-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(4): 55-59
doi:10.5923/j.ajdv.20200904.03
Received: Aug. 14, 2020; Accepted: Sep. 30, 2020; Published: Oct. 15, 2020

Polycystic Ovary Syndrome in Psoriasis Patients: A Case – Controlled Study
Hussam Ali Salman1, Sarah Abbas Jabur2
1Iraqi Board for Medical Specializations, Baghdad, Iraq
2Dermatology Center, Medical City, Baghdad, Iraq
Correspondence to: Sarah Abbas Jabur, Dermatology Center, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

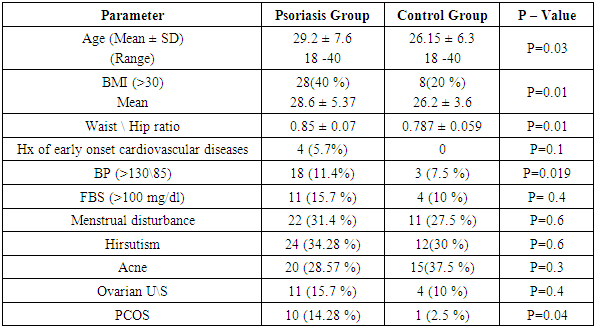
Background: Psoriasis is a chronic inflammatory disease where much comorbidities can occur. Polycystic ovary syndrome (PCOS) is common in females of reproductive age with similarity to psoriasis in its relation to metabolic syndrome. Objective: to investigate the association between psoriasis and polycystic ovary syndrome. Patients and Methods: This is a case – controlled comparative study. It was conducted at the dermatology center, Medical City, Baghdad teaching hospital from Oct 2018 to Oct 2019. We analyzed (70) female patients with psoriasis aged between (18-40) years and (40) apparently healthy controls aged between (18-40) years. Detailed history, clinical examination, abdominal sonography and hormonal assays were obtained for both groups. Results: In this study it was found that the percentage of PCOS in psoriasis patients (14.28%) is significantly higher than in control group (2.5%) (P-value=0.04). Psoriasis patients with PCOS had more association with PASI score > 10 in addition to more risk of associated disease like elevated fasting blood sugar and hypertension than psoriasis without PCOS. Conclusion: The incidence of PCOS in women with psoriasis is higher than in control women, this association makes psoriasis patients with PCOS more suspecitible to hormonal disturbances, metabolic derangement including impaired glucose tolerance test and higher PASI score. Psoriasis patients have higher BMI, WHR and blood pressure than control patients.
Keywords: Psoriasis, Polycystic Ovary Syndrome
Cite this paper: Hussam Ali Salman, Sarah Abbas Jabur, Polycystic Ovary Syndrome in Psoriasis Patients: A Case – Controlled Study, American Journal of Dermatology and Venereology, Vol. 9 No. 4, 2020, pp. 55-59. doi: 10.5923/j.ajdv.20200904.03.
Article Outline
1. Introduction
- Psoriasis is a chronic immune-mediated inflammatory disease that affects 2% of the general population. Psoriasis characterized by erythematous scaling plaques on the extensor surfaces of the body, with different clinical manifestations. Evolving data suggest that psoriasis is a complex disorder caused by the interaction between multiple predisposing genes, the immune system, and environmental factors [1]. Recent studies have shown that patients with immune-mediated inflammatory disease have a higher prevalence of comorbidities, including diabetes, cardiovascular disease, metabolic syndrome (MS) [2].The components of metabolic syndrome, obesity, diabetes, insulin resistance, dyslipidemia, hypertension, and coronary artery disease are also associated PCOS, a common endocrine disorder in women of reproductive age. According to Rotterdam criteria two of the following criteria are sufficient for diagnosis: oligo- or anovulation, biochemical or clinical hyperandrogenism, and polycystic ovaries on ultrasound examination [3]. Although the cause of PCOS is unknown, PCOS has been linked to insulin resistance (IR) and obesity. Hyperinsulinemia participate in or cause the abnormalities seen in the hypothalamic-pituitary-ovarian axis that lead to PCOS [4].Based on these similarities regarding MS and IR female patients with psoriasis in the reproductive period are thought to have a higher risk of PCOS. Additionally, the women with psoriasis and PCOS had more insulin.Resistance, more hyperinsulinemia, and lower high density lipoprotein (HDL) cholesterol levels compared to the patients with psoriasis alone [5]. The etiology of these associations are not clear, but common inflammatory mechanisms may have an influence, TNF-α which is a pro-inflammatory cytokine that affects lipid metabolism, insulin resistance, and endothelial function. It play a role in the inflammatory course of both psoriasis and PCOS, and TNF-α can trigger both PCOS and psoriasis [6].
2. Patients and Methods
- This is a case controlled study. It was conducted at the outpatient clinic of Dermatology Center, Medical City in Baghdad / Iraq for the period of one year from 1st of Oct 2018 to 1st of Oct 2019).Two groups of subjects were collected, the first group included (70) female patients were diagnosed with chronic plaque psoriasis aged between (18-40) years, the second group included (40) apparently healthy controlaged between (18-40) years.Informed consent was obtained from each participant before enrollment. Exclusion criteria √ Diabetes mellitus, thyroid disease. √ Other disorders with a similar clinical presentation to PCOS (such as adrenal hyperplasia, Cushing syndrome and androgen congenital secreting tumor) largely dependent upon history and clinical examination because of the unavailability of laboratory tests that confirm the diagnosis at time of the study. √ Treatment with clomiphene citrate, oral contraceptives, antiandrogens, drugs to control appetite or insulin-sensitizing drugs (metformin, pioglitazone, and rosiglitazone) during the past six months before the evaluation.In case of systemic treatment for psoriasis at the time of enrolment, patients were evaluated after a drug wash-out period of two months.All participants were subjected to the following:Detailed history including age, gender, occupation, marital status, history of oligomenorrhea, hirsutism, acne, history of early coronary heart disease, drug intake. Psoriasis history include: onset, duration, associated diseases, family history of psoriasis.General examination: height, weight, body mass index, blood pressure, waist / hip ratio (WHR).PASI score was applied to measure the severity of psoriatic plaques.Psoriatic plaques are graded based on three criteria: redness, thickness, and scaliness in four body regions (head, upper extremities, trunk, and lower extremities) [7].• For the Waist – hip ratio, waist circumference was measured as the smallest trunk circumference midway between the lowest rib margin (12th rib) and the iliac crest at the end of gentle expiration with patient in standing position, and the hip circumference was measured around the widest portion of the buttocks with the tape parallel to the floor [8].• Hirsutism was evaluated by the presence of terminal hair in a male pattern distribution [9], and clinical acne was defined by a history of persistent acne (presence of acne on most days for at least three years) and presence of more than 10 inflammatory acne lesions [10]. Oligomenorrhea was defined by menstrual cycles more than 35 days apart but less than six months apart [9].Investigations were performed for all patients in the study including:Ø Fasting blood sugarafter a 12 hrs. fasting period, pregnancy test(for married women).Ø Hormonal study:LH and FSH: The concentrations of these hormones were determined by direct immunoenzymatic assay in serum of samples obtained on day 2 or 3 of the natural cycle in menstruating women. The ratio of LH/FSH of two or more was regarded a significant level.Total testosterone was determined by direct immunoenzymatic assay in the serum of samples, prolactin levels, and thyroid function test also was measured.Ø Abdominal ultrasonography: the presence of 12 or more follicles measuring (2-9mm) in diameter or an ovary that has a volume greater than 10ml is needed to define the polycystic ovary. The presence of a single polycystic ovary is sufficient to provide the diagnosis [9].Diagnosis of polycystic ovary syndrome Patients of both groups were evaluated for polycystic ovary syndrome. It was diagnosed according to Rotterdam Criteria as two of the following three criteria are required [11]:1. Oligomenorrhea/ amenorrhea.2. Hyperandrogenism: clinically diagnosed by the presence of excessive acne or hirsutism (terminal hair in a male pattern distribution) or chemically by elevated levels of total testosterone.3. Polycystic ovaries on ultrasound.Statistical analysisStatistical analysis was calculated using IBM SPSS V.20 in which chi square and independent T-test were used to compute P value; P-value less than 0.05 were considered significant.
3. Results
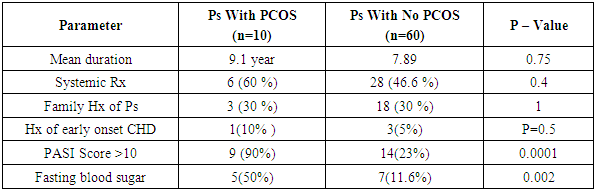
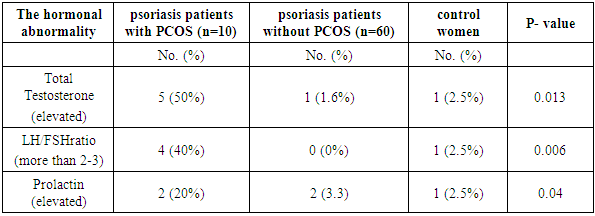
- This study was carried out on 70 female psoriasis patients and 40 apparently healthy control group.The Prevalence of PCOS in psoriasis group was 10 (14.28%) versus 1 (2.5%) in the control group (P-Value= 0.04). The clinical and biochemical characteristics of psoriatic and the control group also shown in (Table 1).In addition to BMI and WHR other risk factors for metabolic disturbance and cardiovascular risk factors such elevated blood pressure, family history of early ischemic heart disease and fasting blood sugar were assessed.Ovarian ultrasound examination for both groups is also checked, signs of polycystic ovaries seen in 11 (15.7%) in psoriasis group and 4 (10%) in the control group (p-value= 0.4). (Table 1).Regarding hormonal abnormalities total testosterone was found to be elevated in 5 (50%) psoriasis patients with PCOS, 1 (1.6%) psoriasis patients without PCOS and in 1 (2.5%) control women and the difference was significant (P-value=0.013) (Table 3).The elevated ratio of LH/FSH (> 2-3) was found in 4 (40%) Psoriasis patients with PCOS, 0 (0%) psoriasis patients without PCOS and in 1 (2.5%) control women and the difference was significant (P-value=0.006).Prolactin was found to be elevated in 2 (20%) psoriasis patients with PCOS, 2 (3.3%) psoriasis patients without PCOS and in 1 (2.5%) control women and the difference was significant (P-value=0.04).Evaluation of psoriasis and its connection to the presence and absence of PCOS is evaluated. The psoriasis group is weighed according to severity, risk factors and the diagnosis of PCOS depending on Rotterdam criteria; mean duration of psoriasis was 9.1 years in the psoriasis group who met PCOS criteria and 7.89 years in those who didn’t. (P-value=0.75). Both psoriasis with PCOS and psoriasis without PCOS patients had 30% family history of psoriasis. Regarding the severity of psoriasis; PASI score > 10 found in 9 (90%) in psoriasis with PCOS group and 14 (23%) in the psoriasis without PCOS (p-value=0.0001). Fifty percent of psoriasis with PCOS has impaired glucose tolerance test compared to (11.6%) in the psoriasis with no PCOS (p-value=0.002) (Table 2). Fifty percent of psoriasis patients with PCOS had hypertension >130\85 paralleled to (21.6%) in psoriasis without PCOS (p-value=0.05).
|
|
|
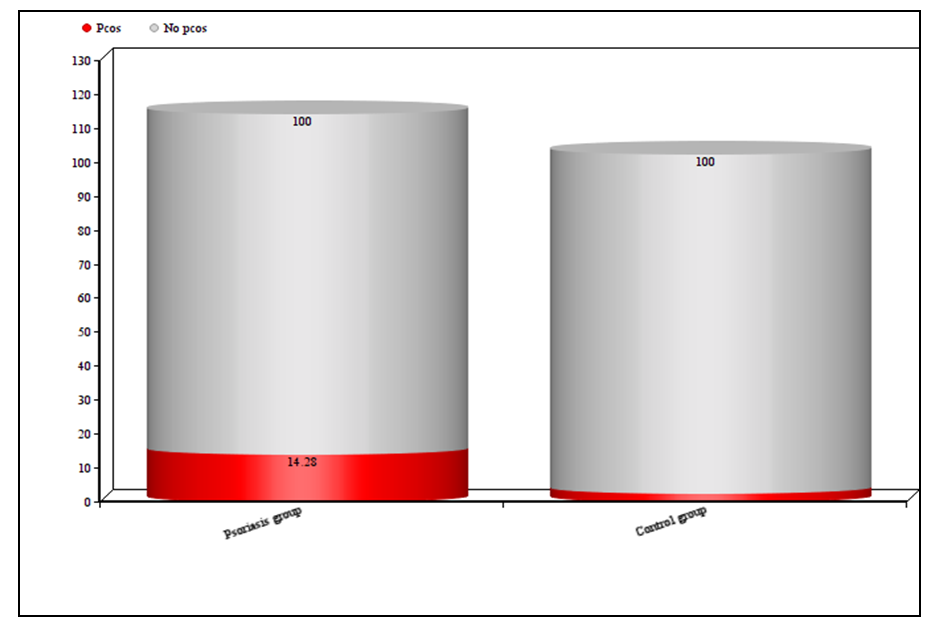 | Figure 1. Prevalent risk of PCOS in psoriasis and control groups |
4. Discussion
- Polycystic ovary syndrome is not uncommon endocrine disturbance of females in reproductive age. It displays many features like chronic anovulation, infertility, and hyperandrogenism, acne, hirsuitism, androgenic alopecia etc… It was noticed that most affected women exhibit a certain body habitus as they tend to present with central obesity due to hyperandrogenemia and impaired glucose tolerance test in coincidence with longer-term health consequences of PCOS have been recognized [12].The relationship between both PCOS and psoriasis haven't been studied much and a little information had been published regarding their coexistence [13].The common trail that bonds psoriasis to PCOS is not well-known precisely, but there are studies supporting this relationship. In a study performed by Moro et al, showed that in patients with psoriasis the prevalence of PCOS was significantly greater "47%" than in age matched women in the control group [14].Even though the etiology of PCOS is still not quietly known, evolving data suggest that insulin resistance could play an important role in the development and the pathophysiology of this syndrome and may also contribute to the PCOS-related increase of cardiovascular complications. This strong association between PCOS and psoriasis could be a consequent to the fact that both diseases havesimilar metabolic comorbidities such as impaired glucose tolerance test increase, risk for oxidative stress, inflammationand increased cardiovascular risk [15].Correspondingly, compared with healthy control, women with psoriasis are more frequently affected by impaired glucose tolerance test; fasting blood glucose was elevated in 11(15.7%) in psoriasis group and only 4(10%) in the healthy control. This result is in agreement with study performed by Ucak et al which is showed that psoriatic patients had more insulin resistant than healthy subjects [16]. Moro et al also assessed level of glycaemia, insulin resistance in both psoriasis and control group and the result and p-value was significant suggesting impaired GTT and insulin resistance in psoriasis which is one of metabolic syndrome diagnostic pillars [14].Assessment of early onset cardiovascular complications such as ischemic heart diseases and hypertension is higher in the psoriasis group than in the control group. This is especially observed in patients with both PCOS and psoriasis than psoriasis without PCOS group. Cardiovascular derangements could contribute to "3 to 4 years" reduction in life expectancy among patients with severe psoriasis [17].The prevalence of metabolic syndrome is at least two times in psoriatic patients compared with non-psoriatic control [18]. Increase adipose tissue contributes to increase secretion of cytokines and hormones i.e. both psoriasis and PCOS patients are more liable to develop obesity, and it is speculated that adipose tissue delivers cytokines that trigger PCOS in psoriatic patients and vice versa [19].Psoriasis patients with PCOS have more patients with PASI score >10 in addition to more risk of associated diseases like impaired glucose tolerance test and hypertension than psoriasis patients without PCOS. In a study by Maluki et al found that metabolic derangement was found to be associated to the severity of psoriasis; Obesity, dyslipidemia was statistically significant in patients with severe psoriasis [20].Psoriasis severity may be attributed to the fact that it’s a disease affected by hormonal variations during puberty, postpartum, and menopause. Androgens are steroid structural hormones responsible for male features. PCOS is a hyperandrogenic state thus it may be participate to enhancing psoriasis severity [21].
5. Conclusions
- The incidence of PCOS in women with psoriasis is higher than in control women, this association makes psoriasis patients with PCOS more suspecitible to hormonal disturbances, metabolic derangement including impaired glucose tolerance test and higher PASI score. Psoriasis patients have higher BMI, WHR and blood pressure than control patients.
Disclosure
- This study was an independent study and not funded by any of the drug companies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML