-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(3): 43-46
doi:10.5923/j.ajdv.20200903.03
Received: August 2, 2020; Accepted: August 20, 2020; Published: August 29, 2020

Metabolic Syndrome in Iraqi Patients with Vitiligo
Hussam Ali Salman1, Suroor Rafea Abdulkareem2
1Iraqi Board for Medical Specializations, Baghdad, Iraq
2Dermatology Center, Medical City, Baghdad, Iraq
Correspondence to: Suroor Rafea Abdulkareem, Dermatology Center, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

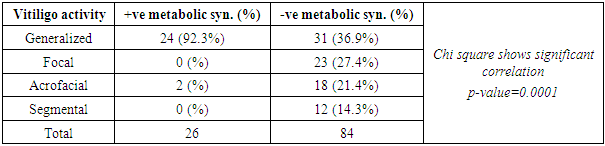
Background: Metabolic syndrome (MS) is a complex of interrelated risk factors for cardiovascular diseases, diabetes mellitus, and stroke. Those factors include; abdominal obesity, dyslipidemia, glucose intolerance, and hypertension. Vitiligo is an acquired depigmenting disease with multifactorial etiology. However, there is a growing evidence that Vitiligo not only affect the skin but it may also related to systemic metabolic abnormalities. Objective: To investigate the association between metabolic syndrome and Vitiligo. Patients and methods: The present study was a case control study, carried out on 110 Vitiligo patients and 131 age matched and sex matched healthy control. Metabolic syndrome and its components including (abdominal circumference, serum triglyceride, high density lipoprotein level, blood pressure and fasting blood glucose) were compared between cases and control. Detailed history was taken from each participant and physical examination was done for all. Results: the present study was found that the percentage of metabolic syndrome in Vitiligo patients was 26 (23.6%) and in control group was 24(18.3%) (p-value = 0.3). Age of patient may also carry more risk of metabolic syndrome; older individuals show significant increase in metabolic syndrome p-value 0.04. Regarding the clinical type of Vitiligo, we found that generalized type of Vitiligo carries more risk 24(92%) of them develop metabolic syndrome. Active Vitiligo shows significant correlation with metabolic syndrome 21(60%) p-value 0.0001. This study also revealed that increase body surface area increase risk of metabolic syndrome (p-value 0.0001). Conclusion: Several factors might collaborate, to increase incidence of metabolic syndrome in Vitiligo patients (increase body surface area, activity of Vitiligo, generalized type of Vitiligo, increase age of patient). These factors, may make Vitiligo patient more susceptible to develop metabolic syndrome.
Keywords: Vitiligo, Metabolic Syndrome
Cite this paper: Hussam Ali Salman, Suroor Rafea Abdulkareem, Metabolic Syndrome in Iraqi Patients with Vitiligo, American Journal of Dermatology and Venereology, Vol. 9 No. 3, 2020, pp. 43-46. doi: 10.5923/j.ajdv.20200903.03.
Article Outline
1. Introduction
- Vitiligo, an acquired skin disease of progressive melanocyte loss, is clinically characterized by well-defined milky-white macules that may also include white hairs, or poliosis. [1] is an autoimmune disease of the skin in which CD8+ T cells target melanocytes and destroy them, leaving areas without pigment production, which is clinically manifest as white macules and patches. The pathogenesis has been debated for many years, with multiple hypotheses offered as alternative explanations as to what lies at the root of the disease. These alternative hypotheses include cellular stress causing degeneration of melanocytes, chemical toxicity causing melanocyte death, and neural changes that influence melanocytes or their ability to produce melanin. [1]Metabolic syndrome (MetS) is a composite of risk factors. In 2001, the National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP) III published their criteria for diagnosing MeTS. It is a simpler and easier to use definition. Five criteria were specified: abdominal obesity, estimated by an increased waist circumference, high TG and low HDL concentrations, elevated BP, and glucose intolerance. Presence of any three of the above criteria is considered compatible with a MeTS diagnosis. [2]TNF-α, IL-6, IL-1, are among the proinflammatory cytokines that play a role in the pathogenesis of Vitiligo and are also associated with insulin resistance, atherosclerosis, and other metabolic complications. The presence of these proinflammatory cytokines may support the association of Vitiligo with MetS. An alternate hypothesis is that Vitiligo and metabolic syndrome have a similar pathogenesis, in Vitiligo lipid peroxidation causes a deterioration of reactive oxygen species, which cause a reduction of melanocytes in adipose Tissue. The Reduced Melanocytes Are Posited As A Possible factor for the co-occurrence of MetS. [3]
2. Patients and Methods
- This case control study was conducted on Vitiligo patients attending the outpatient clinic of dermatology center, medical city In Baghdad/Iraq from the beginning of May 2018 till the end of July 2019.One hundred and ten (110) Vitiligo patients and 131 control, the control group included age matched and sex matched volunteers who had no history of dermatologic or systemic diseases.Informed consent was, obtained from each participant, before enrollment.Inclusion and exclusion criteria:Inclusion criteria were: older than 15 years, no systemic or local therapy 3 months before beginning of the study.Exclusion criteria were: age below 15years, Vitiligo lasting for less than 6 months, alcoholic and smokers, psoriasis, rheumatoid arthritis, chronic obstructive lung diseases, thyroid diseases, autoimmune diseases, liver diseases, malignancy, users of immunosuppressive or systemic corticosteroids, infections, pregnancy, lactation, and women use hormone replacement therapy.All participants were subjected to the following:Detailed history with regard to age, gender, occupation, marital status, special habits, and drug intake. Vitiligo history include: onset, course, duration, progression, characteristics, associated medical or surgical conditions, family history of Vitiligo, diabetes and cardiovascular diseases.General examination: height, weight, body mass index, blood pressure, waist circumference of participant was obtained. Waist circumference was measured as the smallest trunk circumference midway between the lowest rib margin (12th rib) and the iliac crest at the end of gentle expiration. The measurements were performed with the patients in standing position with a relaxed abdomen, arms at sides, and their feet joined together, ensuring that the tape measure was horizontal and did not cause skin compression.Dermatologic examination: examination of skin, hair, nails and oral mucosa was carried out.The percentage of Vitiligo involvement: is calculated in term of hand units. One hand unit (which encompasses the palm plus the volar surface of all digits) is approximately equivalent to 1% of total body surface area, (BSA). [4]Disease activity: [5]Stable Vitiligo defines as patient, reporting no new lesions, no progression of existing lesions, and absence of Koebner, phenomenon during the past 1-year, active Vitiligo was defined as development of new lesions and/or progression of existing lesions, or positive Koebner phenomenon.Types of Vitiligo: [6]According to Bordeaux Vitiligo global issues consensus conference classification:• Non segmental: Acrofacial, Mucosal (more than one mucosal site), Generalized, Universal, Mixed. • Segmental Vitiligo: Uni-, bi-, or plurisegmental.• Undetermined/unclassified Vitiligo: Focal, Mucosal (one site in isolation).Laboratory investigations:Glycemic index, high density lipoprotein (HDL) and triglycerides (TG), the metabolic syndrome criteria were defined by the current American Heart. Association and the National Heart Lung and Blood Institute in 2005, According to the NCEP ATP III definition, metabolic syndrome is present if three, or more of the following five criteria are; waist circumference over, 102cm (men) or 88 cm (women), blood pressure over, 130/85 mmHg, fasting triglyceride level over 150 mg/dl, fasting high-density lipoprotein cholesterol level less than 40 mg/dl (men) or 50 mg/dl (women) and fasting blood, sugar over 100 mg/dl. [7]Statistical analysis Data entered using computerized statistical software; Statistical Package for Social Sciences (SPSS) version 22 was used. Descriptive statistic presented as (mean +/- standard deviation) and frequencies as percentages. p-value of less than 0.05 was considered statistically significant.
3. Results
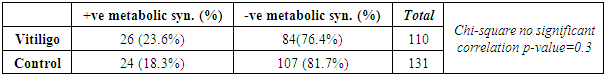
- This study was carried out on 110 Vitiligo patients and 131 age matched and sex matched control. In Comparison between the control group and Vitiligo group in term of presence and absence of metabolic syndrome; (26) 23.6% of Vitiligo patients were diagnosed with metabolic syndrome while (24) 18.3% was diagnosed in the control group, however the Comparison using chi square wasn’t significant between the two groups as (p-value= 0.3) Table (1).
|
|
|
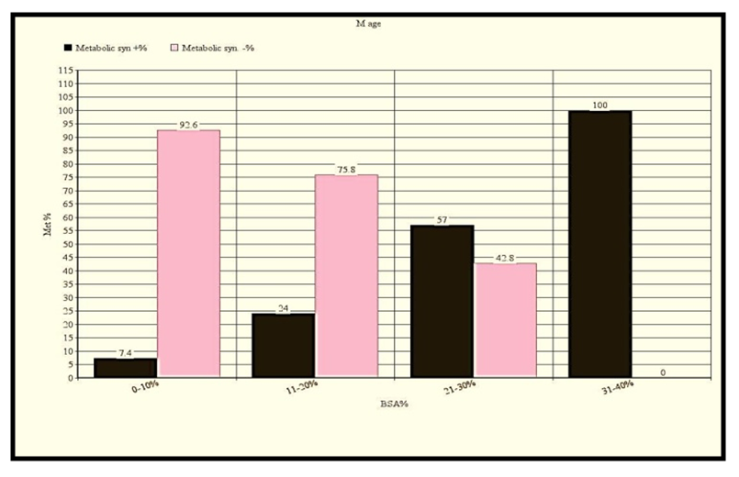 | Figure (1). Relationship between metabolic syndrome and BSA% |
|
|
4. Discussion
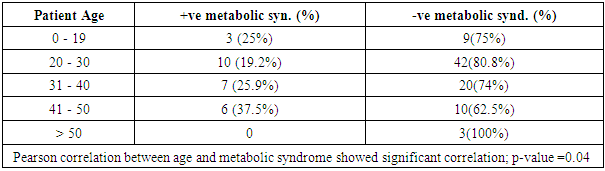
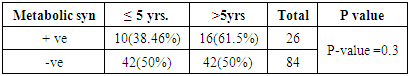
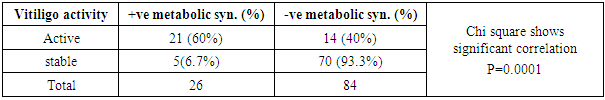
- Vitiligo is a common autoimmune skin condition. Pathogenesis of Vitiligo is still largely unknown and several theories have been proposed such as changes in the cytokine profiles, genetic factors, melanocyte abnormality and destruction and stress can contribute to the beginning of Vitiligo. [8]Vitiligo is not a skin limited disease since the mechanisms that have supposed to elicit it can attack other systems therefore, there may be metabolic disturbances in cases of Vitiligo.The erratic metabolic profiles, a feature shared with & contribute to the development of Metabolic syndrome through complicated mechanisms involving many systems such as insulin resistance, lipid profile disturbances. Generally, researches that study the relationship between Vitiligo and metabolic syndrome in the literature are uncommon. [9]This study attempts to find out the prevalence of metabolic disturbance in Vitiligo patient and to find out whether there are risk association within different Vitiligo patients. This study showed that Metabolic syndrome presented in both cases of Vitiligo (23.6%) and in the controls (18.3%), (p-value =0.3 which wasn't significant) table (1).In a study by P. K. Sinha et al, there wasn’t significant difference in waist circumference, plasma glucose and blood pressure between cases and controls. however, in a study performed by Hatice et al revealed that metabolic syndrome was more prevalence in Vitiligo patient than control. [10]Age of the patient might also carry more risk of metabolic syndrome, older patient of both Vitiligo and control have higher risk of metabolic syndrome (p-value = 0.04) (table 2). age alone might not be enough as a sole factor for developing metabolic syndrome in vitiligo patients. however, older patient of vitiligo likely has longer history of the disease i.e. longer duration and naturally carry more risk of metabolic syndrome than patient with shorter duration of the disease, so the duration of the disease might be more important than the patient age. the same fact was suggested in a study done by University of Health Science in turkey. [10]Relatively short Vitiligo history (the mean is 7 years duration) may explain the statistically insignificant differences in metabolic syndrome risks between the studied and control groups table (3).A significant correlation was found between metabolic syndrome and disease activity (p- value= 0.0001) (table 4). similar findings found in the study of Hatice. [10] Clinical types of Vitiligo; generalize, focal, acrofacial and segmental show significant difference in metabolic syndrome were; generalize type is 92% followed by acrofacial (7.7%) table (5). in our study segmental type showed no increase in metabolic syndrome contrary to previous studies such as the one suggested by Hatice et al [10] in which segmental type was a head of others in term of metabolic syndrome occurrence and regarded as independent risk factor for metabolic syndrome in Vitiligo patient. That might be attributed to the shorter duration for Vitiligo of all cases (mean of 7 years) and fewer cases in our study or lesser activity of the disease.A significant correlation was found between the percentage of body surface (BSA%) and metabolic syndrome (p-value=0.0001) figure (1) in agreement to study performed by Y.K. Sharma et al. [11]
5. Conclusions
- 1- In the present study we found, that several factors might collaborate to induce metabolic syndrome in Vitiligo patients (increase body surface area, active Vitiligo, generalized type of Vitiligo, increase age of patient) these factors may make Vitiligo patients more susceptible to development of metabolic syndrome and it’s complications like cardiovascular diseases.2- There were no significant differences in the prevalence of metabolic syndrome between Vitiligo and control group.3- There were no significant correlation between duration of Vitiligo and metabolic syndrome.4- There were no significant correlation between gender of Vitiligo patient and metabolic syndrome.5- We need further larger population-based study to establish the relationship between vitiligo and metabolic syndrome with concentration on environmental, genetic and immunological factors leading to their co-occurrence.
Disclosure
- This study was an independent study and not funded by any of the drug companies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML