-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(4): 47-50
doi:10.5923/j.ajdv.20200904.01
Received: Jul. 27, 2020; Accepted: Aug. 23, 2020; Published: Sep. 15, 2020

Lichen Planus in Iraqi Patients (Clinical – Descriptive Study)
Basman M. Fadheel1, Jameela B. Meseeck2
1Iraqi Board for Medical Specialiazation, Baghdad, Iraq
2Dermatology Center, Medical City Teaching Hospital, Baghdad, Iraq
Correspondence to: Jameela B. Meseeck, Dermatology Center, Medical City Teaching Hospital, Baghdad, Iraq.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: lichen planus is an idiopathic inflammatory and immune mediated disease that effect skin, nail, hair and mucous membrane, mostly affect middle age people, with chronic course with relapses and periods of remissions. Objective: To assess various aspects about cutaneous LP in Iraqi patients. Its clinical subtypes and its correlations with mucosal, nail, scalp involvement, and gender, age distribution. Patients and methods: This observational study was carried out at the center of Dermatology and Venereology - Baghdad Teaching Hospital, from the first of April 2018 to the first of April 2019. 158 patients with cutaneous lichen planus were included in this study. Detailed history and thorough physical examination had been done for all patients. Results: The sample include 158 patients, there were 76 male and 82 female. The age ranged of males at presentation was from 7 to 70 years with a mean ± SD ═ 38.14 ±16.96, in females the age range at presentation between 17 to 65 with a mean ± SD ═ 45.06 ± 12.65. The disease duration ranged from two weeks to 5 years. the most common type was classical type (74%), the second was actinic type (10%). most common sites were lower limb, upper limb, face. Conclusions: Lichen planus is a disease of middle aged patients, 68% of patients were of the age group between 31 to 60 years. In classical type there is obvious female predominance, while in actinic type male predominate the picture. The most common site in Lichen planus pigmentosus are the axillae and groin. Oral involvement mostly seen in middle age female, most common type was the reticular and most common site was the buccul. Nail involvement mostly seen in young male, the most common type was 20 nail dystrophy, Follicular involvement mostly seen in male. Genital involvement mostly seen in women and mostly of reticular type.
Keywords: Lichen planus
Cite this paper: Basman M. Fadheel, Jameela B. Meseeck, Lichen Planus in Iraqi Patients (Clinical – Descriptive Study), American Journal of Dermatology and Venereology, Vol. 9 No. 4, 2020, pp. 47-50. doi: 10.5923/j.ajdv.20200904.01.
1. Introduction
- Lichen planus (LP), the most typical and best characterized lichenoid dematosis, is an idiopathic inflammatory skin disease affecting the skin and mucosal membranes, often with a chronic course with relapses and periods of remission. LP most commonly has its onset during the fifth or sixth decade. Both T lymphocyte and keratinocytes play role in development of LP lesions. Genetic factors [1], hepatitis C virus and many drugs has been linked with cutaneous eruptions similar or identical to LP [2]. In lichen planus the characteristic primary lesion is a small, polygonal-shaped, violaceous, flat-topped papule. The surface is slightly shiny or transparent, and a network of fine white lines called “Wickham striae”. Postinflammatory hyperpigmentation is also a common finding. LP is usually pruritic, mostly occur on flexor wrists and forearms, the dorsal hands, the shins, and the presacral area. Mucous membranes, especially the oral mucosa, are affected in more than half of patients. Other clinical variants of LP exist like linear LP which occur spontaneously within the lines of Blaschko. [3] Annular LP Men represent 90% of patients with annular Lp. Mostly involve axilla and penis [4]. Hypertrophic LP mostly involve pretibial area and ankles. They are extremely pruritic and more chronic in nature than classic LP lesions, malignant transformation to squamous cell carcinoma (SCC) has been documented [5]. Inverse lichen planus appear in intertrigenous zones [6]. Aim of the study is to evaluate epidemiological and various clinical aspects of lichen planus in Iraqi patients…
2. Patients and Methods
- This is a descriptive clinical study that was conducted in Center of Dermatology and Venereology, Baghdad Teaching Hospital in a period from April 2018 to April 2019. A verbal consent from all patients included in this study was taken; after full explanation about the nature of the study. The ethical approval was given by the Scientific Committee of Scientific Council of Dermatology and Venereology –Iraqi Board for Medical Specializations. A total of 158 Lichen planus patients were enrolled in this study. History was taken regarding age, duration of disease, occupation and drug history. Thorough physical examination were carried out in order to determine the clinical types of lichen planus, distribution of the lesions, nail, mucosal, scalp involvement. Inclusion criteria involve all patients with cutaneous lichen planus. Exclusion criteria involve those patients who have only mucosal, scalp or nail LP without skin lesion and those taking drugs causing LP. Diagnosis made on clinical bases. Medical photographic documentation of the lesion sites was done by using Samsung Galaxy S9-12megapixel digital camera in the same place and illumination.
3. Results
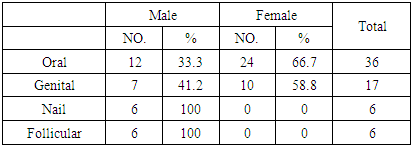
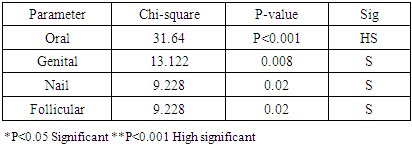
- A total of 158 cases of cutaneous LP were enrolled in this study, the diagnosis were made on clinical bases. The sample include 76 males (48. 10%) and 82 (54.43%) females, the females to males ratio is (1.07:1). The age ranged of males at presentation was from 7 to 70 years with a mean ± SD = 38.14 ±16.96 years and median of 35 years, in females the age range at presentation between 17 to 65 with a mean ± SD = 45.06 ± 12.65 years with median of 45 years. Most common age groups involved were those between 31 to 60 years. Eighty six patients were of this age group, comprising (54.8%) of the sample. Out of 158, 118 (74.6%) cases were of classical type of LP, 17 ( 10.7 %) were of LP actinicus, 10 (6.3%) cases of hypertrophic LP and 7 (4.4%) cases of Lichen planus pigmentosus, atrophic type 2 cases (1.26%), inverse type 2 cases (1.26%), annular and eruptive 1 case (0.54%) for each. In classical type 47 (39.8%) male, female 71 (60.1%). Actinicus type there were 12 male (70.5%), 5 female (29.4%), hypertrophic type 8 male (80%) and 2 female (20%), lichen planus pigmentosus 4 male (57.1%) and 3 female (42.8%). Age of patients range between 7 to 70 years, 64% of patients were above 40 years, more details in table (1).
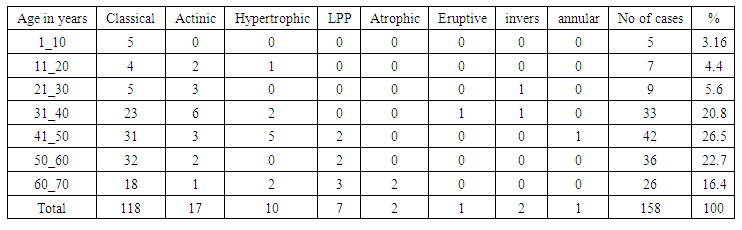 | Table 1. Age distribution of different clinical types of Lichen |
 | Figure 1. A forty four years old male show classical Lichen Planus |
 | Figure 2. A forty two year male showing twenty nail |
 | Figure 3. Sixty five years old male show Lichen Planus Pigmentosus on axilla |
 | Figure 4. A ten years male showing hypertrophic lichen planus |
 | Figure 5. A thirty eight years old male develope verocus SCC on lesion of hypertroohic Lichen |
|
|
4. Discussion
- The present study describes the details of epidemiological and clinical characteristics of LP in Iraqi patients. In this study the most common affected age group were those between 31 to 60 years who comprise about 54.4 % of the sample, this finding correlate with other studies that show high occurrence of LP in middle age people. It has been stated that Lichen planus has a very limited frequency in children, this also correlates with our findings children who are less than 10 years comprise less than 3% of the sample It had been recorded that LP preferentially affect females however in this study there is no significant sex predilection, females 52%, males 48% of the sample. In this study the classical LP was the most common type, constituting 74.6% of the sample. This finding is consistent with finding of most of the studies [6]. Most cases of classical LP were female 67.6%, although it had been recorded in all age groups but it was more prevalent in middle age and elderly, in this study the lower limbs were the most common site of involvement in classical LP 75%. The second most common site involved in classical LP were the upper limbs (43.7%). Actinic LP was the second most common type of LP seen in 10.7% of our sample, 64.2% were males, higher prevalence of actinic LP in males. The face was the most common site of involvement 100% of cases, followed by neck 70%, dorsal hands and forearms 17.64% and this correlate with other studies [7] In this study hypertrophic type comprise 6.3% of the sample, there were significant male predominance 80%, it was most common in middle age above 40 years (75%) and this correlate other studies, most common sites were the anterior legs and dorsum of feet. The long duration for this type and sever itching may explained the malignant potential that have been recorded with it. Lichen planus pigmentosus comprise 4.4% of sample, it usually affect Indians and darker skinned individuals in whom the most common sites of involvement are sun exposed parts, in our study the most common sites were the axilla and groins (100%), and this compatible with usual findings in lighter skinned Asians, which typically affects the intertrigenous and flexural areas. Oral involvement with skin lesions seen in 14% of the sample which are consistent with reported involvement of mucous membrane in 15-20%. Women outnumber men (ratio f: m=2:1) and this correlates with findings of other studies [8]. In this study oral LP more prevalent in 6th decade, mean age 52 years. The most common site was the buccle 83.3% followed by the tongue 33.3% and lips 13.8%, gingiva and hard palate involved in less frequency, this finding of dominance involvement of buccle is concordance with other studies. Most common subtype was the reticular 94%, plaque type 30%, erosive 11% this is similar to other studies found reticulate pattern being the common presentation [9]. Nail involvement were 3.7% and this is comparatively low as compared with reported nail involvements in LP that range between 5 to 10% [10]. All patients were males, and as reported in other studies. 66.6% of patients were young less than 20 years old. Genital involvement seen in 10.7% of cases. it was more common in middle age females (F:M ratio 3:1) it mostly affect peri or post menopausal women with mean age 47 years, in men genital lesion occur in younger age group mean age 31 year [11]. In females the most common site was the labia minora (100%), the most common type was the reticular type (83%), erosive type (16.3%). In male the most common site was the glans (100%), the most common type was the reticular ((100%). Follicular involvement recorded in 3.7% of cases. Hair involvement seen exclusively in older male age more than 50 years, those patients present with patches of cicatercial alopecia of the scalp.
5. Conclusions
- Lichen planus is a disease of middle aged patient, 68% of patients were of the age group between 31 to 60 years. In classical type there is obvious female predominance, while in actinic type male predominate the picture. The most common site in Lichen planus pigmentosus are the axillae and groin. Oral involvement mostly seen in middle age female, most common type was the reticular and most common site was the buccul. Nail involvement mostly seen in young male, the most common type was 20 nail dystrophy, Follicular involvement mostly seen in male.Genital involvement mostly seen in women and mostly of reticular type.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML