-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(2): 17-20
doi:10.5923/j.ajdv.20200902.01

Efficacy of Voriconazole among 500 Dermatophytes Patients: A Study in a Tertiary Care Hospital, Cumilla, Bangladesh
Hoq AJMS1, Sultana F.2, MJ Abedin1, GM Matiur Rahman1
1Assistant Professor, Dept. of Dermatology and Venereology, Cumilla Medical College Hospital, Cumilla, Bangladesh
2Emergency Medical Officer (EMO), Mymensingh Medical College Hospital, Mymensingh, Bangladesh
Correspondence to: Hoq AJMS, Assistant Professor, Dept. of Dermatology and Venereology, Cumilla Medical College Hospital, Cumilla, Bangladesh.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Dermatophytosis is a major health related problem in areas with high humidity, overpopulation and poor hygienic conditions. Treatment options are topical as well as systemic antifungal drugs. But during course of time dermatophytes have also evolved drug resistance for single as well as multiple drugs simultaneously. Therefore, it became necessary to find out antifungal susceptibility for dermatophytes. In this study, we included 500 patients of all age group with clinical diagnosis of dermatophytosis. To find out antifungal resistance pattern and efficacy of Voriconazole among dermatophytes. (Skin, hair and nail samples were taken aseptically. Some patients were resistant against present treatment options like: fluconazole, itraconazole & terbinafine etc.) All patients were treated with Voriconazole (Voricon used as a Voriconazole which was from a renowned pharmaceuticalin Bangladesh name General pharmaceutical limited. Duration of treatment of each patient was 12 weeks. Resistance against fluconazole and terbinafine was most common, 85.33% and 58% respectively. No resistance against voriconazole was observed in this study. Resistance against fluconazole was noted among all species of dermatophytes, followed by terbinafine. fluconazole was least effective drug followed by terbinafine. Among 500 patients 88% was fully cured and rest of 12 % were partially cured with Voriconazole.
Keywords: Dermatophytes, Antifungal, Efficacy, Voriconazole
Cite this paper: Hoq AJMS, Sultana F., MJ Abedin, GM Matiur Rahman, Efficacy of Voriconazole among 500 Dermatophytes Patients: A Study in a Tertiary Care Hospital, Cumilla, Bangladesh, American Journal of Dermatology and Venereology, Vol. 9 No. 2, 2020, pp. 17-20. doi: 10.5923/j.ajdv.20200902.01.
Article Outline
1. Introduction
- Dermatophytes are filamentous fungi that are able to digest and obtain nutrients from keratin, primarily a component of skin hair and nails. Cutaneous mycoses are mostly caused by keratinophilic filamentous fungi called dermatophytes and are classified into three genera: Trichophyton, Microsporum and Epidermophyton. So far, about 30 species of dermatophytes have been identified as human pathogens. [1] Although infections caused by dermatophytes are generally limited to the surface regions of the skin, these fungi can behave as invasive, causing deeper and disseminated infection, especially in immunocompromised patients. [2] World Health Organization estimates dermatophytes affect about 25% of the world population. [3] Anthropophilic dermatophytes are associated with humans and rarely infect animals. Zoophilic dermatophytes cause infection in animals and may infect humans who come in contact. Geophilic dermatophytes are generally found in soil and take part in decomposition of hair, nails, feathers and horns. [4] When the organism grows on the host, living tissue is not usually invaded. The organism simply colonizes in the keratinized outermost layer of skin. The disease is known as tinea or ringworm. It is the result of the host reaction to the enzymes released by the fungus during its digestive process. Dermatophytes are the only fungi that have evolved a dependency on human or animal for the survival of the species. It is therefore, these fungi are among the most common infectious agents. [5] The most common dermatophytes that cause cutaneous mycoses are Trichophyton rubrum, Trichophyton mentagrophytes, Microsporum canis and Trichophyton tonsurans. [6] The tinea infections are prevalent worldwide but they are common in geographical areas with higher humidity. Over population and poor hygienic living conditions also contribute to dermatophytic infections. Hot and humid climate of Bangladesh makes dermatophytosis a very common superficial fungal infection of skin. [7] In recent years, the number of human infections caused by this group of fungi has increased considerably and is of particular concern in immune compromised patients. [8] Studies conducted show that resistance among dermatophytes is not uncommon and fluconazole to be most resistant and voriconazole to be most sensitive drug for dermatophytes. Some investigators reported that the disease pattern of fungal infections varies among the different countries and different areas within the same country. [9,10] Due to high temperature and increased humidity, there are increased cases of dermatophytosis and other fungal infections especially in Bangladesh. There was increased incidence of drug resistance observed over a period of time to the antimycotic drugs commonly used for the treatment i.e. fluconazole, itraconazole and terbinafine. Therefore, this study was carried out to find out incidence of dermatophytes infection as well as prevalence of drug resistance and the efficacy of Voriconazole to superficial fungal infection.
2. Objectives
- General Objective: • To evaluate the treatment modalities of tinea infections in Bangladesh Specific Objective: • To find out the role of voriconazole in different tinea infections in Bangladesh
3. Materials and Method
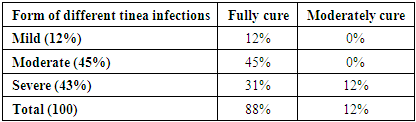
- Out of total tinea infected patients we selected only those patients who didn’t respond to routine treatment, relapsed soon after stoppage of treatment or those having persistent dermatophytic infection. A total of five hundred patients of all age group and both sexes attending skin outpatient department were recruited into the study. The interventional study was carried out for a period of total 9month from August 2018 to April 2019 in the OPD at CumillaMedical College & Hospital, Cumilla, Bangladesh. Total hundred patients of tinea infections were selected considering exclusion criteria like patients with known hypersensitivity to any ingredients of Voriconazole, Pregnancy/lactation, impaired hepatic function, impaired renal function and severe systemic illness. All the clinically suspected 500 cases were subjected to mycological work up. Purposive type non-probability sampling technique was followed in this study. After collection of data, these were screened by checking consistency, edited and were finally analyzed by software SPSS (Statistical Package for Social Science) method.Procedure of TreatmentThe patient of tinea infections was identified first. The diagnosis was made on the clinical basis by assessing morphology of lesions, age of onset and their distribution sites. To reach a clinical diagnosis, detailed history and thorough physical examination done. Then clinical conditions of the patient were recorded along with hematological and biochemical profile, like blood for total count, differential count, ESR, platelet count, random blood sugar, serum for ALT and serum creatinine level. Finally, all patients with tinea infections were treated by oral Voriconazole 200 mg (available as Voricon 200mg tab) twice daily for 4 weeks. The cases were divided as mild from (itching, red and flaky skin), moderate form (moderate itching, thick, oily and yellow) and severe from (extensive itching, inflamed skin) and patient’s subjective assessment of pruritus and burning sensation were evaluated before and after treatment. A final medical assessment of efficacy is made at the end of the treatment period using a four -point scale (categories: Fully cure 88%, moderately cure 12%) and the assessment result is recorded and analyzed to prepare the final result. Follow up were done at the end of 2nd, 4th, 8th, & 12th week.
4. Results
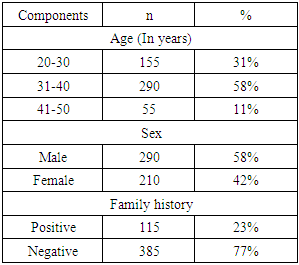
- The study was carried out for a period of total 9 month from August 2018 to April 2019 in the OPD at Cumilla medical college & Hospital. Total five hundred patients of tinea infections were selected. Among them, 31-40 years age group was 58%, 20-30 years was 31%- and 41-50-years age group was 11%, regarding sex, (58%) males and (42%) females between 20-50 years aged patients with tinea infections and regarding family history, (23%) had positive family history and (77%) had negative family history of tinea infections (Table 1). Regarding occupation among the patients, 50% were outdoor worker, 38% were involved in indoor service and rest 12% involved in other occupation (Figure 1).
|
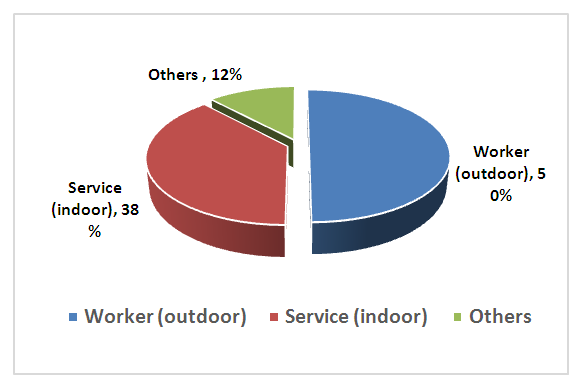 | Figure 1. Distribution of patients according to occupation |
5. Discussion
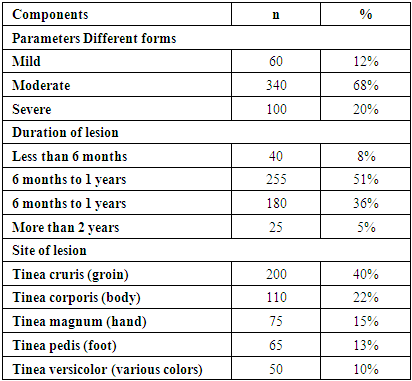
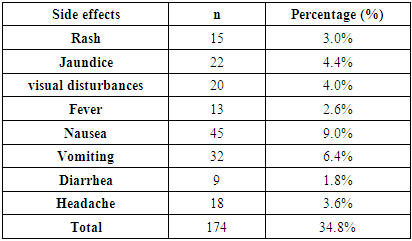
- The study was carried out for a period of total 9from August 2018 to April 2019 in the OPD at Cumilla Medical College & Hospital, Cumilla, Bangladesh. Total fivehundred patients of different tinea infections were selected. In table 1: 31% patients were 20-30 age group, whereas most of them 58% were 31-40 age group and 11% were 41-50 age group. 58% were male and rest of 42% were female. Another factor 23% patients had positive family history whereas 77% negative. In figure 1: regarding occupation among the patients, 50% were outdoor worker, 38% were involved in indoor service and rest 12% involved in other occupation. Among the five hundred patients of different tinea infections in table 2, mild form was 12%, moderate was 62% and severe was 20%. Regarding duration of lesions, highest patients of different tinea infections 51% had the duration 6 month to 1 years and next 36% had the duration 1 to 2 years. Regarding site of lesions, maximum patients of different tinea infections 40% had involvement of groin, next 22% had involvement in the body, 15% had involvement in hand, 13% & 10% are respectively foot and others etc. Table 3: showed that 88% patients of different tinea infections had fully cure, only 12% moderately cure. 12% severe patients were moderately cure and they need to increase the duration. Table 4: showed that only 34.8 % seen with side-effect like rash 3.0%, jaundice 4.4%, visual disturbance 4.0%, fever 2.6%, nausea 9.0%, vomiting 6.4%, diarrhea 1.8%, and headache 3.6% which was not significant. Nobody had discontinued therapy for side effects and not required any additional treatment for side effect. Fifty percent of total patients are outdoor worker used to exposure in sunlight and hot humid climate for their nature of occupation. This reflects the precipitating factor of tinea infections. The study showed that 88% patients of different tinea infections had very good response, 12% patients were moderately cure of tinea infections. The efficacy of oral antifungals was attributable to their antifungal and/or anti-inflammatory effects by Gupta, Nicol and Batra 8. At present, systemic use of fluconazole, ketoconazole, itraconazole, and terbinafine has been associated with very low clinical response in the treatment of different tinea infections because of their narrow spectrum as well as high resistance rate. However, the efficacy of oral voriconazole which was highly effective against a greater spectrum of dermatophytes causes tinea infections and showed marked improvement. In one study, oral voriconazole 200 mg twice daily for 4 weeks. This dosage was chosen because it has been used effectively and safely in the treatment of different tinea infections. The study showed (Figure 2) showed that improvement of fully cure group is 38% observed and moderately cure group 27% improvement on the 1st follow up visit at the 2nd week. On the 2nd follow up visit at 4th week, 75% cure of fully cure group and 53% cure of moderately cure group. Then 88% cure of fully cure group as well as 78% moderately cure group at 3rd week, at 4th week 100% cure found in fully cure group and 98% observed in moderately cure group. The safety profile of voriconazole when used on a long-term basis, its efficacy against dermatophytes causes tinea infections, make voriconazole an excellent therapeutic option in different superficial fungal infections and treatment of choice in ‘recalcitrant cases’ of tinea infections. Nobody had discontinued therapy for side effects and not required any additional treatment for side effect. Our study had several limitations. First, no fungal culture was performed and the clinical outcome could not therefore be correlated with Malassezia yeast colonization. Consequently, a possible anti-inflammatory effect of voriconazole could not be evaluated. In addition, the self-remitting course of the disease, the number of patients and the duration of treatment in this study may have been insufficient to evaluate drug-related improvement. The current study was an attempt to develop a short, convenient, and safe treatment protocol, which is strongly needed for different tinea infections. The results of this study indicate that voriconazoleis a suitable treatment for the patients of different superficial fungal infections like tinea and others. However, larger studies using different dosages and durations of therapy may provide a rationale for systemic use of voriconazole in different superficial fungal infections.
|
|
|
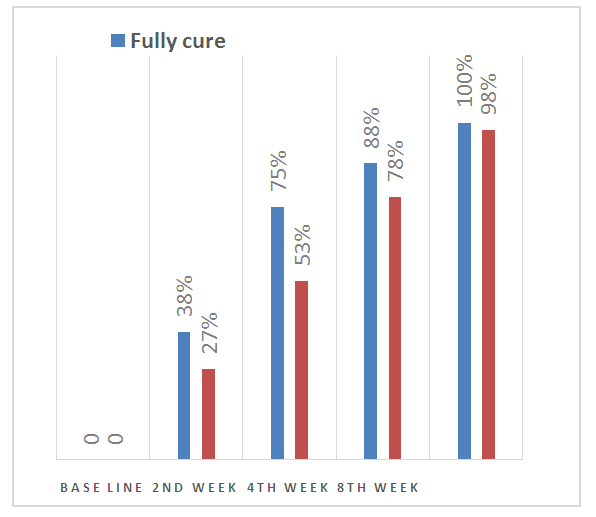 | Figure 2. Distribution of the patient by follow up after voriconazole therapy |
6. Conclusions & Recommendations
- In our study no resistance against voriconazole was found whereas resistance against fluconazole was noted among all species of dermatophytes, followed by terbinafine. Among all the study people 88% was fully cure and rest of 12% were partially cure with voriconazole which seems to be more effective against dermatophytes. For more specific and potential information we would like to recommend for conducting more studies on the same issue.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML