Khalifa E. Sharquie1, Fatema A. Al-Jaralla2
1Department of Dermatology, College of Medicine, University of Baghdad. Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
2Department of Dermatology, College of Medicine, University of Baghdad, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad. Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: there are groups of skin diseases that share a characteristic clinical picture that resemble first and 2nd degree burn which have diagnostic properties although are different in their etiology, and to put them in one group, to make easy, early diagnosis and management. Objective: to collect these different skin disorders in one address as all of them have characteristic clinical picture as burn like and to do new classification aiming to find diagnostic features that are helpful in establishing the right diagnosis and therapy. Patients and methods: this is case series descriptive study that was conducted in department of dermatology, college of medicine, university of Baghdad, Baghdad teaching hospital during the period from 2006 through 2019 where all cases with features of 1st and 2nd degree burn like rash were collected and analyzed into groups aiming to find characteristic features that are helpful in diagnosing and management of these skin diseases. Results: certain dermatoses are gathered together including pellagra, acrodermatitis enteropathica, thallium poisoing, fixed drug eruption, Stevens Johnson syndrome, toxic epidermal necrolysis, staphylococcal scalded skin syndrome that have characteristic burn like rash in most of the cases in the early course of the disease. While other skin diseases that can occasionally or rarely present with burn-like picture during the course of the disease like mycosis fungoides, pemphigus, solar keratosis, lichen planus actinicus, hair dye dermatitis, pedaerus dermatitis, necrolytic migratory erythema, discoid lupus erythematosus, dermatitis artefacta and acute cement burn. Conclusion: pellagra, acrodermatitis enteropathica, thallium poisoning and fixed drug eruption with Stevens Johnson syndrome, toxic epidermal necrolysis, staphylococcal scalded skin syndrome, are grouped together as all of them commonly share characteristic burn like clinical picture in early course of the disease and almost seen in all patients. While many other skin diseases might occasionally or rarely present with a burn like picture during the course of the disease that might lead into misdiagnosis.
Keywords:
Burn like rash, Thallium, Zinc deficiency
Cite this paper: Khalifa E. Sharquie, Fatema A. Al-Jaralla, Burn- Like Dermatoses: A Neglected Group of Skin Diseases with a New Classification, American Journal of Dermatology and Venereology, Vol. 8 No. 5, 2019, pp. 88-93. doi: 10.5923/j.ajdv.20190805.03.
1. Introduction
Burn-like lesions can be life threatening and carry diagnostic as well as management challenges; the term burn like syndrome has been proposed by Atiyeh B.S. et al in 1999 [1] to include skin disorders manifested by blistering and exfoliation mimicking burn injuries in their clinical presentation and behavior as they are characterized by sloughing of the epidermal layers, which uncovers the underlying dermis. A number of skin conditions were mentioned with emphasis on toxic epidermal necrolysis (TEN). [1] A second article in 2005 mentioned six diseases mimicking burn with complications, treatment requirements, and outcome of burns; namely; Stevens-Johnson disease; TEN, bacterial fasciitis; skin necrosis combined with coagulation disturbances; pemphigoid; and subacute cutaneous lupus erythematosus. [2]The objective of the present work is to do new classification of these diseases and to add new diseases as a cause of burn like dermatosis.
2. Patients and Methods
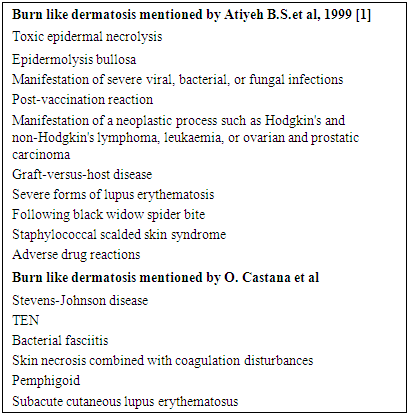
Patients and methods: this is case series descriptive study that was conducted in department of dermatology, college of medicine, university of Baghdad, Baghdad teaching hospital during the period from 2006 through 2019 where all cases with features of 1st and 2nd burn like rash were collected and analyzed into groups aiming to do new classification aiming to find characteristic features that are helpful in diagnosing and management of these skin diseases.Many dermatoses present almost always with burn-like lesions in the early onset of the disease, these include Stevens-Johnson disease and TEN; zinc deficiency; thallium intoxication; pellagra and fixed drug eruption.However, certain skin diseases might occasionally or rarely present with burn like during the course of the disease. They may not come at the top of the list, but keeping these diseases in the differential list that will aid physicians to reach final diagnosis. Table 1. Lists burn-like diseases mentioned previously in the literature
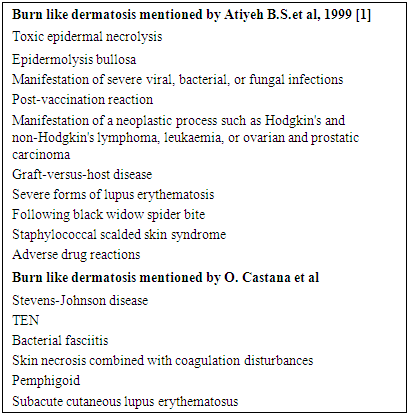 |
| |
|
3. Results
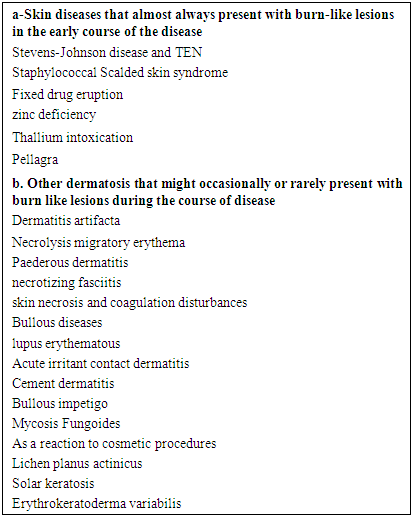
We made a list of dermatosis that has the clinical presentation of burn like rash (table 2).Table 2. Showing diseases with burn-like Dermatoses
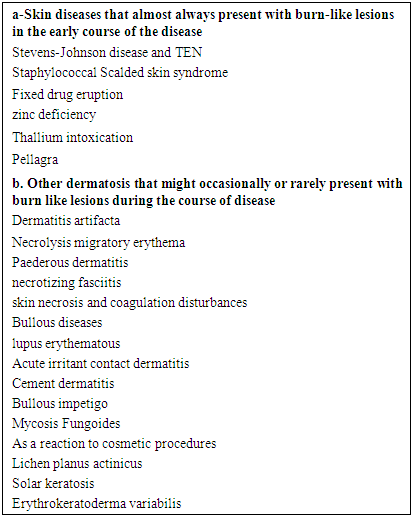 |
| |
|
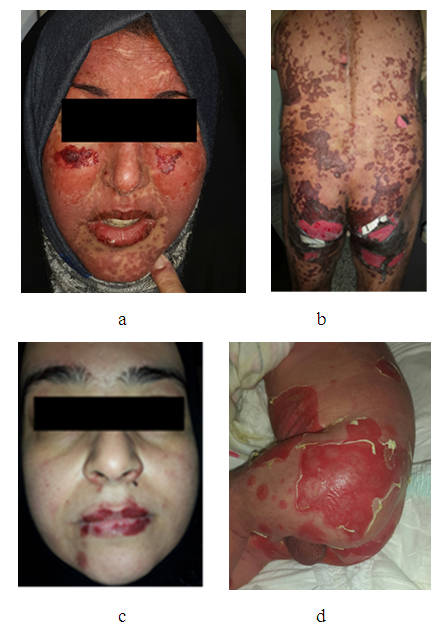
We have grouped burn like dermatoses into the following:1-Skin diseases that almost always present with burn-like lesions in the early course of the disease, these include:Stevens - Johnson syndrome (SJS) and Toxic Epidermal Necrolysis (TEN)These two syndromes are said to exist at the two ends of the spectrum of an adverse skin burn like reaction occurring from severe epidermolysis [3,4]. The initial presentation of SJS/TEN may include non-specific symptoms such as fever, discomfort with swallowing, and stinging eyes. The second phase is the development of wide-spread areas of epidermal separation Early locations for skin involvement include the presternal truncal region, the face, and could also involve the palms and the soles. In about 90% of patients, there is involvement of the mucosa of the mouth, genital and/or gastrointestinal tracts visible as erythema and erosions [5]. Figure 1a and b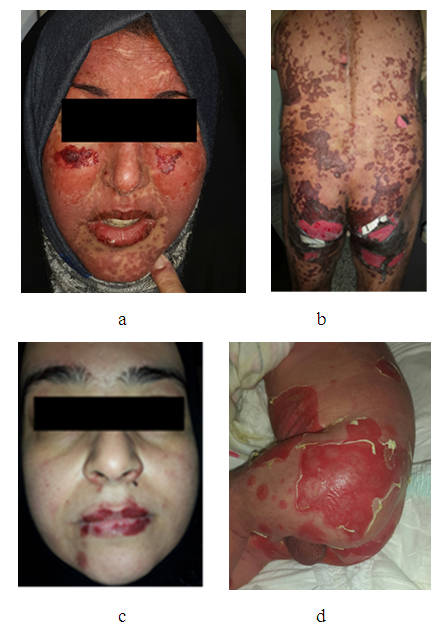 | Figure 1. a. patient with Stevens - Johnson syndrome showing confluent erythema, ruptured bullous lesions leaving denuded skin with burn like picture b. TEN c. fixed drug eruption d. staphylococcal Scalded skin syndrome |
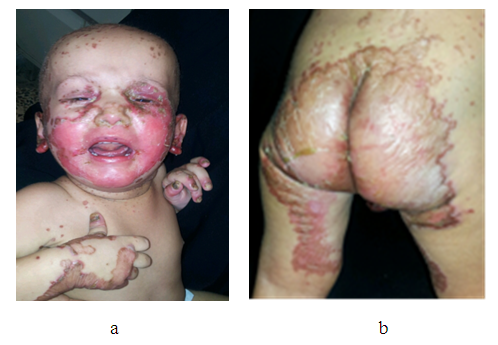
A major percentage of the disease is caused by medications like allopurinol, NSAIDs, antibiotics, and anticonvulsants, while the remaining is due to upper respiratory infections such as HIV [5], Hepatitis virus, Herpes virus, Mycoplasma pneumoniae [7,8]. Others include malignancies, as well as idiopathic.Fixed drug eruptionFixed drug eruption (FDE) is an adverse drug effect that appears as sudden onset of round and/ or oval, burn like edematous, dusky-red macules/plaques on the skin and/or mucous membranes, accompanied by burning and/or itching. (Figure 6). Medications taken episodically, such as pain relievers, antibiotics, or laxatives, are often to blame. [9] figure 1c.Staphylococcal scalded skin syndrome Staphylococcal scalded skin syndrome (SSSS) is a systemic blistering skin disorder leaving large areas of denuded skin with burn like picture. It arises from the systemic circulation and accumulation in the skin of exfoliative toxins A and ⁄or B from an infection focus, resulting in a proteolytic cleavage of desmoglein 1. [10] figure 1 d.Acrodermatitis enteropathica (ADE) Zinc is an essential trace nutrient required for the proper function of more than 100 enzymes and plays a crucial role in nucleic acid metabolism concern for the patient. Zinc deficiency can be acquired or inherited. There are many causes of acquired zinc deficiency: premature infants, low birth weight, zinc deficiency in maternal milk, exclusive parenteral nutrition, malabsorption syndromes such as Crohn disease and celiac disease, alcoholism, low calcium and phytate diet, and kwashiorkor. [11,12]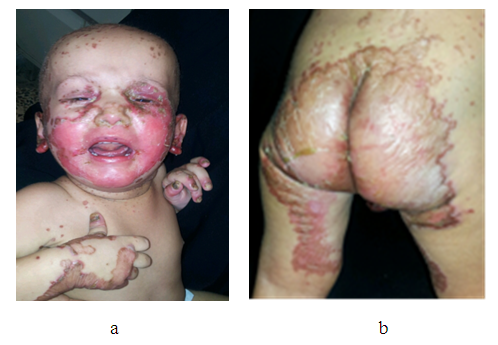 | Figure 2. a and b –infant with acrodermatitis enteropathica showing burn like dusky red lesions with blisters around the mouth with angular stomatitis, napkin area and limbs |
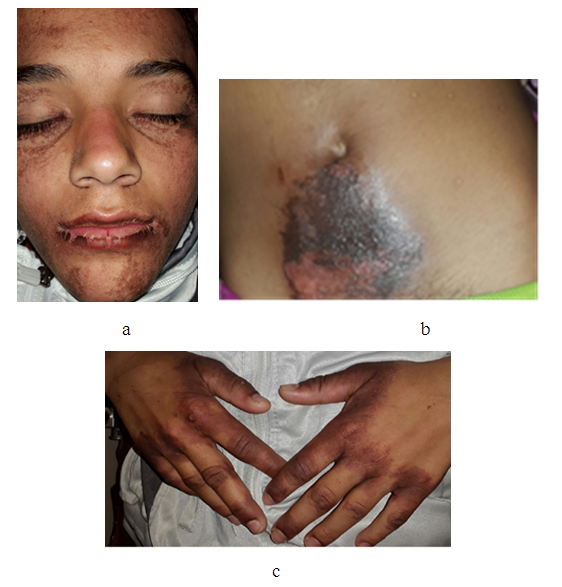
Acrodermatitis enteropathica is an autosomal recessive disorder postulated to occur as a result of mutations in the SLC39A4 gene located on band 8q24.3 [13,14] The disease begins with burn like symmetrical erythematous, squamous or eczematous lesions, sometimes vesiculobullous or pustular lesions, located around perioral, anogenital, and acral areas. The severity of the skin lesions is variable. Without treatment, skin damage becomes erosive and spreads to other periorificial areas of the face (eyes, nose, and ears), neck, lower abdomen, back, inguinal area, and thighs. Other features consist of diffuse alopecia, loss of eyelashes and eyebrows, glossitis, gingivitis, angular stomatitis, onychodystrophy, onycholysis [12,14]. Diarrhea is the predominant extracutaneous symptom, general symptoms and neuropsychological disorders are common (irritability, lethargy, depression, anorexia), and also growth retardation, weight loss, anemia, and ophthalmic involvement (photophobia, blepharitis, conjunctivitis). Secondary bacterial infections (with Gram-positive and sometimes Gram-negative) or candidiasis (Candida albicans) are common and they can modify the clinical picture. [15] Thallium intoxication Thallium is a heavy metal that has the qualities of a perfect criminal poison. Its salts are tasteless, odorless, dissolve completely in liquids, are rapidly absorbed, and defy detection on routine toxicological screens. Thallium has been the agent of choice in several criminal poisonings [16]. In the past, thallium was used as a therapeutic agent to treat syphilis, gonorrhea, tuberculosis, and ringworm, and it was also used as a depilatory for excess hair [17,18]. Thallium was also widely used as a rodenticide [19]. Average lethal dose for thallium sulphate has been reported from 10 to 15 mg/kg. [20]Its toxic effect is due to its ability to inhibit a number of intracellular potassium-mediated processes and ligand formations with protein sulfhydryl groups, inhibition of cellular respiration, interaction with riboflavin and riboflavin-based cofactors, and distribution of calcium homeostasis. [21]An outbreak of thallium poisoning was reported in Baghdad in February 2008 where members of the Iraqi Air Force Club and some of their children were poisoned by cake laced with thallium. Two of the children died. [16]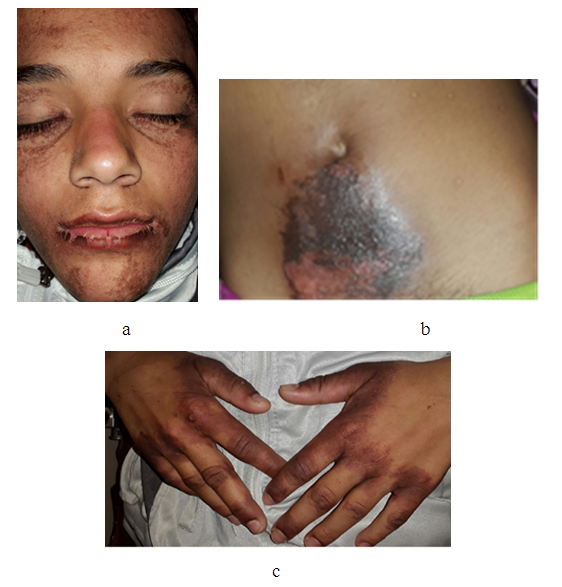 | Figure 3. a, b, and c –a boy with accidental thallium poisoning due to inadvertent ingestion of a rodenticide showing dusky red burn like rash of the face, hands and abdomen |
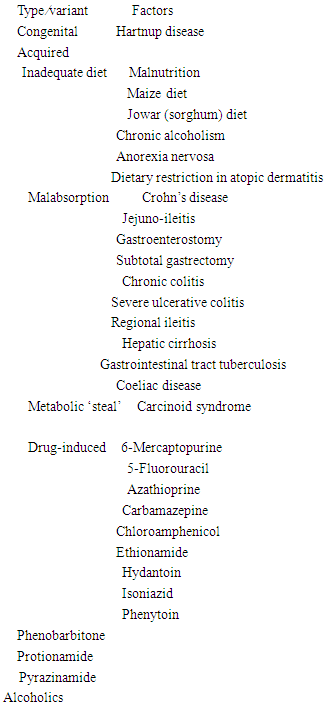
The clinical features of short-term thallium intoxication include the gastrointestinal symptoms of nausea, vomiting, stomatitis, and diarrhea, followed by severe painful dysesthesia and paresthesia in the distal limbs, dusky erythematous burn like rashes on the cheeks and perioral region, hands and hyperkeratosis with loss of hair in the subacute stage. [22]Oral Zinc sulphate appears to be an effective and safe treatment for thallium poisoning particularly for skin and hair features and in reducing its lethal progression and complications. [23]PellagraPellagra occurs as a result of a deficiency in niacin (also known as nicotinic acid or vitamin B3). Niacin is a water‐soluble B‐complex vitamin and important component of two co‐enzymes, nicotinamide‐ adenine dinucleotide (NAD) and NADP, which act as hydrogen donors and acceptors in numerous anabolic and catabolic reactions. Pellagra is clinically manifested by the 4 D’s: dermatitis (photosensitive) similar to burn, diarrhea, dementia, and death. Conditions that cause niacin deficiency are listed in table 3 [24]. In Iraq, all cases of pellagra are seen among alcoholics and rarely observed as a part of pure nutritional deficiency [25] acute pellagra resembles acute sunburn. The skin is red, and large blisters that may develop often exfoliate, leaving large areas of denuded epithelium that may resemble severe sunburn. The changes subside, leaving a dusky, brown-red coloration. [26] The usual sites are the dorsal surfaces of the hands, face, neck, arms, and feet. [27] figure 4 and 5.Table 3. Medical conditions that cause niacin deficiency
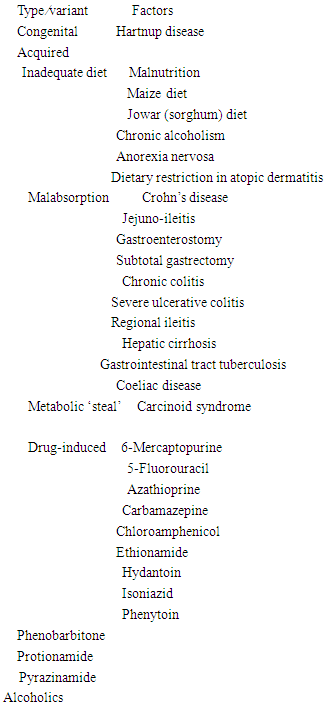 |
| |
|
 | Figure 4. a and b patient with burn like photosensitivity due to pellagra following alcoholism, c and d Pellagra due to Hartnup disease |
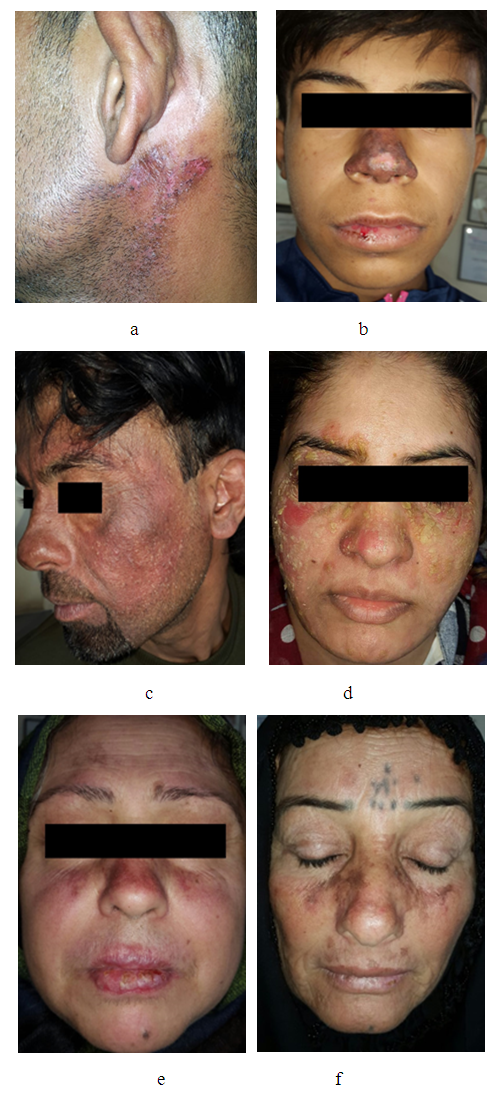
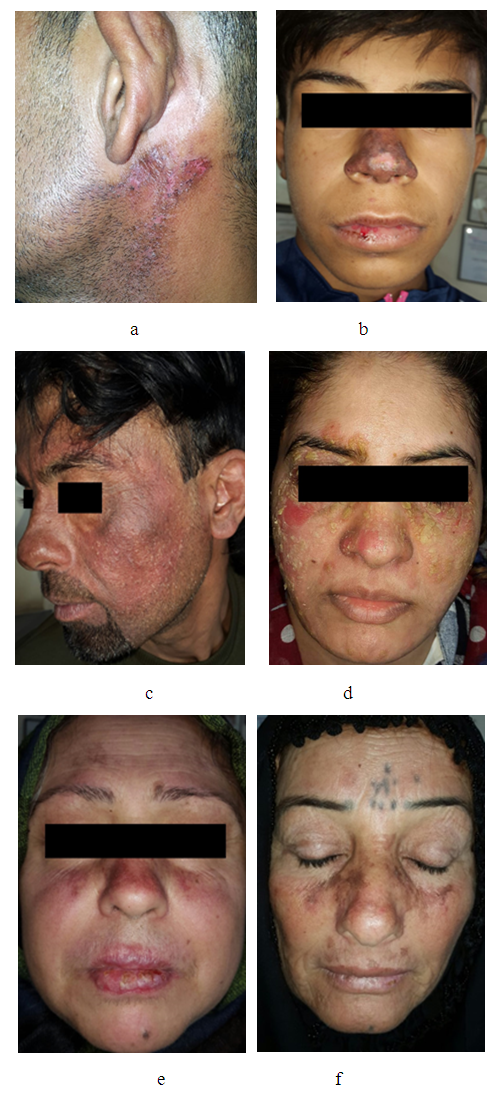 | Figure 5. Paederus dermatitis. b DLE, c hair dye dermatitis, d Pemphigus foliaceus e. actinic lichen planus butterfly like solar keratosis |
2-Other dermatoses that might occasionally or rarely present with burn like lesions during the course of the disease (table), these include:Paederus dermatitis is a peculiar, irritant contact dermatitis characterized by a sudden onset of erythematobullous lesions on exposed areas of the body. The disease is provoked by an insect belonging to the genus Paederus. This beetle does not bite or sting, but accidental brushing against or crushing the beetle over the skin provokes the release of its coelomic fluid, which contains paederin, a potent vesicant agent [28] figure 6a.Other dermatoses that present with burn rash like discoid lupus erythematosus (DLE) figure 6 b, hair dye dermatitis figure 6c, Pemphigus foliaceus figure 6 d, and actinic lichen planus, butterfly like solar keratosis, figure 6 e.
4. Discussion
Burn like dermatoses are gathered together aiming to be easy remembered and leading to early diagnosis and management as all share 1st and 2nd degree burn. This skin problem is rarely mentioned in medical literature including textbooks [1,2]. To the best of our knowledge this is the first solid study that pays attention to this gathering of skin diseases and adding new dermatosis not mentioned before such as thallium poisoning, pellagra and acrodermatitis enteropathica and others. Also new classification was carried out as these diseases can be divided into two groups, the first group includes diseases that almost always present as burn like rash in early course of the disease and they are considered as major causes of burn like lesions, namely pellagra, Stevens-Johnson disease and TEN; zinc deficiency; thallium intoxication; and fixed drug eruption. While the second group includes other miscellaneous conditions that occasionally or rarely present as burn, like during the course of the disease and these include: paederus dermatitis, DLE, hair dye dermatitis, Pemphigus foliaceus, and actinic lichen planus and others. The burn like rash in these diseases might lead to misdiagnosis as this rash is not normally seen in these diseases.
5. Conclusions
Burn- like dermatosis is a distinguished a common diagnostic problem seen in clinical practice where the diagnosis could be easily established as these diseases present as first and second degree- like burn, commonly seen in certain diseases and rarely seen in others. A new classification was done and new list of new differential diagnoses were added that can be very helpful to lead into the diagnosis and management.
Disclosure
This study was an independent study and not funded by any drug companies.
References
| [1] | Atiyeh B.S., Kayle D. I., Nasser A.A. Burn-like syndromes. Annals of Burns and Fire Disasters - vol. XII - n. 1 - March 1999. |
| [2] | O. Castana, M. Makrodimou, D. Michelakis, Z. Tsandoulas, and D. Alexakis. Diseases Mimicking a Burn - Outcome and Treatment. Ann Burns Fire Disasters. 2005 Sep 30; 18(3): 130–132. |
| [3] | Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;7:803–813. https://doi.org/10.1586/eci.11.66. PMid:22014021 Bielsa Marsol I. Update on the classification and treatment of localized scleroderma. Actas Dermosifiliogr. 2013; 104:654–66. |
| [4] | Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome and erythema multiforme. Arch Dermatol. 1993;129:92–96. |
| [5] | Revuz J, Penso D, Roujeau JC, Guillaume JC, Payne CR, Wechsler J, Touraine R, Toxic epidermal necrolysis Clinical findings and prognosis factors in 87 patients. Arch Dermatol. 1987;123:1160–1165. |
| [6] | Mockenhaupt M, Viboud C, Dunant A, Naldi L, Halevy S, Bouwes Bavinck JN, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: assessment of medication riskswith emphasis on recently marketed drugs. The EuroSCAR study. J Invest Dermatol. 2008;128:35–44. |
| [7] | Rojeau JC, Kelly JP, et al. Medication use and the risk of Steven Johnson syndrome or toxic epidermal necrolysis. The New England Journal of Medicine. 1995;333:1600–1608. |
| [8] | Ling YF, Yang CH, et al. Severe cutaneous adverse reactions related to systemic antibiotics. Clinical Infectious Diseases. 2014;58(10):1377–1385. |
| [9] | Sehgal VN, Srivastava G. Fixed drug eruption (FDE): Changing scenario of incriminating drugs. Int J Dermatol. 2006;45:897–908. |
| [10] | Hubiche T, Bes M, Roudiere L, Langlaude F, Etienne J, Del Giudice P. Mild staphylococcal scalded skin syndrome: an underdiagnosed clinical disorder. Br J Dermatol. 2012 Jan. 166(1): 213-5. |
| [11] | Perafa´n-Riveros C, Franc¸ a LF, Alves AC, et al. Acrodermatitis enteropathica: case report and review of the literature. Pediatr Dermatol. 2002;19:426–431. |
| [12] | Sharquie KE, Al-Timimi DJ & Tawffek MAR. Comparison of serum zinc level in healthy children and patients with acrodermatitis enteropathica. J Com Med 1992; 5: 71-2. |
| [13] | Kury S, Dreno B, Bezieau S, et al. Identification of SLC39A4, a gene involved in acrodermatitis enteropathica. Nat Genet. 2002 Jul. 31(3):239-40. |
| [14] | Gutie´rrez-Gonza´lez E, Alvarez-Pe´rez A, Loureiro M, et al. Acrodermatitis enteropathica in a breast-fed infant. Actas Dermosifiliogr. 2012;103:170–172. |
| [15] | Scrivener Y, Bessis D. Dermatoses carentielles. In book: Manifestations dermatologiques des maladies d’organes. Springer-Verlag. 2012;4:45–62. |
| [16] | Sharquie KE, Ibrahim GA, Noaimi AA, Hamudy HK, Outbreak of thallium poisoning among Iraqi patients, Journal of the Saudi Society of Dermatology & Dermatologic Surgery, 2011:15(issue 1);29-32. |
| [17] | Mulkey JP, Oehme FW. A review of thallium toxicity. Vet Hum Toxicol. 1993 Oct. 35(5):445-53. [Medline]. |
| [18] | Saddique A, Peterson CD. Thallium poisoning: a review. Vet Hum Toxicol. 1983 Feb. 25(1):16-22. |
| [19] | Rusyniak DE, Furbee RB, Kirk MA. Thallium and arsenic poisoning in a small midwestern town. Ann Emerg Med. 2002 Mar. 39(3):307-11. |
| [20] | Galvan-Arzate, S., Santamaria, A., 1998. Thallium toxicity. Toxicol. Lett. 99, 1–13. |
| [21] | John Peter, A.L., Viraraghavan, T., 2005. Thallium: a review of public health and environmental concerns. Environ. Int. 31 (4), 493–501. |
| [22] | Desenclos, J.C., Wilder, M.H., Coppenger, G.W., Sherin, K., Tiller, R., Vanhook, R.M., 1992. Thallium poisoning: an outbreak in Florida, 1988. South Med. J. 85, 1203–1206. |
| [23] | Sharquie KE, Al-Hamdi KI, Noaimi AA, Al-Mohammadi AA. Oral zinc sulphate in treatment of patients with thallium poisoning: A clinical therapeutic trial. Journal of Clinical and Experimental Investigation.2011; 2 (2): 133-137. |
| [24] | Oliver FJ, Menissier-de Murcia J, de Murcia G. Poly(ADP-ribose) polymerase in the cellular response to DNA damage, apoptosis, and disease. Am J Hum Genet 1999; 64:1282–8. |
| [25] | Sharquie KE, Rasam S. Pellagra in Alcoholic patients. J. Iraqi Med. Assoc. 1978, 1979; 26, 27: 37-42. |
| [26] | Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol. 2002 Aug. 41(8):476-81. [Medline]. |
| [27] | Stratigos AJ, Antoniou C, Papathanakou E, Daboudi M, Tranaka K, Tsara K, et al. Spectrum of idiopathic photodermatoses in a Mediterranean country. Int J Dermatol. 2003 Jun. 42(6):449-54. |
| [28] | Mammino JJ. Paederus dermatitis: an outbreak on a medical mission boat in the Amazon. J Clin Aesthet Dermatol. 2011; 4(11): 44–46. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML