-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2020; 9(1): 1-5
doi:10.5923/j.ajdv.20200901.01

Outbreak of Hair Dye Dermatitis with Imitating Tendency
Khalifa E. Sharquie1, Adil A. Noaimi1, Roaa L. Hasan2
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
2Department of Dermatology, College of Medicine, University of Baghdad, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Hair dye is a common cosmetic agent that had been used since ancient times that might be associated with hair dye dermatitis in certain people. In Iraq for the last 3 years, the frequency of hair dye dermatitis is increasing. Objective: To record this outbreak of hair dye dermatitis in the Iraqi population and to evaluate the different types of hair dye rash. Also to study its clinical patterns in relation to gender and sites. Patients and Methods: This is a descriptive, clinical study that was done in the Center of Dermatology -Medical City, Baghdad, Iraq through August 2016 to September 2017. A total number of 56 patients were seen and history and physical examination were carried out to record all socio-demographic data related to this problem. Results: A total of 56 patients with a clinical diagnosis of hair dye dermatitis were included in this study. Their ages ranging from 20 to 72 years with a mean ±SD of (52.3±9.5) years. The males were 47(83.9%) patients and females were 9 (16%) patients with a male: female ratio 5.2:1. The male age ranged 28-65y with a mean 52.4y while female ages ranged from 20-72y with a mean 52.2y. The most common sites of involvement were the face in 55 (98.2%) patients followed by neck and v -shape of the chest in 40 (71.4%) scalp and scalp margin in 30 (54%). While upper extremities involved in 15(26.7%), the dorsal aspect of hands in 12 (21.4%) patients, and chest in 7 (12.5%) patients. The most common pattern of distribution was localized lesion in 42 (75%) patients and photo-distributed in 8 (14.20%) and generalized lesion in 6 (10.7%) patients. The majority of cases were above 40 years 51(91.7%) patients. The most common clinical presentation of skin rash was dermatitis in 35(62.5%) of the patients, followed by a lichenoid eruption in 11(19.9%), actinic dermatitis in 4(7.1%), facial melanosis and angioedema in 3(5.3%) for each one. In conclusion; this is the first Iraqi study reporting outbreak of hair dye dermatitis with a mean age of 52.3 years which was mainly a disease of males (83.9%). The face was the commonest site affected (98.2%) while the scalp was involved in 54%. The rash could be localized to the head or could be generalized and might take many clinical patterns like dermatitis, lichenoid rash or photodermatoses.
Keywords: Hair Dye Dermatitis, Paraphenylenediamine, Iraq
Cite this paper: Khalifa E. Sharquie, Adil A. Noaimi, Roaa L. Hasan, Outbreak of Hair Dye Dermatitis with Imitating Tendency, American Journal of Dermatology and Venereology, Vol. 9 No. 1, 2020, pp. 1-5. doi: 10.5923/j.ajdv.20200901.01.
Article Outline
1. Introduction
- There are a variety of hair dyes that have been used since ancient times [1] Types of hair dyes can be either vegetable hair dye like Henna, [2] metallic hair dye that derived from silver salts, lead, [3] or synthetic hair dye that can be either nonoxidative (temporary and semi-permanent) or oxidative such as demi-permanent and permanent. [4] Contact allergy to vegetable hair dyes are rarely reported, [5] but commonly seen in hair dye paraphenylenediamine (PPD) which is well known as the most important allergen associated with hair dye-related allergic contact dermatitis. [6,7] It has been used for a long time, [8] and a preferable content in many hair dye formulas as it gives longer-lasting black or intensified natural color. [7] The incidence of PPD dermatitis 4.3% in Asia, 4% in Europe, and 6.2% in North America [9]Hair dye dermatitis clinically may present as irritant contact dermatitis, allergic contact dermatitis, photo contact dermatitis, contact urticaria, contact leucoderma, contact anaphylaxis, photosensitivity, airborne contact dermatitis like picture and prurigo -like lesion. Rarely adverse reaction to hair dye can present with a non-eczematous morphology like a lymphomatoid contact dermatitis, dysmorphic syndrome, eye lens toxicity, renal impairment, proteinuria, hematuria, hypertension, and bronchospasm. Hydrogen peroxide present in hair dyes may cause structural hair shaft damage. Also, loss of eyelashes with the use of mascara containing PPD might occur. Another area of concern is the association of the use of hair dyes and malignancies. [9]PPD is the most common cause of hair dye dermatitis, [6,7] but other content as resorcinol can cause sensitization. [10] PPD can cross-react with local ester anesthetics, rubber Toluene -2,5- diamine. (11) Diagnosis of Hair dye dermatitis by history and clinical approach. [12] Patch test which is the gold standard test to confirm hair dye contact allergy is by an epicutaneous patch test. [13,14] Open testing is recommended by hair dye manufacturers to test for allergic reactions 48 hours prior to hair dye applications. [15,16] In vitro tests also could be carried out. [17]Hair dye dermatitis is increasing all over the world due to the increase in applications of hair dyes. [9] Hair dermatitis in Iraq was seen as a sporadic case from now and then but over the last few years the frequency of hair dye dermatitis is increasing forming an outbreak, accordingly, the present work is arranged to do a clinical assessment of hair dye dermatitis among Iraqi patients.
2. Patients and Methods
- This is a descriptive, clinical study was done in the Center of Dermatology-Medical City, Baghdad, Iraq, through August 2016 to September 2017. Formal and ethical approval was granted by the Scientific Committee of the Scientific Council of Dermatology and Venereology-Arab Board for Health Specializations. After explanation to each patient about the nature of disease including its cause, course, complications, prognosis, treatment modality, their complications and the goal of the study, photography in good illumination was taken with Galaxy Note 4 phone camera, 16 megapixels, resolution 2988x5312. The scientific name in all dyes that had been used by the patients was paraphenylenediamine (PPD). A total number of 56 patients were included in this study, males were 47 (84.9%) patients and females were 9(16%) patients. A full history was taken from each patient regarding the following: age, gender, duration of the lesions, chief complain, associated symptom, recurrence, aggravating and relieving factors, the site, type, geographical distribution of the lesion, types of hair dye being used, job, family history, past medical, drug history. Clinical examination was done regarding the sites, types, and distribution of the lesions. Descriptive statistics were done including number, percentages, mean and standard deviation.
3. Results
- A total of 56 patients with hair dye dermatitis that diagnosed clinically were enrolled in the study. Their ages ranging from 20 to 72 years with a mean ± SD of 52.3±9.5 years and male: female ratio 5.2:1. The male patients were 47 with age ranged 28-65 years, the youngest male was 28 years old and the oldest with 65 years old with a mean ±SD for their age 52.4±8.2 years. While female patients were only 9 in number, with ages ranged from 20-72 years. The youngest female was with 20 years old and the oldest one of 72 years old with a mean ± SD value of age 52.2 ± 15 years.The chief complain was itching and skin rash in all the patients. This rash associated mainly with itching in 46 patients while the other patients were complaining from burning sensation or pain. Nearly all of them were chronic hair dye users except, one female developed skin lesion from the first use of hair dye.Different sites of the body were involved including the face in 55(98.2%) patients, the neck and v -shape of the chest in 40(71.4%) patients, scalp and scalp margin in 30(54%) patients, upper extremities in 15(26.7%) patients, the dorsal aspect of hands were affected in 12(21.4%) patients and chest was involved in 7(12.5%) patients.
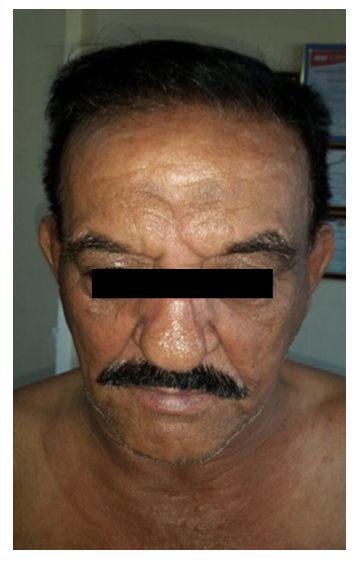
 | Figure 1. A 55 years old male presented with lichenoid dermatitis over the face due to hair dye |
 | Figure 2. A 58 years old male presented with actinic dermatitis of the face due to hair dye |
 | Figure 3. A 45years old male presented with Per- orbital angioedema due to hair dye |
 | Figure 4. A 61 years old male presented with generalized skin rash due to hair dye application |
4. Discussion
- Hair dye dermatitis is a well-recognized entity that has been recorded since long times. [18]Hair dyes are one of the most commonly applied cosmetics by the elderly and young alike. This rising tendency of hair coloring had resulted in an increased frequency of hair dye associated adverse effects. [19]This allergic reaction is increasing all over the world but especially in Asia. [9] In Iraq, sporadic cases of hair dye dermatitis were seen but they were also increasing over time especially in the last three years.Unfortunately, the disease is not well recognized as the patients have different sites of distribution in the body making the diagnosis easily to be missed, especially if the patients are not asked about the use of hair dye. Accordingly one should think about the reason behind this outbreak of hair dye dermatitis in the Iraqi population. Although we cannot find an actually clear cause for this outbreak, we can speculate that a bad chemical formula of hair dyes imported to Iraq or different types of hair dyes were used that have not been used before this outbreak. Another reason might be due to the application of hair color that had increased tremendously over the last few decades due to increased social pressure and the change in fashion trends. [9] The present study showed that male to female ratio was 5.2:1 and the reason behind this couldn’t be explained but we can suggest that the increased use of hair dyes among males in the last few years is one of the causes. Also, another reason behind this increase among males is using a high concentration of hair dye ranging from black to deep brown that gives rapid and long-lasting effect due to higher concentration of PPD in dark colors hair dye compared to light colors, [7] that has been used by females. Although the present work showed that the most common clinical pattern of hair dye dermatitis among the patients were localized dermatitis (62.5%), but a lichenoid eruption (19.9%), actinic dermatitis (7.1%), angioedema (5.3%) and facial melanosis (5.3%) were also seen and this pattern of rash was not well recognized in the published literature. [20] This study showed that the face (98.2%) was almost always involved and the scalp (54%) was relatively less commonly affected and the most common site of scalp involvement was the scalp margin. While in Gupta's study the most common site affected was scalp in (61.2%) of the patients. [20] The reason for the scalp being relatively spared except the margin is that the scalp has a thick skin so the dye is difficult to be absorbed and causes sensitization. That’s why the diagnosis could be missed easily as the first complaint of the patient is not the scalp involvement.Generalized dermatitis was seen in 10.7% of patients in the present study, this could be explained either the hair dye will be distributed all over the skin during bathing of the hair dye or the hair dye is absorbed from the skin into the blood causing general allergic reaction. [9]The exact nature of the haptens association with PPD sensitivity remains not well understood. The metabolized in the skin especially the p-benzoquinone are considered responsible for its allergenicity and cross-reactivity. Another possibility is that Bandrowski's based, a of PPD formed on exposure is responsible for its allergenicity. [20,21,22]A genetic polymorphism in the cutaneous metabolism of PPD too has been suggested to explain why only a few individuals applying hair dyes well develop contact sensitivity or variable allergic responses. [23]In a recent study by Gupta et al 2015 where many findings are comparable to the result of the present work. [20] The age of patients was similar to the age mean (52.2%) years in the present study while in Gupta study it was (62.47%) years. The frequency of hair dye dermatitis was much higher in males in the present work with male to female ratio was 5.2:1 while in Gupta study male to female ratio was 1.4:1. Many patients might not complain from scalp rash but present with generalized dermatitis as had been noticed in the present work and this might mask the diagnosis for a long time before the actual diagnosis of hair dye dermatitis is reached.
5. Conclusions
- This is the first Iraqi study reporting outbreak of hair dye dermatitis with a mean age of 52.3 years which was mainly a disease of males (83.9%). The face was the commonest site affected (98.2%) while the scalp was involved in 54%. The rash could be localized to the head or could be generalized and might take many clinical patterns like dermatitis, lichenoid rash or photodermatoses.
Disclosure
- This study is independent study and not founded by any Drug company.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML