-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 10(1): 6-10
doi:10.5923/j.ajdv.20200901.02

Intralesional Therapy of Vitiligo by 1% Lactic Acid Solution Versus Triamcinolone Acetonide Injection
Khalifa E. Sharquie 1, Adil A. Noaimi 1, Sarmad Adnan 2, Ann Mahjoob Al-Niddawi 3, Wesal K. Aljanabi 3
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology and Venereology, Dermatology center, Medical City, Baghdad, Iraq
2Arab Board for Dermatology and Venereology, Dermatology Center, Medical City, Baghdad, Iraq
3Dermatology Center, Medical City, Baghdad, Iraq
Correspondence to: Wesal K. Aljanabi , Dermatology Center, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

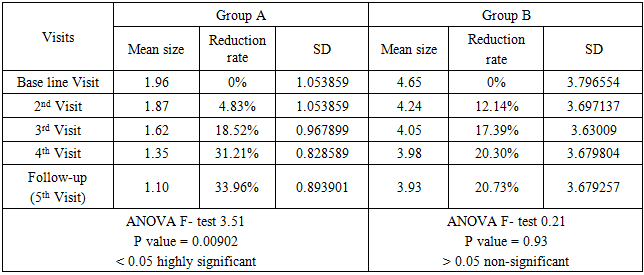
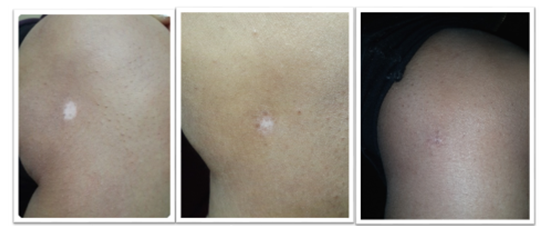
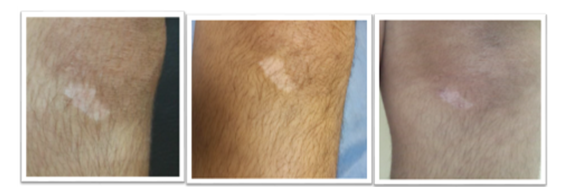
Vitiligo is a common autoimmune disease, where many topical and systemic therapies has been used, and each has its own advantages and disadvantages. Lactic acid has been used successfully in the treatment of vitiligo as a topical solution and was an effective intralesional therapy of alopecia areata. The objectives is to use 1% intralesional lactic acid in the treatment of vitiligo especially in localized patches. This is an interventional, case control, single blind, comparative study that was conducted in the Department of Dermatology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq, between April 2016 and July 2017. Forty-five patients with vitiligo and 64 patches were enrolled in this study, 33 (73.33%) patients were females and 12 (26%) patients were males, with a female to male ratio of 2.7:1. They were divided into 2 groups according to type of therapy. Group (A) (lactic acid 1% solution): twenty-three patients with 31 patches were included in this group. Lactic acid solution 1% was injected intralesionally every 2 weeks. Group (B) (triamcinolone acetonide injectable suspension): Twenty-two patients with 33 patches were included in this group. Intralesional triamcinolone acetonide was injected every 2 weeks. Treatment of both groups continued for 6 weeks (three sessions), and further three months as follow up. Group (A): The mean surface area of the lesions was decreased from 1.96 cm2 to 1.10 cm2 from the baseline visit to the last follow-up visit with a reduction rate mean of 33.9 and a P value of 0.00902, which was highly statistically significant. Group (B): The mean surface area of the lesions was decreased from 4.56 cm2 to 3.93 cm2 from the baseline visit to the last follow-up visit with a reduction rate mean of 20.9 and a P value of 0.93 and was statistically insignificant. In conclusion, lactic acid was proved statistically significant cost effective intralesional therapy for localized patches of vitiligo with a P value of 0.00902, while the use of triamcinolone acetonide intralesional injections gave a p value of 0.93 and was statistically insignificant.
Keywords: Vitiligo, Lactic acid, Sharquie, Iraq
Cite this paper: Khalifa E. Sharquie , Adil A. Noaimi , Sarmad Adnan , Ann Mahjoob Al-Niddawi , Wesal K. Aljanabi , Intralesional Therapy of Vitiligo by 1% Lactic Acid Solution Versus Triamcinolone Acetonide Injection, American Journal of Dermatology and Venereology, Vol. 10 No. 1, 2020, pp. 6-10. doi: 10.5923/j.ajdv.20200901.02.
1. Introduction
- Treatment of vitiligo is essentially needed in many patients especially those with dark skin as it makes a great contrast and gives a very bad cosmetic appearance that sometimes might lead to a social isolation, thus interfering with all daily activities. Although there are many variants of medical therapies many patients do not prefer these modalities of treatment as they need many applications during the day and could be long lasting and interfere with the patient’s life behavior and daily activities, therefore some patients might prefer melanocytes transplant [1-3] or narrow band exposure [4-6] or giving intralesional therapies like in needling techniques. [2,3,7,8]Lactic acid has been used since ancient time as a good cosmetic procedure as what has been used by queen Cleopatra in Alexandria since 69 B.C to maintain her beauty and for skin rejuvenation. [9]Sharquie et al used lactic acid in many skin diseases: as a peeling agent in the treatment of melasma [9] or as a topical agent for vitiligo treatment [10, 11] and as an intralesional in treatment of Striae Distensae [12] and in alopecia areata. [13]As lactic acid can cause the release of cytokines during its therapy and causing stimulation of keratinocytes; the theory behind this repigmentation is through what is called irritant theory which is similar to the inflammation induced by psoralen compound and ultraviolet light (UVL) through stimulation of keratinocytes to release inflammatory mediators such as basic fibroblast growth factor, interleukine-1, leukotriene C4 and E4, TGF-α (transforming growth factor alpha) and endothelin–1,3 thus stimulating proliferation of melanocytes and inducing repigmentation. [14] This probably helped for the recovery of the disease whether it is vitiligo, alopecia areata or other.The objective of the present work is to use lactic acid 1% as intralesional therapy for vitiligo once every 2 weeks especially in patients with localized vitiligo.
2. Patients and Methods
- This is an interventional, case control, single blind, comparative study that was conducted in the Department of Dermatology. Baghdad Teaching Hospital, Medical City, Baghdad, Iraq, between April 2016 and July 2017. The diagnosis of vitiligo was based on clinical ground with the characteristic loss of skin pigmentation and the examination under Wood’s lamp. The evolution of vitiligo was considered active when new lesions appeared and the existing lesions had increased in size over the past 3 months, and was considered stable when depigmentation had not increased during the last 3 months and no new lesions appeared. Photographs were taken for each patient at each visit by a mobile GALAXY note 3 Camera, at the same place, distance and illumination. All cases had received no treatment for at least 6 months before starting therapy. Verbal consent was taken from each patient before starting the trial after a full explanation for the nature of the disease, cause, prognosis, the drug, the method of treatment, duration of follow up and the possible side effects. Patients were divided into 2 groups, according to type of therapy:Group A: they were injected intradermally by insulin syringe 30 gauge with lactic acid 88% concentration, which was diluted with distilled water to have a final concentration of 1%, PH 6.84. Group B: they were injected intradermlIy by insulin syringe 30 gauge with triamcinolone acetonide injectable suspension (40mg/ml, Bristol-Myers Squibb) which was diluted with distilled water to 5mg/ml, mixed well. The treatment of both groups continued for six weeks (three sessions), and further three months as follow up. Patients were evaluated clinically by looking for any changes in the size and follicular pigmentation by using graph sheets. During each visit of follow up, any adverse effects were recorded of both drugs like pain, erythema, itching and others. ANOVA Independent T-test were used for statistical analysis.
3. Results
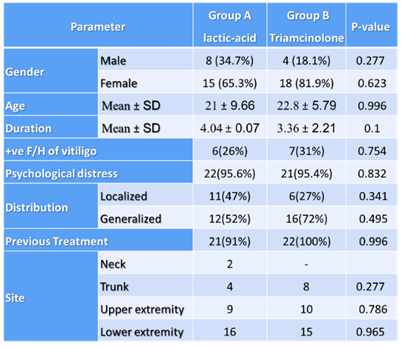
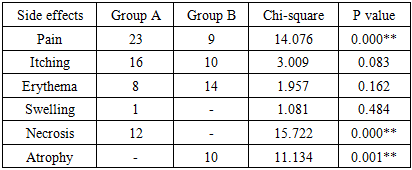
- Forty-five vitiligo patients were enrolled in this study and being evaluated during both treatment and follow-up period. They were 33 (73.33%) females and 12 (26.77%) males with female to male ratio of 2.75:1. Their ages ranged from 7 - 45 years. The disease duration ranged from 12-180 months. The family history of vitiligo was positive in 13 (28.88%) of cases. The Psychological distress history was positive in 43 (95.5%) and 66% of the cases were affected by generalized vitiligo.Total number of the lesions were 64 patches with a mean of 1.4 lesion per patient and the surface area of the lesions ranged from 0.5-15 cm2.Group A: twenty-three patients with 31 patches were included in this group. Eight (34.7%) patients were males and 15 (65.2%) were females, with a duration Mean ±SD of 4.04 ±0.07. Group B: Twenty-two patients with 33 patches were included in this group. Four (18.1%) patients were males and 18 (81.8%) were females, with a duration Mean ±SD of 3.36±2.21. The distribution of the lesions was shown in table 1 for each group; lower extremity lesions represent 51.6% of the group A lesions and 45.4% of group B lesions.
|
|
|
4. Discussion
- Vitiligo is a common autoimmune disease where there are many topical and systemic therapies like topical psoralen, khellin, pseudocatalase and calcium in combination with short term UVB exposure, steroids, immunomodulators as tacrolimus and pimecrolimus ointment, iodine tincture, 20% sour orange solution and UVA singly or in combination, and Topical lactic acid solution. [14-20] Systemic therapies as psoralens + UVA, PUVASOL (psoralens and sunlight) and Systemic steroid. [14,16,21], and Finally Surgical treatment as Tissue Grafts in Melanocyte transplant by needle micro grafting. [2]According to the available literatures, intralesional Corticosteroid therapy was used by E. Kandil in 1970 [22] whom demonstrated that 45 of 52 patches in 26 patients responded to intralesional corticosteroid injection and PUVA, however in 1979 Vasistha and Singh conducted a ‘‘head-to head’’ comparison between intralesional corticosteroid injections and intralesional distilled water injections and found no significant difference in repigmentation. A more recent study run by Wang E. from 2009-2013 showed 80-90% repigmentation in patients treated with intralesional corticosteroid with concomitant therapy like tacrolimus and NB-UVB. [22]Lactic acid is an Alpha-hydroxy acids, which has been used since ancient to induce rejuvenation of the skin as in the time of Cleopatra around 69 B.c. It has been used for the first time by sharquie since 2005 as a therapeutic peeling agent in the treatment of melasma [9]. Later on lactic acid 15% has been used in the treatment of vitiligo as a topical agent and was effective as topical iodine tincture [10] and since then this therapy has been ued for hundreds of patients and improved its effectiveness, and the theory behind this repigmentation is through what is called irritant theory which is similar to the inflammation induced by psoralen compound and ultraviolet light (UVL) through stimulation of keratinocytes to release inflammatory mediators such as such as basic fibroblast growth factor, interleukine-1, leukotriene C4 and E4, TGF-a (transforming growth factor alpha) and endothelin–1,3 thus stimulating proliferation of melanocytes and inducing repigmentation. [14] As lactic acid is an effective repigmenting agent in vitiligo, this encouraged us to conduct the present study to use it as an intralesional agent similar to what has been used in the treatment of alopecia areata where it gave a cure as compared to triamcinolone and causing no side effects. [13]The result of the present work was very encouraging as the repigmentation started 2 to 3 weeks after intralesional session and progressed to have a statistically highly significant result with p value 0.00902 and a reduction rate mean 33.9%. This new kind of therapy is worthy to be advised in localized type of vitiligo especially when failed to respond to other type of treatment. Triamcinolone has been used since long time ago as a topical and intralesional therapy of vitiligo. The present study showed that triamcinolone injection has a bit more rapid response than lactic acid but at the end of the study 4 months and a half when compared to lactic acid it was statistically insignificant with a p value of 0.9 and this was consistent with the results of Vasistha and Singh. Accordingly, lactic acid was more effective as a repigmenting agent. In addition, triamcinolone injection caused some atrophy at the area of injection although it was diluted with distilled water from 40mg/ml to 5mg/ml, mixed well and intradermal injection was carried out by insulin syringe 30 gauge. However, lactic acid local injection was more painful when compared to triamcinolone injection.
5. Conclusions
- Intralesional injection of lactic acid in the treatment of localized vitiligo is a new cost effective mode of therapy and was more effective than triamcinolone injection with a little or no side effects.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML