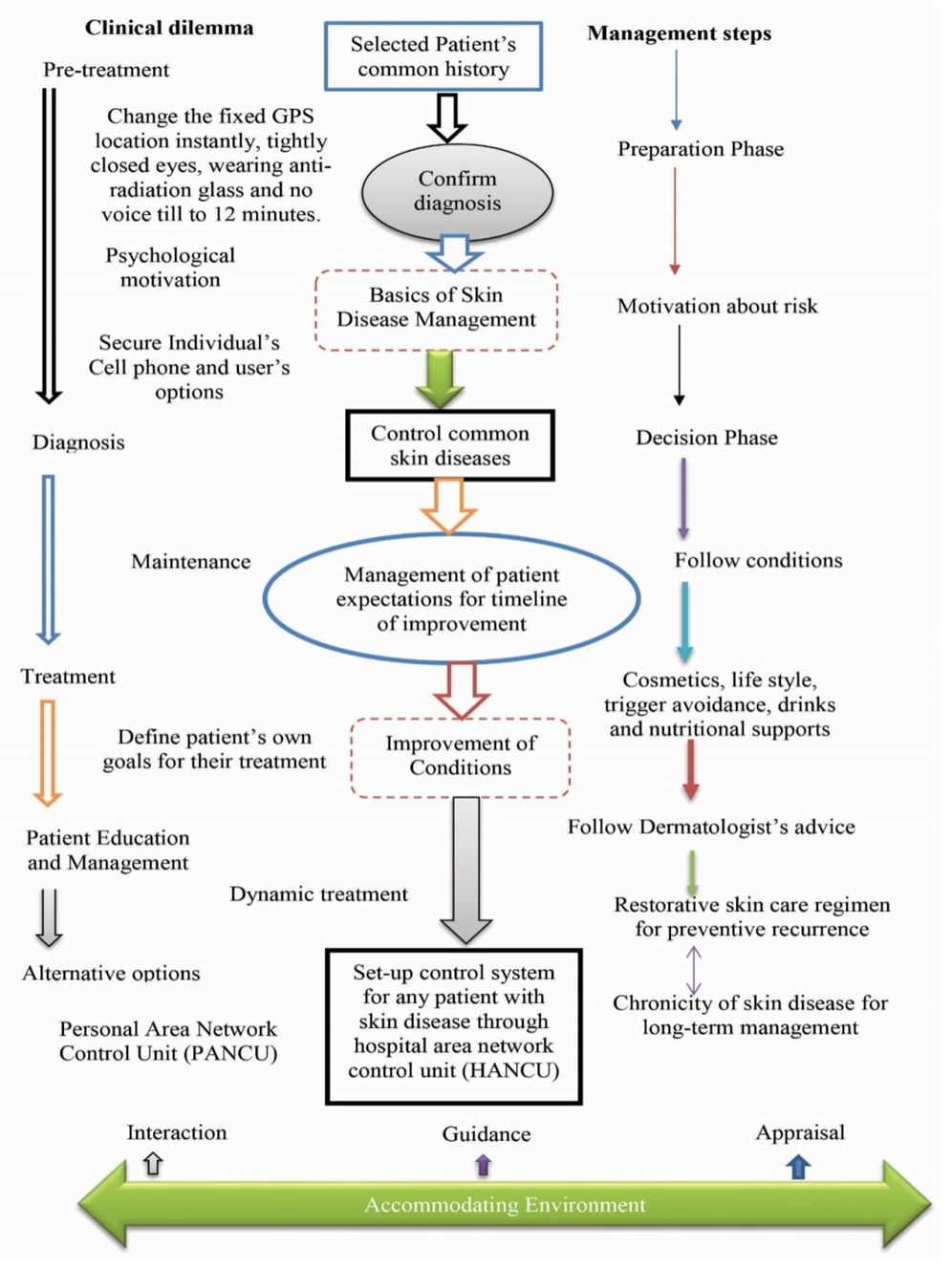 | Figure 12. Management of Dermatological Disease with relevant parameters |
4.1.1. Dermatology at a Fast Pace
- Females are a higher degree of emotional distress and a higher degree of discomfort from skin diseases than males [59,60]. Every human being needs fresh, bright, flawless, smooth skin. But many may not be able to pay attention to the time spent on it. For many people, spending extra time on beauty care after a long day's work is a real hassle. Again, many find it a waste of time and money to pursue beauty. That is why it is not permissible for everyone to be beautiful. Some take a little care, but it is considered very good if it is done regularly. There will be a lot of quick skin care work. If individuals don't do it at all, they have to add some shortcut strategies with dermatologic ideas and pace every day.
4.1.2. The Solution in Water
- Proper use of water can also keep individual free from skin diseases. Those who are reluctant to spend both time and effort, if they just clean the skin with regular water, it is 25 percent of the work to stay free from skin diseases [61]. Many people know that proper use of water is very important to keep skin and hair healthy. In addition, the person concerned can keep an account of how many liters of water are being drunk throughout the day, how much water is getting to the hair and skin, and how much is still fresh. Individuals do nothing else throughout the day, wipe their face a few times with a wet towel or splash water, then they will find a solution. It is better for the person to use cold water in this case. And if individuals give a splash of water, they have to wipe their face gently immediately. We need to keep in mind that water keeps the skin fresh and moist. If individuals want to spend some more time, they can use hydrating cream in the morning and at night. It is mentioned, if the skin is not dehydrated, the problem will be reduced by half. So, it is very easy to take care of the skin through water.
4.1.3. Before Going to Sleep
- Skin disorders are inconsistently allied with sleep disturbance and deprivation including obstructive apnea [64]. Before going to sleep, individual can take care of his/her teeth as well as take some care of their skin to get rid of skin diseases. The person concerned does not need to spend extra time on it. It can solve the problem of acne, chapped lips and dry skin [43]. If individual want, they can apply the toothpaste they are using for brushing their teeth on the acne. And there are many benefits to rubbing their lips gently with a toothbrush. Oral health and mucocutaneous inflammation play a significant role in the etiopathogenesis of dermatological diseases [65]. When the person wakes up in the morning, he will see that his lips have become soft, as well as acne. However, in this case, it should be noted that in the case of all types of acne and dermatitis, but the toothpaste is not the solution.
4.1.4. Cleansing Oil for Treatment
- Dermatitis can also be treated with cleansing oil in gender differences [58]. Many people do not want to use multiple beauty products at once. Cleansing oil is good for them. Many people may not know that cleansing oil is a kind of oil. However, it is very effective in cleansing the skin. At the same time, it is effective in melting makeup, as it penetrates deep into the skin and removes oil and dirt. It is very effective in removing daily dust and dirt as well as on acne. At the end of the day, if individuals massage their face with cleansing oil for five to seven minutes, blackheads and whiteheads will be removed easily. The skin will be clean. If there is makeup, it will also come up.
4.1.5. Lockdown Skin Problems and Remedies
- We had to stay at home in lockdown for a long time because of the corona virus. That is why we are all going through an uncertain time. Coronavirus has changed our lives a lot. This is having an adverse effect on our skin. For this reason, various skin problems are appearing during the lockdown. The appearance of healthy skin enhances the quality of life everywhere [62]. Somewhere it will be fair, somewhere it will not be black. They will not be excessively oily or dry. There will be no spots or sores anywhere on healthy skin. There are several skin problems during lockdown. The skin is turning black or the skin is becoming pale after a long stay at home and less exposure to the sun. In addition, there is an impression of fatigue on the face of many. Those who already had skin problems, it has increased anew. Because, he could not get good treatment for lockdown. Staying at home has made many people reluctant to take care of their skin. As a result, oily skin has become oilier. Dry skin has become excessively dry. Vitamin D is also very important for the skin. Vitamin D is deficient in the skin and body due to less sun exposure from house arrest. Again, many people are getting tired of the lockdown. It has an effect on the skin.
4.1.6. The Relationship of Skin to Mental Health
- Skin health has a subtle and intimate link with mental health [56]. Skin is a mirror of human health; Especially mental health. If someone has a skin problem, he goes into depression. And the stress from the lockdown is creating a lot of bad habits. For example, teenage children are getting fat from home. Because, they are buying food by ordering online for stress relief. Taking diet as a recreation. Eating unhealthy foods causes stretch marks on the skin and black spots on the neck. Waking up at night, and sleeping during the day. The black spot is falling under the eyes. For these reasons, the growth of children is abnormal. Being taller is shorter. And due to the lack of vitamin D, the bone structure in the body is not getting better, the metabolism is not going well. The effects of aging on the skin of middle-aged men and women are falling very fast just because of the lack of movement and stress.
4.1.7. Dermatitis Due to Sensor Technology
- Dermatitis is caused by the misuse of sensor technology [55]. If a person is at a certain GPS distance with the open active eyes, then the existed cyber hacker tracts suddenly the skin of a person or an animal through high frequency wireless sensor technology, which immediately stops the movement of electrons on that radiated skin and causes skin disease. However, if the person closes his eyes at the initial stage and changes his GPS position quickly, the person can be protected from skin diseases.Overall, many people have had skin diseases in their daily life, including coronavirus disease, and they have been abnormally affected by various diseases. Dermatitis caused by neglect of the immune system can be fatal [63], if it limits the effectiveness of the work of the affected people, which is an unintended consequence, especially when health workers are infected with the disease. Again, limited information on pandemics, including dermatosis, maintaining psychotic stress, the use of irritating and harsh chemicals, its significant impact on patients' quality of life, the marketing of unplanned cosmetics, and the misuse of sensor technology, is still limited information to recover from dermatological diseases. The strength of the dermatological study is the high response rate together with the comprehensive evidence about the doctors, patients and health professionals with respect to disease and treatment systems. The weakness of the study is that the data is questionnaire-based and observation at OPD, and that information about skin disease severity is assessed without the advanced sensor technology.
4.2. Risk in Dermatology
- Diverse data on treatment of dermatological diseases are inadequate, and differences between males and females with respect to advanced treatment are not well illustrated. The use of laser and cosmetics has enormously contributed to dermatology with different types of lasers and cosmetics in gender aspects providing a range of clinical benefits [46,47,48,49,50,51,52,53,54]. But their excessive uses and adultery are risk in daily life. Individual affects in skin disease due to misuse of wireless sensor technology at a fixed GPS (Geographic Positioning System) location and GNSS (Global Navigation Satellite System) positions [55].
5. Conclusions
- Finally, we conclude that skin diseases are common among male and female in outdoor patients at the department of dermatology, North East Medical College Hospital in Sylhet, Bangladesh. The clinical experience is that females are more accustomed to and more enthusiastic to use contemporary treatments except investigation and documentation. Everyone uses different types of cosmetics but none can know its impact due to unauthenticated elements. The study will enhance to all on the priority of the medical, nutritional and psychosocial conditions of such patients by regular follow up, medical campaigns, ensure adequate access to healthcare services at the community and institutional levels in daily life.
6. Declaration
- FundingThis research work is financed by the Higher Authority of North East Medical College, affiliated with Sylhet Medical University, Sylhet, Bangladesh.Data AvailabilityThe data being used to support the findings of this research work are available from the corresponding author upon request.Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of North East Medical College & Hospital (NEMCH), affiliated with Sylhet Medical University, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML