-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(5): 61-64
doi:10.5923/j.ajdv.20200905.01
Received: Apr. 11, 2020; Accepted: Jun. 12, 2020; Published: Oct. 26, 2020

A Comparison between the Efficacies of Fluconazole and Ketoconazole in the Treatment of Tinea Versicolor
GM Matiur Rahman1, AKM Zayedul Haque2, MJ Abedin1, Hoq AJMS1, Sultana F.3
1Dept. of Dermatology and Venereology, Cumilla Medical College Hospital, Cumilla, Bangladesh
2Dept. of Dermatology and Venereology, Sheikh Hasina Medical College Hospital, Tangail, Bangladesh
3Emergency Medical Officer (EMO), Mymensingh Medical College Hospital, Mymensingh, Bangladesh
Correspondence to: GM Matiur Rahman, Dept. of Dermatology and Venereology, Cumilla Medical College Hospital, Cumilla, Bangladesh.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Both fluconazole as well as ketoconazole are Azole antifungal agents. Ketoconazole has two Nitrogen atoms in its azole ring and fluconazole has three N-atoms. Both the drugs work by inhibiting the cytochrome P450 dependent enzyme and are used widely in the treatment arena of Dermatology. Tinea versicolor (TV) or pityriasis versicolor is caused by a type of yeast that naturally lives on human skin. Aim of the study: The aim of this study was to compare the efficacies of fluconazole and ketoconazole in treating tinea versicolor. Methods: This comparative prospective study was conducted in the Department of Dermatology of Cumilla Medical College Hospital, Cumilla, Bangladesh during the period from January 2018 to December 2018. In total 60 patients with tinea versicolor, age around 15–55 years, were finalized as the study population who has continued up to the end of the full tenure of this intervention. The patients were randomly divided into equal two groups. Patients of Group I (n=30) received 300 mg fluconazole as a single dose and repeated weekly for 2 weeks and patients of Group II (n=30) received 400 mg ketoconazole as a single dose and repeated weekly for 2 weeks. Diagnosis of TV was made clinically and by direct KOH preparation. Result: After completing 1 (One week) treatment we got 60% mycological cure rate in Group I patients who were treated by fluconazole. On the other hand this rate was 56.67% which was some less than that of Group II and these patients were treated by Ketoconazole. On the other hand, after completing 2 (Two weeks) treatment we got 93.33% mycological cure rate in Group I patients who were treated by fluconazole. On the other hand this rate was 86.67% which was some less than that of Group II and these patients were treated by Ketoconazole. Conclusion: Although in our study we found some superiority of fluconazole regarding efficacy over ketoconazole in treating tinea versicolor but the ratio was not remarkable. Both the antifungal agents of Azole group were well tolerated.
Keywords: Fluconazole, Ketoconazole, Azole, Tinea Versicolor
Cite this paper: GM Matiur Rahman, AKM Zayedul Haque, MJ Abedin, Hoq AJMS, Sultana F., A Comparison between the Efficacies of Fluconazole and Ketoconazole in the Treatment of Tinea Versicolor, American Journal of Dermatology and Venereology, Vol. 9 No. 5, 2020, pp. 61-64. doi: 10.5923/j.ajdv.20200905.01.
Article Outline
1. Introduction
- Both fluconazole and ketoconazole are Azole antifungal agents. Ketoconazole has two Nitrogen atoms in it’s azole ring and fluconazole has three N-atoms. Both the drugs work by inhibiting the cytochrome P450 dependent enzyme and are used widely in the treatment arena of Dermatology. Tinea versicolor is caused by a type of yeast that naturally lives on human skin. It is a very common fungal infection of the skin. The fungus interferes with the normal pigmentation of the skin, resulting in small, discolored patches. These patches may be lighter or darker in color than the surrounding skin and most commonly affect the trunk and shoulders. Colour of the affected skin can vary from brown to red and hypo-pigmented patches may also be present. [1] Klenket al [2] has observed that Tinea versicolor is more frequently seen in humid, warm climates or in the tropics than in dry cold zones. Rao et al, has also found that, 35% of the patients had the disease first in summer and this could probably be due to increased sweating. There by, predisposing the person to the infection. [3] TV is found worldwide, but is most prevalent in the tropics where there is high humidity, high temperatures and frequent exposure to sunlight. [4] The aetiological agent is Malassezia furfur (also called Pityrosporum orbiculare or P. ovale), a lipophilic yeast. [5] The disease is most prevalent in early adulthood and small children are rarely affected. [6] TV is common in the post-pubertal age where sebaceous glands are active and in individuals who sweat more. [7] There is often a positive family history of the disease. [8] Dermatologists uses many single or combined, superficial or systemic drugs in the treatments of TV. But, according to investigators, all topical therapies are associated with a relatively high recurrence rate (60–80%). [1] The main problem with the use of topical antifungals is the difficulty of applying creams to such a large body surface area. For this reason TV is perhaps more easily treated with systemic agents such as ketoconazole, itraconazole and fluconazole. 3-6 Ketoconazole was the first oral antifungal drug to be shown to be effective in the treatmentof TV. It is a substituted imidazole derivative and inhibits the biosynthesis of ergosterol a major membrane lipid of the causative yeast. [7] Ketoconazole is absorbed in the small intestine and is rapidly carried (in 1 hour) via sweat and passive diffusion through the blood to the skin, where it stays in the stratum corneum for 10–12 days. Since ketoconazole is excreted in the eccrine sweat, methods such as exercise can be used to promote delivery of the drug to the skin. [3] By a slower route, it reaches the basal cells of the epidermis and sebum after 3–4 weeks. [7] Though usually well tolerated, the most worrisome adverse reaction to ketoconazole is hepatotoxicity (incidence of between 1 in 10000–15000). Other adverse side effects include nausea, gynaecomastia, infertility, decreased libido and oligospermia. [3] Oral ketoconazole is recommended treatment for TV. [7] Fluconazole is a member of the azole group of antifungal agents, and has proven efficacy in the treatment of infections caused by Candida albicans. [10] Favorable pharmacokinetics of fluconazole, especially its slow elimination from the skin, allow its effective systemic administration in single weekly doses in a variety of superficial fungal infections such as tinea cruris, tinea corporis and tinea pedis. [12] Generally, fluconazole has been found to be safe when treating superficial skin infections. Ketoconazole is also widely used in the treatment of several tinea infections. Our aim of this study was to compare the efficacies of fluconazole and ketoconazole in treating tinea versicolor (TV).
2. Objectives
- a) General objective:• To compare the efficacies of fluconazole and ketoconazole in treating tinea versicolor.b) Specific Objectives:• To assess the demographic status of patients with tinea versicolor.
3. Methodology & Materials
- This was a comparative, prospective study and was conducted in the Department of Dermatology of Cumilla Medical College Hospital, Cumilla, Bangladesh during the period from January 2018 to December 2018. In total 60 patients with tinea versicolor, age around 15–55 years, were finalized as the study population who has continued up to the end of the full tenure of this intervention. The patients were randomly divided into two groups. Patients of Group I(n=30) received 300 mg fluconazole as a single dose and repeated weekly for 2 weeks and patients of Group II(n=30)received 400 mg ketoconazole as a single dose and repeated weekly for 2 weeks. Diagnosis of TV was made clinically and by direct KOH preparation. The inclusion criteria were: According to the inclusion criteria patients with TV for at least I month, free from any topical treatment for 2 weeks and free from systemic antifungal for at least 1 month were included in the study as study participants. On the other hand according to the exclusion criteria patients with less than 15 years, pregnant and lactating mothers and patients with history of liver diseases were excluded from the study. The study was approved by the local ethical committee. The written consents were taken from all the participants before starting the study. Complete blood count and liver and renal function tests were checked for every patient before the study and at week 2. At each visit, patients were examined regarding scaling, hyper pigmentation, hypo pigmentation and pruritus. Mycological evaluations which included direct KOH preparation from the most prominent lesion and Wood’s lamp examination were also performed. Mycological cures were defined when the KOH examination was negative (absence of yeast). Appearance under Wood’s light was compared to the KOH preparation for every patient, but was not considered as part of the mycological result. At the end of the study, the investigator and patients assessed the efficacy and tolerability of the treatment. For statistical analysis chi-square and SPSS version 20 ware used in the study.
4. Result
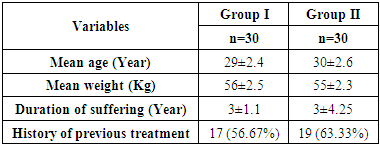
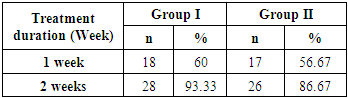
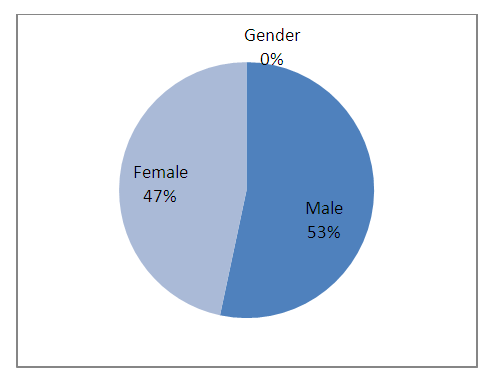
- In total 60 patients with tinea versicolor aged around 15–55 years were finalized as the study population who has continued up to the end of the full tenure of this intervention. The patients were divided into two groups. Patients of Group I (n=30) received 300 mg fluconazole as a single dose and repeated weekly for 2 weeks and patients of Group II (n=30) received 400 mg ketoconazole as a single dose and repeated weekly for 2 weeks. Among total study population 32(53.33%) were male and 28(46.76%) were female. So the male was dominating and male female ratio was 1.14:1. The mean age in Group I was 29±2.4 years and in Group II it was 30±2.6 years. The mean weight in Group I was 56±2.5 Kg and 55±2.3 Kg in Group II. The patients from Group I had suffered from TV for 3±1.1 years whereas the duration of this period was 3±4.25 years. After completing 1 (One week) treatment we got 60% mycological cure rate in Group I patients who were treated by fluconazole. On The other hand this rate was 56.67% which was some less than that of Group II and these patients were treated by Ketoconazole. On the other hand, after completing 2 (Two weeks) treatment we got 93.33% mycological cure rate in Group I patients who were treated by fluconazole. On The other hand this rate was 86.67% which was some less than that of Group II and these patients were treated by Ketoconazole. So in our study we found some superiority of fluconazole regarding efficacy over ketoconazole in treating tinea versicolor.
 | Figure 1. Gender distribution of study population (N=60) |
|
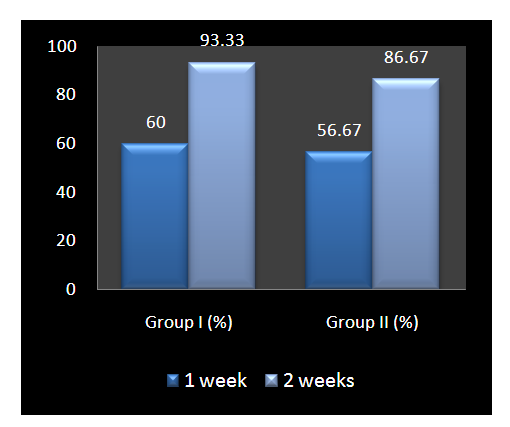 | Figure 2. Mycological cure rate among both groups (N=60) |
|
5. Discussion
- In this present study, the prevalence of disease was more among males accounting to 53% when compared to females (47%). Rao et al [14] Maheshwariamma, and Singh et al [15] have also observed almost similar results with more prevalence of cases in males. This possibly could be attributed to their profession and outdoor activities. The results of this randomized, double-blind trial clearly demonstrate that treatment of tinea versicolor with fluconazole 300 mg/week for 2 weeks is as effective as ketoconazole 400 mg given once weekly for 2 weeks. The subsequent slight decline in cure rate can be explained by the recurrence rate of tinea versicolor. It is established that, tinea versicolor is a skin disease associated with a great recurrence rate. Pityriasis versicolor or tinea versicolor recurs at a variable rate in treated individuals, and 60% to 90% of patients relapse within 2 years in some series. [16] For this reason, it is important to assess a prophylactic regimen that may be more effective and safer in preventing the recurrence of tinea versicolor (TV). The aim of this study was to compare the efficacies of fluconazole and ketoconazole in treating tinea versicolor. Besides this we had an objective to assess the demographic status of patients with tinea versicolor. In our study we found some superiority of fluconazole regarding efficacy over ketoconazole in treating tinea versicolor. But in analyzing the demographic data of the patients from both the group we didn’t find any significant co-relation between both the groups. Both fluconazole and ketoconazole were well tolerated and no serious drug-related events were reported in our study. We also found no relationship between mycological cure and the presence of skin.
6. Limitations of the Study
- It was a single centered study with small sized samples. So the findings of this comparative study may not reflect the exact scenario of the whole country.
7. Conclusions and Recommendations
- We found some superiority of fluconazole regarding efficacy over ketoconazole in treating tinea versicolor but the ratio was not remarkable. For getting more specific discoloration at the end of the treatment regime. Patients should therefore not expect a fast resolution of discoloration and be aware that, the remaining hypo/hyperpigmentation does not mean that it was a failure of treatment. We think, we should conduct more studies for assessment of all the members of Azole group for choosing better options to ensure better compliance in treating tinea versicolor. We would like to recommend for conducting more studies in several places regarding the same issue.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML