Najla A. E. Elhaj 1, Heyam S. Ali 2, Hytham Abu-Agla 3, Khalid O. Alfarouk 4, 5, Razaz A. Elbadawi 6, Ahmed N. Aljarbou 7, Abdelhameed Hifny 8, Adil H. H. Bashir 9
1Sudan Medical Specialization Board, Khartoum, Sudan
2Dubai Pharmacy College, Dubai, United Arabic Emirates
3King Fahd Hospital, Al-Madinah Al-Munwarah, KSA
4Alfarouk Biomedical Research LLC, Tampa, FL, United States of America
5Hala Alfarouk Cancer Center, Khartoum, Sudan
6Prince Mohammed Bin Abd Alaziz Hospital, Al-Madinah Al-Munwarah, KSA
7College of Pharmacy, Qassim University, Buraydah, Saudi Arabia
8Al-Azhar University, Cairo, Egypt
9University of Khartoum, Khartoum, Sudan
Correspondence to: Adil H. H. Bashir , University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Diabetes mellitus is a chronic disease caused by inherited and/or acquired deficiency in the production of insulin by the pancreas, or by the ineffectiveness of the insulin produced. The skin is one of the major organ systems involved in diabetes. Almost all diabetic patients eventually develop skin complications from the long-term effects of diabetes mellitus on the microcirculation and skin collagen. Objectives: This study was aimed to detect the clinicoepidemiological prevalence of pruritus in diabetic patients on Jabir Abu Eliz Diabetic Centre. Methodology: It was observational, descriptive, cross-sectional and diabetic center-based study was conducted in the period from August to December 2014 at Jabir Abueliz Diabetes Centre (JADC), including 100 known diabetic patients (Had old and new files), from both sexes who were complaining of itching. The data were collected from patient’s records by questionnaire and analyzed by computer using SPSS. Results: The results of this study showed that diabetic patients who were complaining of pruritus represented 23.3% out of total DM population of Jabir Abueliz Diabetic Center (420) patients, 100 diabetic patient detected to suffer from pruritus where males represented 42 (42.0%), and females were 58 (58.0%). The majority 67 represented (67.0%) belonged to the age group 26-60 years, followed by 32 patients (32.0%) in the age group >60 years and only 1 patient (1.0%) in the age group 14-25 years. It was noticed that 94.0% of patients had type 2 diabetes mellitus, while 3 patients represented 3.0% had type 1, two patients (2.0%) had gestational diabetes and 1 patient (1.0%) had secondary diabetes. It was found that 92% had years duration, while 5% had a month’s duration and 3% had a duration for days. Duration of itching was months in 56%, years in 22% and days in 22%. Distribution of itching was localized in 61.0% of patients and widespread in 39% of patients. Other symptoms associated with itching were an eruption in 29.0%, dark pigmentation associated with an eruption in 10.0%, dryness, and eruption in 8.0% and dryness per se in 7.0% patients. Pruritis was common in summer 16.0%, 15 patients represented (15.0%) in winter. Aggravating factors of itching were found to be dryness 13.0%, sun exposure (9.0%) and moisture (4.0%). Relieving factors were detected in 11.0% patients, (18.0%) had lesions in lower limbs, (5.0%) in genitalia, (3.0%) in trunk, and (2.0%) in scalp, flexural areas face and neck. It was observed that 18.0% of patients had papule, vesicle, and pustule, while ten patients represented (10.0%) had papules and scales. 4 patients (4.0%) had papule and crust, 3 patients (3.0%) had scales. Conclusion: The prevalence of pruritus in diabetic patients on Jabir Abu Eliz Diabetic Centre was 23.3% (100 patients), found to be 42.0% of them were males and 58.0% were females. The clinical features of pruritus in diabetic patients in this study were an eruption, dark pigmentation, and dryness (29%), 3%, and 7%) respectively. Localized pruritus that attributed to diabetes was the most common among the study population.
Keywords:
DM, Pruritus, Sudan
Cite this paper: Najla A. E. Elhaj , Heyam S. Ali , Hytham Abu-Agla , Khalid O. Alfarouk , Razaz A. Elbadawi , Ahmed N. Aljarbou , Abdelhameed Hifny , Adil H. H. Bashir , The Prevalence of Pruritus among Sudanese Patients with Diabetes Mellitus, American Journal of Dermatology and Venereology, Vol. 8 No. 5, 2019, pp. 73-83. doi: 10.5923/j.ajdv.20190805.01.
1. Introduction
Diabetes mellitus (DM) is a group of metabolic diseases characterized by high blood sugar (glucose) levels that result from deficiency in insulin secretion, or its action, or both. In ancient times, diabetes mellitus, commonly known as diabetes, was identified as a disease linked to the appearance of glucose in urine and extreme muscle loss [1,2].There are three types of diabetes mellitus are:• Type 1 diabetes mellitus, where there is a lack of insufficient insulin production by the body.• Type 2 diabetes mellitus in which the cells become resistant to insulin. This type may be associated with initially normal or increased levels of circulating insulin.• Gestational diabetes: This type is only associated with pregnancy. The prevalence of gestational diabetes is 4% of all pregnant women. It may precede the development of type 2 or rarely type 1 diabetes [3].Pruritus or itch is defined as the urge to scratch. It is an associated with many skin diseases and is an unusual symptom of some systemic diseases. The followings are features of pruritus: local or general and acute or chronic. Chronic pruritus is a term coined for Itching lasting more than 6 weeks. Itching can be problematic and debilitating, as well as it can be a diagnostic and therapeutic challenge [4].Itching is is associated with dermatologic and systemic disorders. Because it results in poor blood circulation, diabetes is one of the systemic disorders associated with itching, particularly in the lower limbs. Moreover, diabetic itching is often caused by dry skin, a situation easily manageable by self-care. The characteristic rash may be taken as a diagnosis of a primary dermatologic disorder. As a matter of fact, some skin diseases are associated with pruritus [4,5].Stress is a precipitating factor in itching; its management should be a prime concern in the treatment of itching. Psychiatric help maybe the need for better management of stress., which is characteristic of this disease. Morbid disease situations associated with diabetic itching include fungal infections such as ringworm or athlete's foot and allergic reactions to medications, including insulin [6,7].
2. Objectives
General Objective:To detect the Clinicoepidemiological prevalences of pruritus in diabetic patients on Jabir Abu Eliz Diabetic Centre. Specific objectives:§ To detect the prevalence and clinical features of pruritus in diabetic patients.§ To determine the severity of pruritus among different groups of diabetic patients.
3. Results
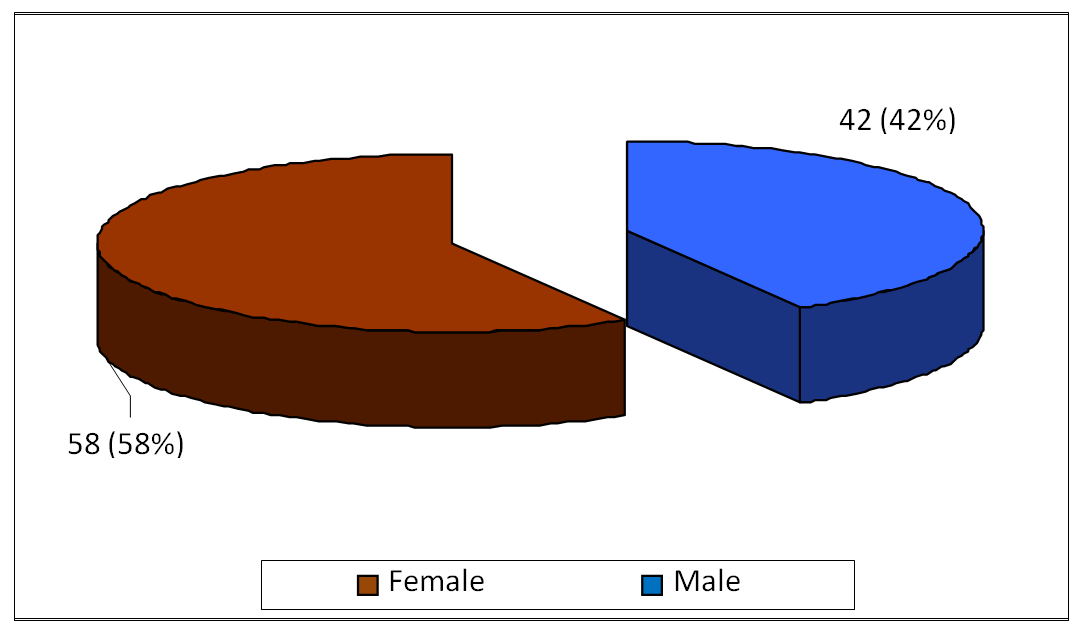
The diabetic patients who had dermatological problems without itching were 429 patients. It was included 100 diabetic patients complaining of pruritus (23.3%), males were 42 represented (42.0%), and females were 58 (58.0%) as shown in (Figure 1).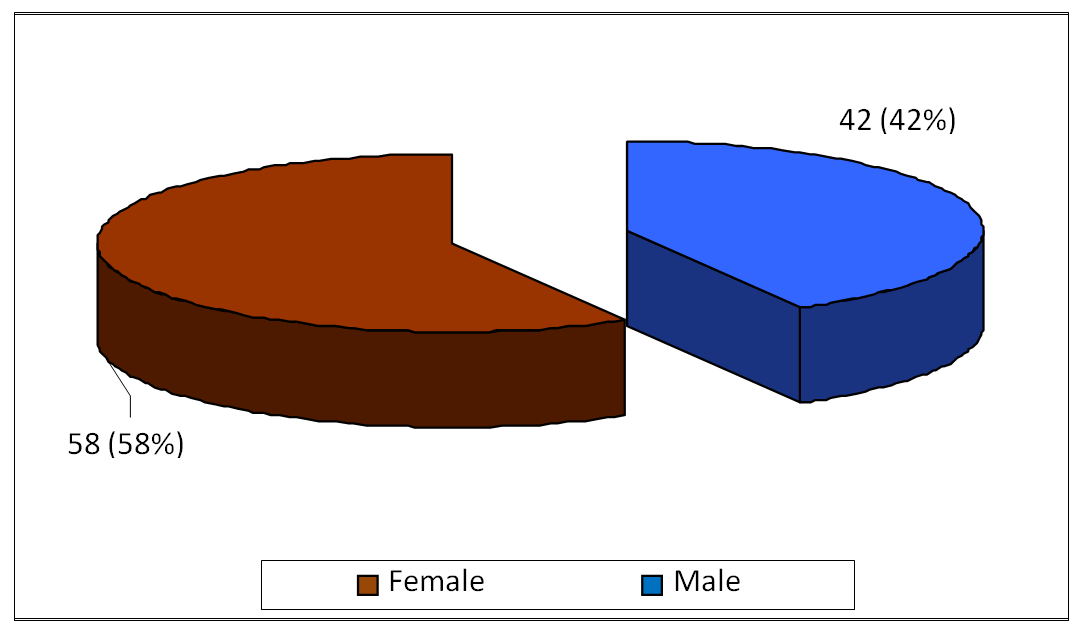 | Figure 1. Showed that Gender in pruritus in DM in period (August –December) 2014 |
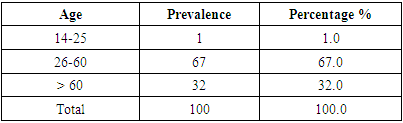
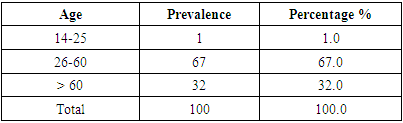
Most of the study population 67 patients represented (67.0%) were belong to age group 26-60 years, followed by 32 patients (32.0%) in the age group >60 years and only 1 patient (1.0%) in the age group 14-25 years (Table 1). Table 1. Showed that Age in pruritus in DM in period (August-December) 2014
 |
| |
|
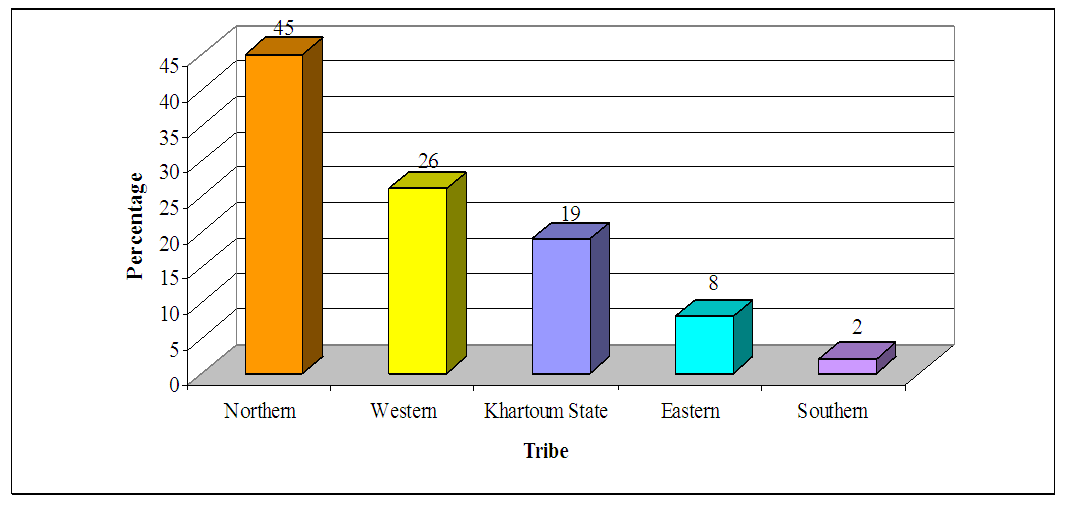
Distribution of the study population according to tribes, 45 patients represented (45.0%) from northern tribes, 26 patients (26.0%) from western, 19 patients (19.0%) from Khartoum State, 8 patients (8.0%) from eastern, and 2 patients (2.0%) from southern tribes, (Figure 2).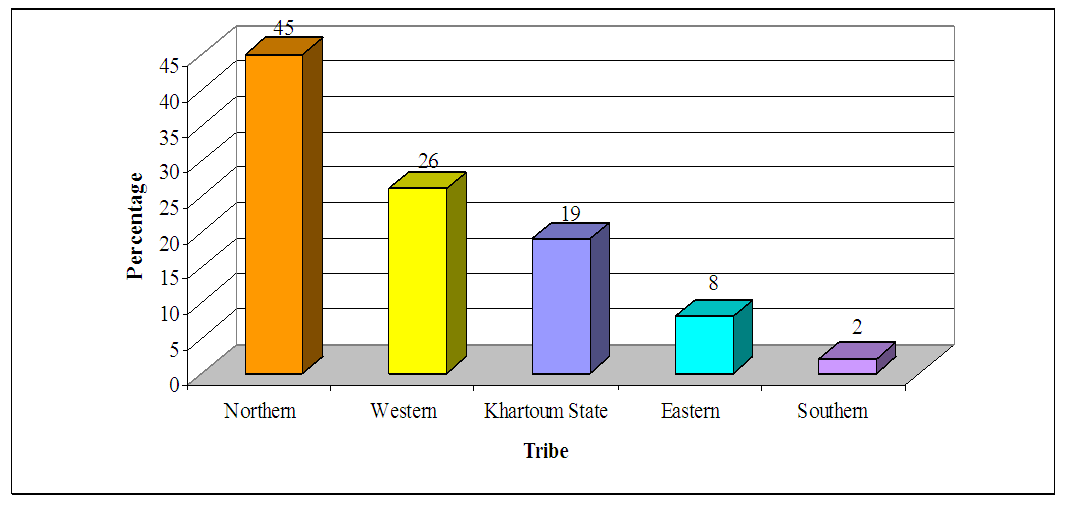 | Figure 2. Showed that Tribes in pruritus in DM in period (August – December) 2014 |
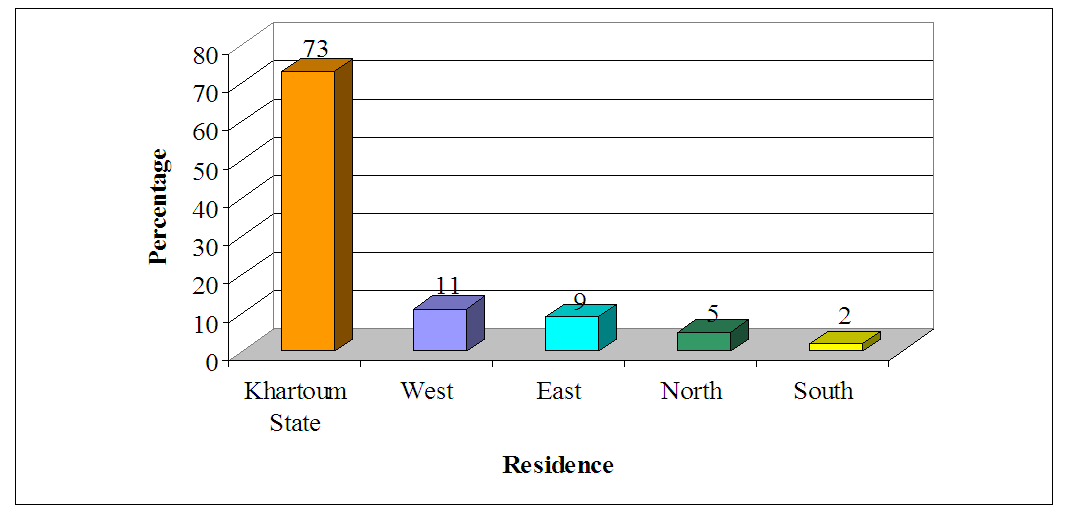
Residence of the study population showed that, 73 patients represented (73.0%) resided Khartoum State, 11 patients (11.0%) in west, 9 patients (9.0%) in East, 5 patients (5.0%) in north and 2 patients (2.0%) in south (Figure 3).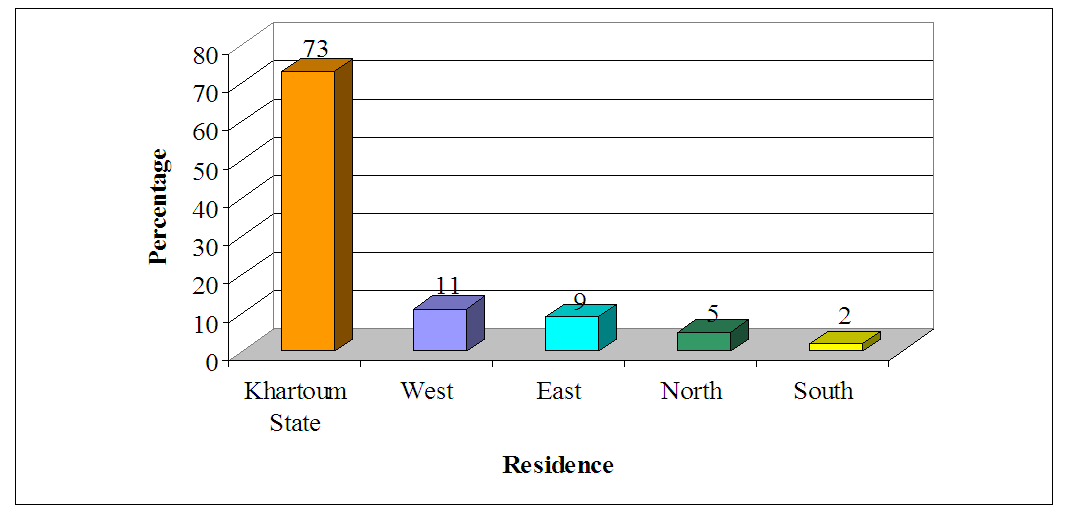 | Figure 3. Showed that Residence in pruritus in DM in period (August- December) 2014 |
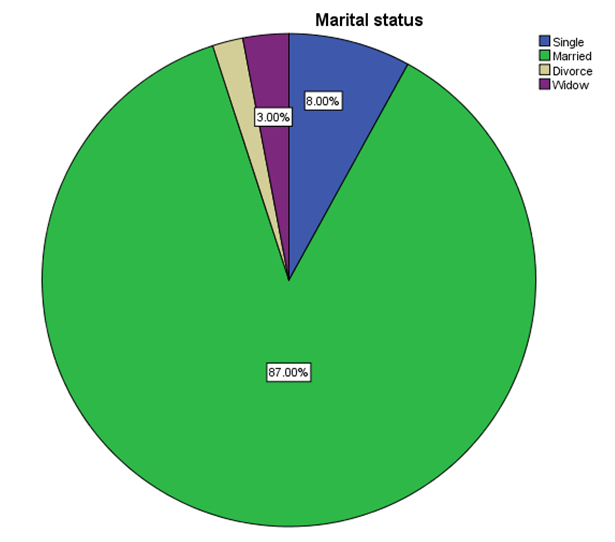
Most of the study population 87 patients represented (87.0%) were married, 8 patients (8.0%) single, 3 patients (3.0%) widow and 2 patients (2.0%) were divorce (Figure 4).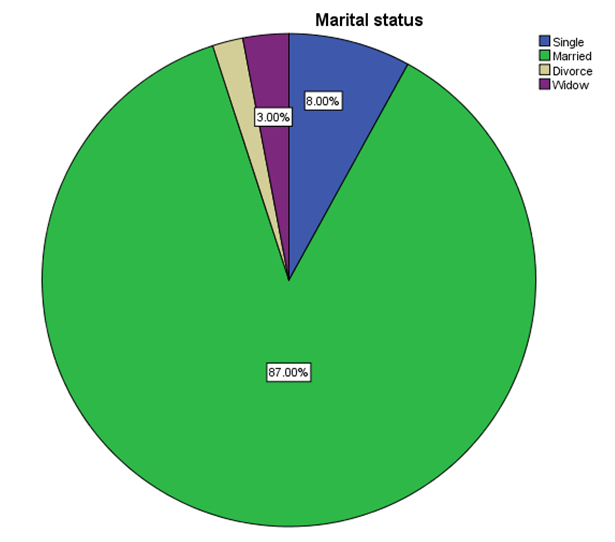 | Figure 4. Showed that Marital status in pruritus in DM in period (August-December) 2014 |
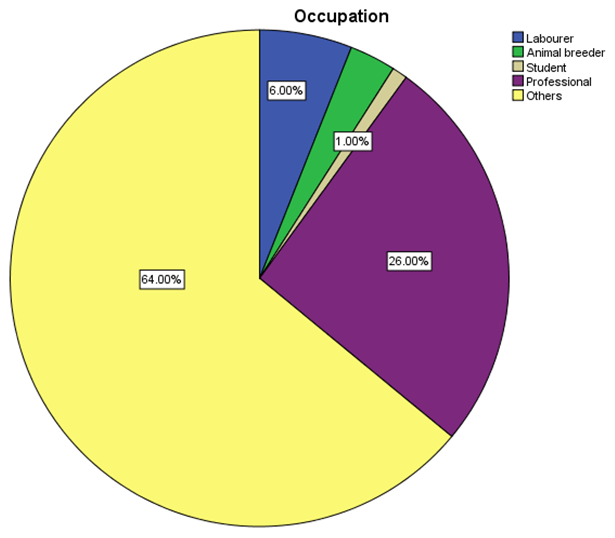
(Figure 5), occupations of the study population, showed that 26 patients represented (26.0%) were professionals, six patients (6.0%) laborer, three patients (3.0%) animal breeder, and one patient (1.0%) student and others category was 64%. 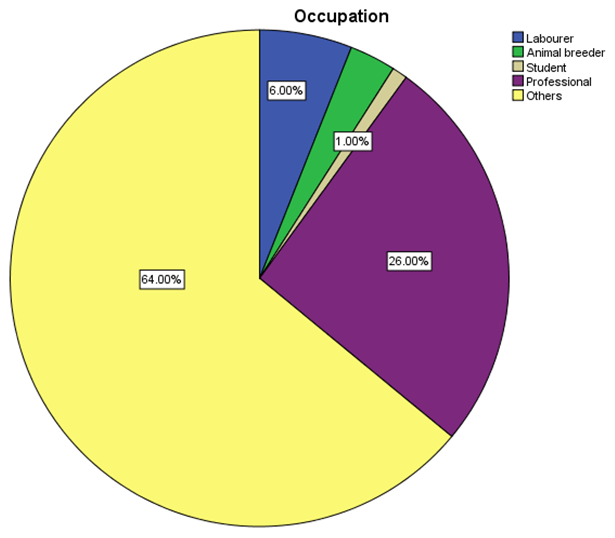 | Figure 5. Showed that Occupation in pruritus in DM in period (August- December) 2014 |
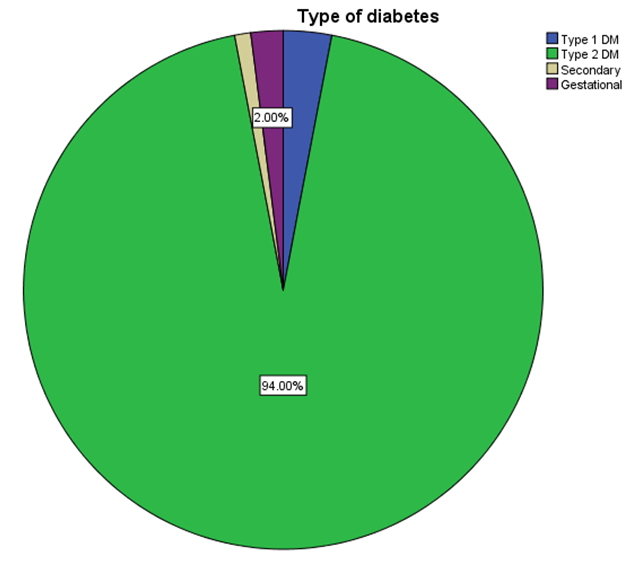
Most of the study population 94 patients represented (94.0%) had type 2 diabetes mellitus, 3 patients (3.0%) had type 1, two patients (2.0%) had gestational diabetes and 1 patient (1.0%) had secondary diabetes (Figure 6).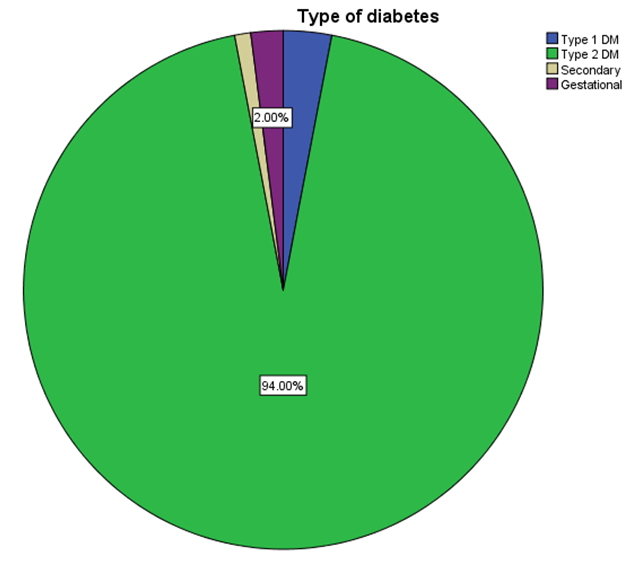 | Figure 6. Showed that Types of DM in the patient of pruritus in period (August-December) 2014 |
Concerning the duration of Diabetes Mellitus among the study population, 92 patients represented (92%) had a duration of years, five patients (5%) had a duration of months, and three patients (3%) had a duration of days (Figure 7). | Figure 7. Showed that Duration of DM in the patient of DM with pruritus in period (August-December) 2014 |
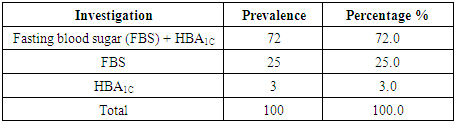
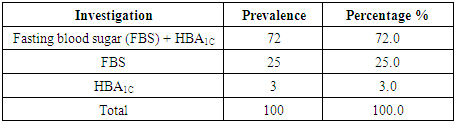
Investigations related to Diabetes Mellitus that performed for the study population, where fasting blood sugar (FBS + HBA1c) was performed for 72 patients represented (72.0%), FBS for 25 (25.0%) and HbA1c for 3 (3.0%) as shown in (Table 2).Table 2. Showed that Investigation related to DM in pruritus in period (August-December) 2014
 |
| |
|
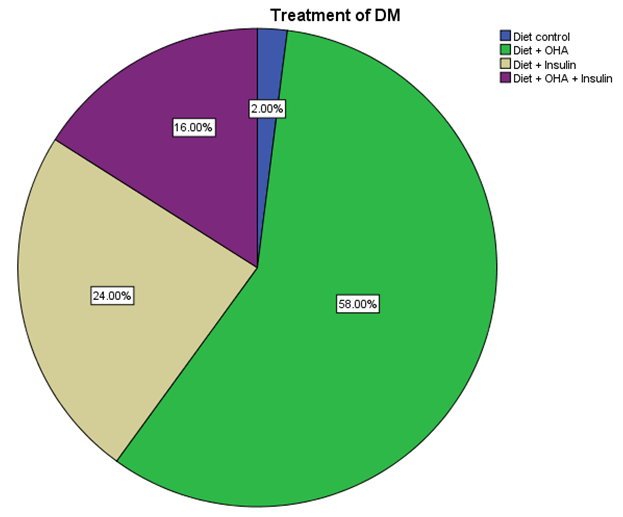
Regarding treatment received by the study population, 58 patients represented (58.0%) received treatment in form of diet + OHA, 24 patients (24.0%) diet + insulin, 16 (16.0%) diet + OHA + insulin and 2 patients (2%) on diet control alone (Figure 8).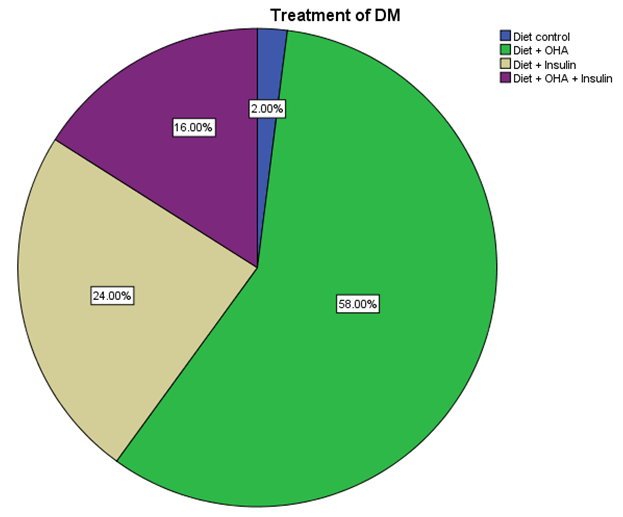 | Figure 8. Showed that Treatment of DM in the patient of DM with pruritus in period (August-December) 2014 |
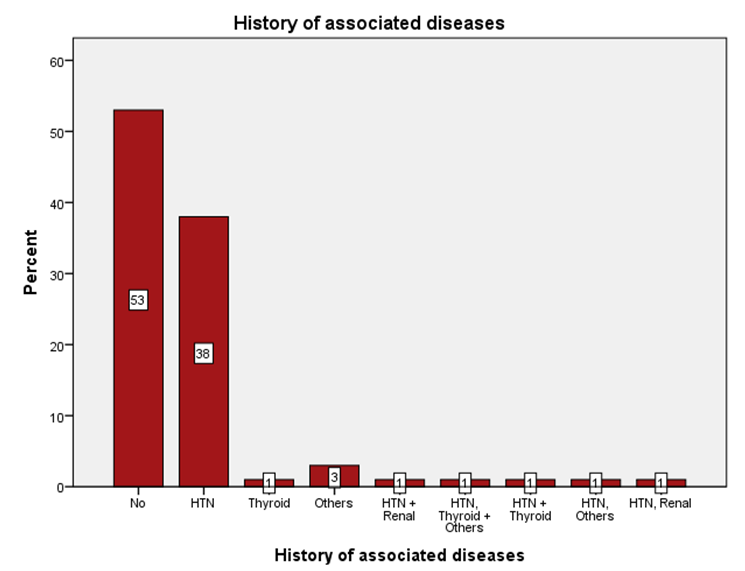
History of associated Diabetes Mellitus among the study population showed that 53 patients represented (53%) had no associated diseases, 38 patients (38%) had hypertension, one patient (1%) had thyroid, three patients (3%) had other diseases (Figure 9).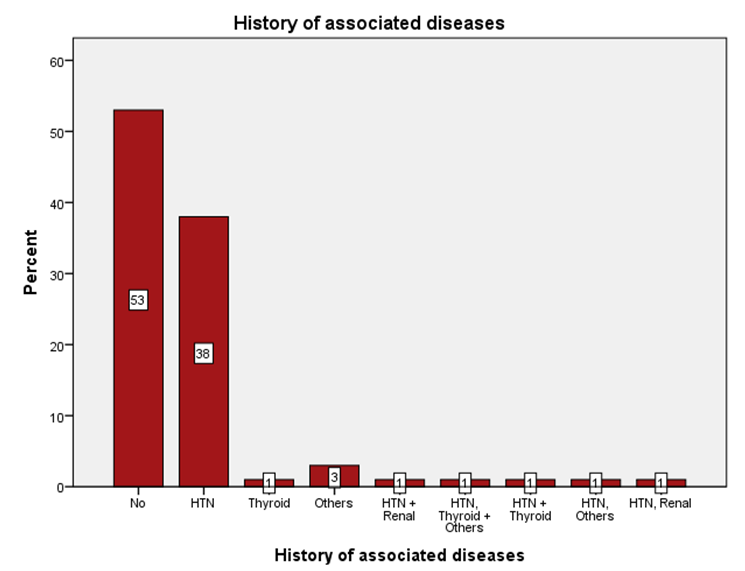 | Figure 9. Showed that Associated diseases with DM in the patients of DM with pruritus in period (August-December) 2014 |
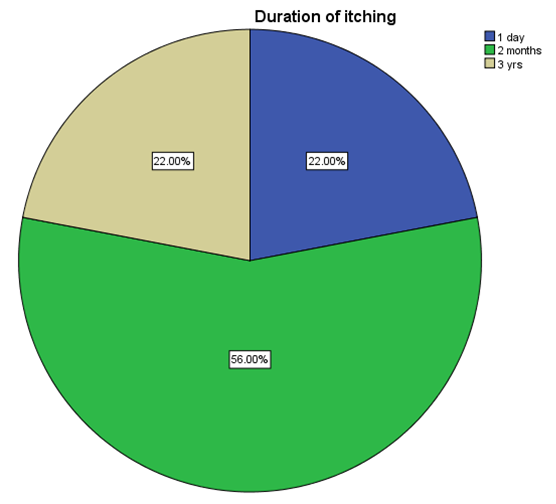
Duration of itching among the study population was as follow, 56 patients represented (56%) had a duration of months, 22 (22%) had a duration of years, 22 (22%) had a duration of days (Figure 10).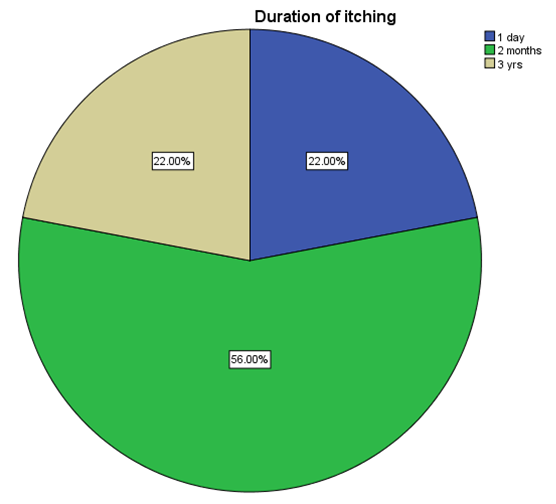 | Figure 10. Showed that Duration of itching in the patient of DM with pruritus in period (August-December) 2014 |
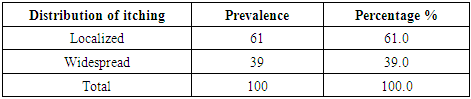
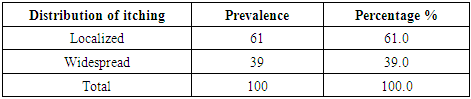
Distribution of itching, in 61 patients represented (61.0%) localized and in 39 (39%) patients, it was widespread (Table 3).Table 3. Showed that Distribution of itching in the patient of DM with pruritus in period (August-December) 2014
 |
| |
|
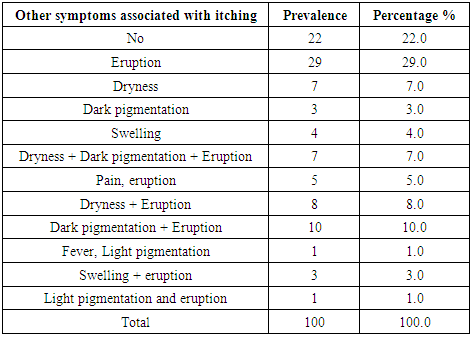
Other symptoms associated with itching among the study population were eruption in 29 patients represented (29.0%), dark pigmentation with eruption in 10 (10.0%) patients, dryness with eruption in 8 (8.0%) patients, dryness alone in 7 (7.0%) patients and 22 patients (22.0%) had no associated symptoms (Table 4). Table 4. Showed that Other symptoms associated with itching in the patient of DM with pruritus in period (August-December) 2014
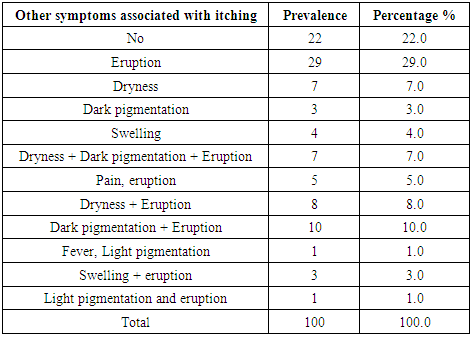 |
| |
|
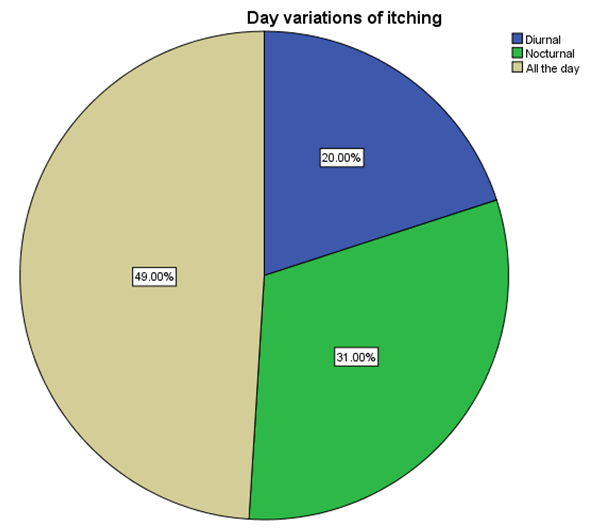
Figure 11: Showed day variations of itching; the majority of the study population 49 patients represented (49.0%) had all day itching, 31 (31.0%) had nocturnal itching, and 20 (20.0%) patients had diurnal itching. 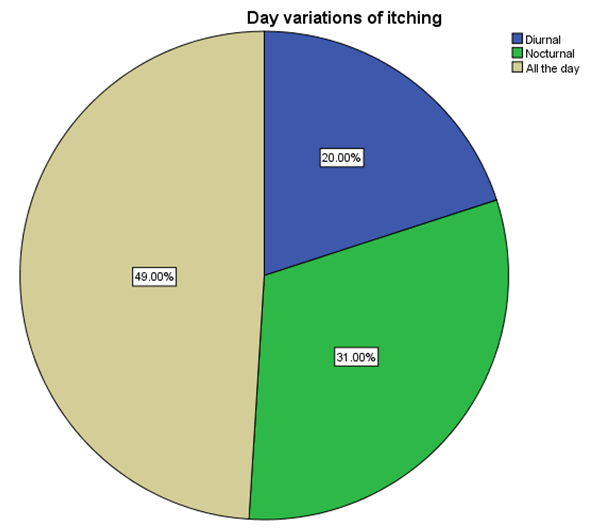 | Figure 11. Showed that Day variation of itching in the patient of DM with pruritus in period (August-December) 2014 |
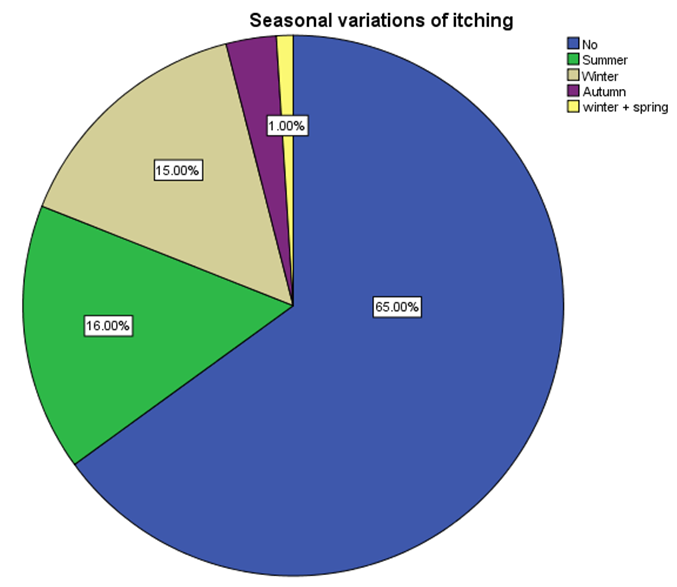
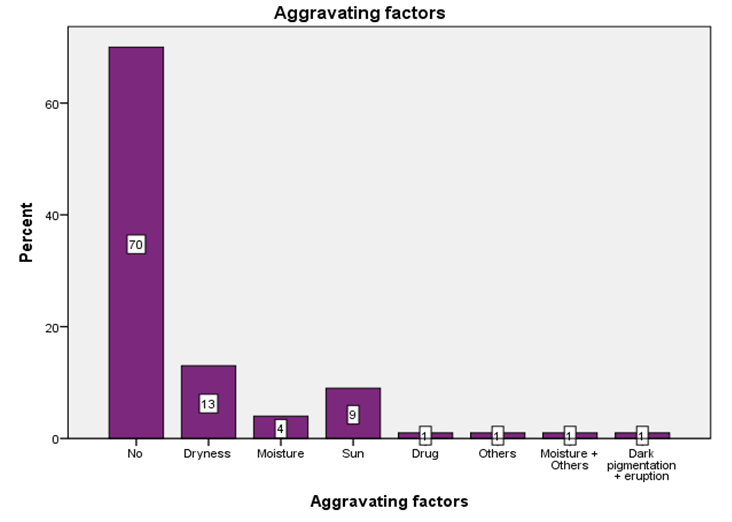
Figure 12: Showed seasonal variations of itching, in the majority of the study population 65 (65.0%) had no seasonal variations, while itching increased in 16 patients (16.0%) in Summer, 15 patients (15.0%) in Winter, 3 patients (3.0%) in Autumn and 1 patient (1.0%) in spring. Aggravating factors of itching among the study population were dryness in 13 patients represented (13.0%), sun in 9 patients (9.0%), moisture in 4 patients (4.0%) , drugs in 1 patient (1.0%) and in 70 patients (70.0%) there is no aggravating factors (Figure 13).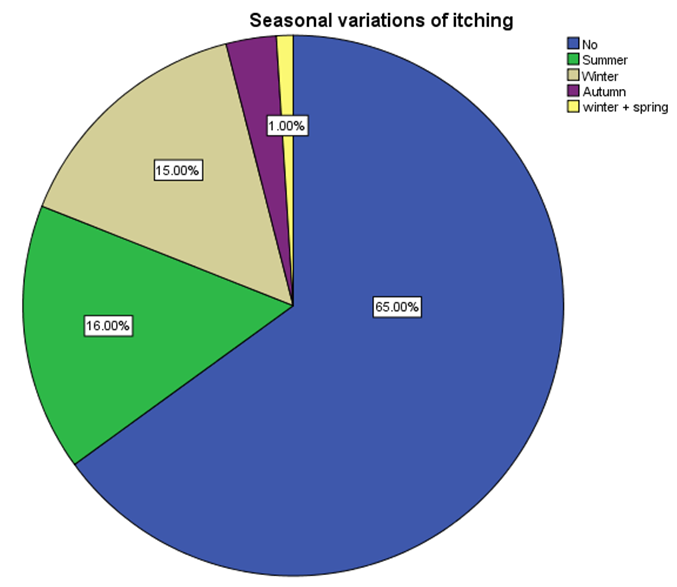 | Figure 12. Showed that Seasonal variation of itching in the patient of DM with pruritus in period (August-December) 2014 |
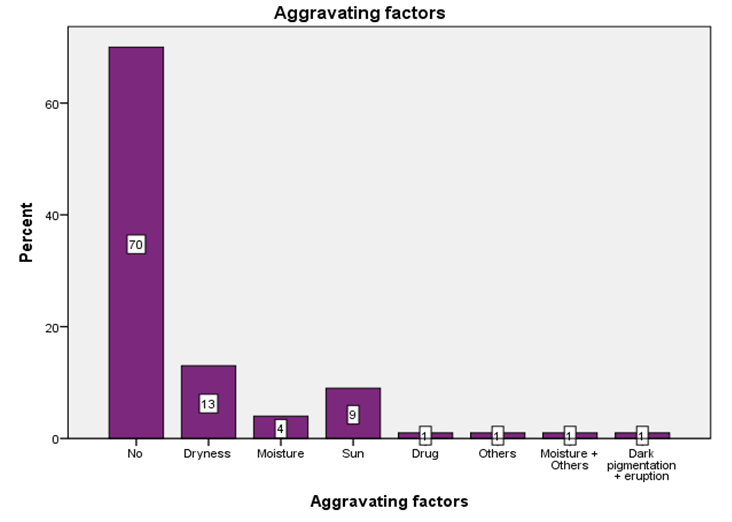 | Figure 13. Showed that Aggravating factors of itching in the patient of DM with pruritus in period (August-December) 2014 |
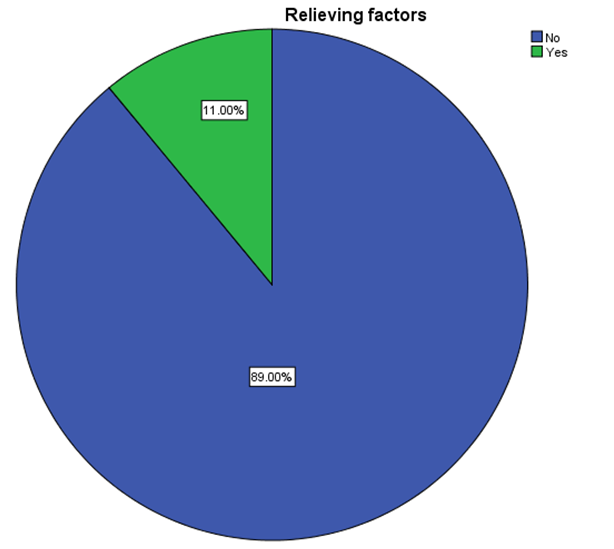
In 89 patients represented (89.0%), there were no relieving factors of itching, but in 11 patients (11.0%) have relieving factors, most of them (Figure 14).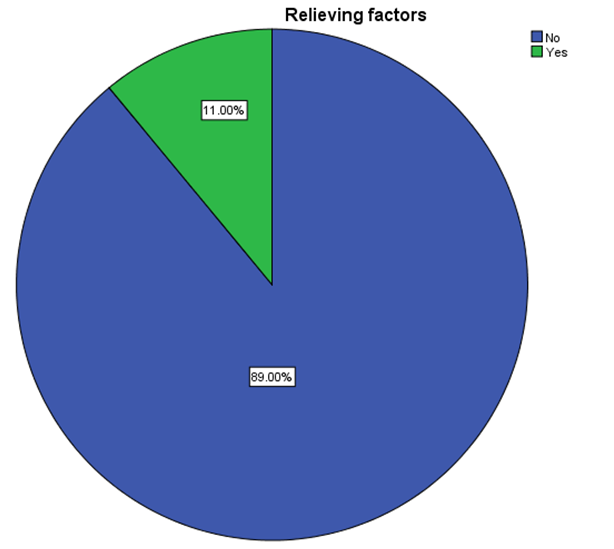 | Figure 14. Showed that Relieving factors of itching in the patient of DM with pruritus in period (August-December) 2014 |
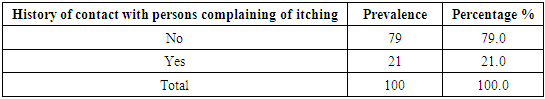
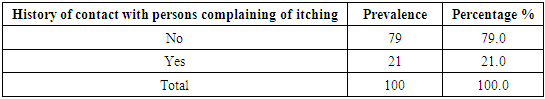
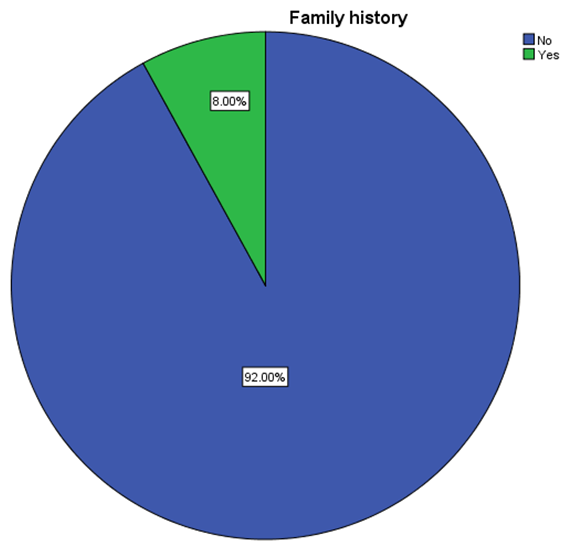
Figure 15: Showed family history of pruritus, in 92 patients represented (92.0%), there is no family history in 8 patients (8.0%), 21 (21.0%) patients had history of contact with persons complaining of itching and no history of contact in 79 patients 79.0% (Table 5).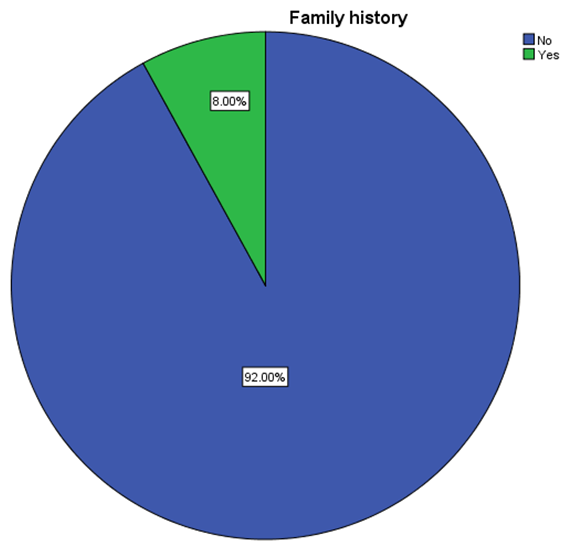 | Figure 15. Showed that Family history of pruritus in DM in period (August-December) 2014 |
Table 5. Showed that History of contact with persons complaining of itching in the patient of DM with pruritus in period (August-December) 2014
 |
| |
|
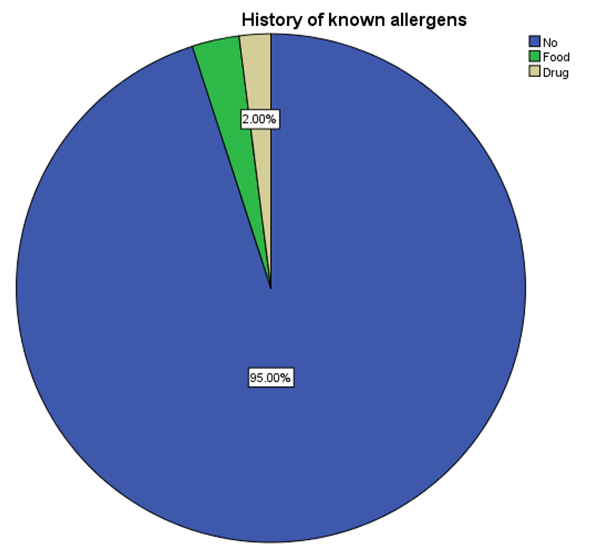
It was noticed that three patients represented (3.0%) patients had a history of known food allergens, 2 (2.0%) patients had a history of known drug allergen and in 95 patients (95.0%) had no history of known allergen or drug as showed in (Figure 16).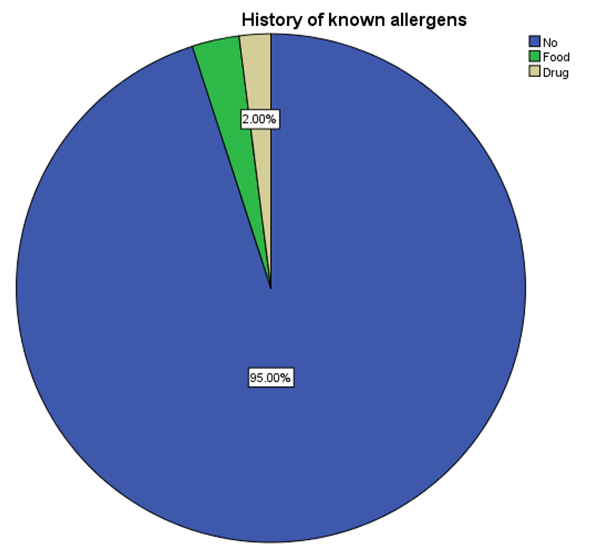 | Figure 16. Showed that History of known allergens in patients of DM with pruritus in period (August-December) 2014 |
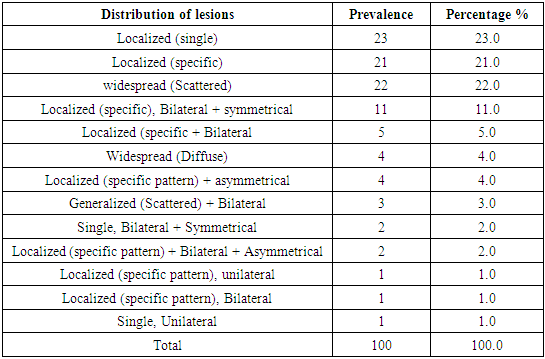
Table 6: Showed distribution of lesions, localized in 23 patients represented (23.0%), widespread (Scattered) in 22 (22.0%) patients.Table 6. Showed that Distribution of the lesions in pruritus in DM in period (August-December) 2014
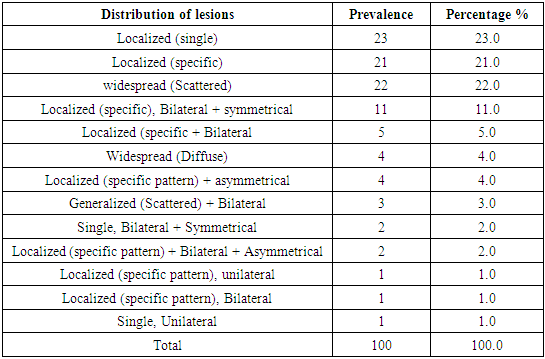 |
| |
|
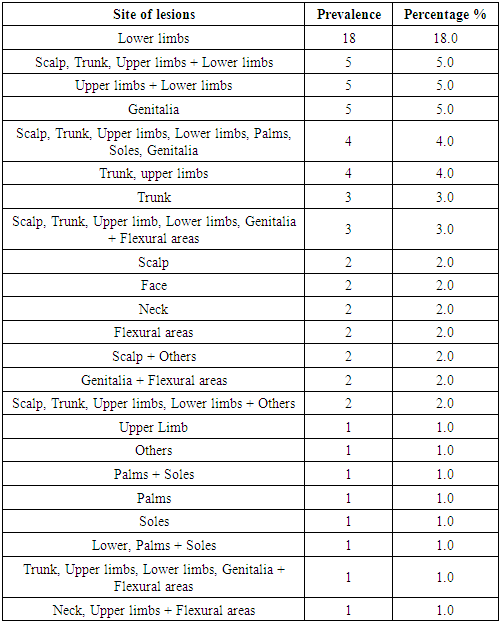
Table 7: Showed distribution of site of lesions in the study population, 18 patients represented (18.0%) had lesions in lower limbs, 5 (5.0%) had lesions in genitalia, 3 (3.0%) in trunk, 2 (2.0%) patients had lesion in scalp, flexural areas, face, and neck. Table 7. Showed that Site of lesions in pruritus in DM in period (August-December) 2014
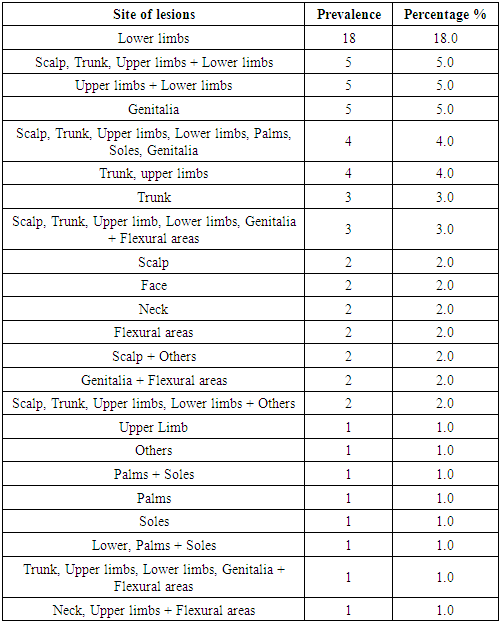 |
| |
|
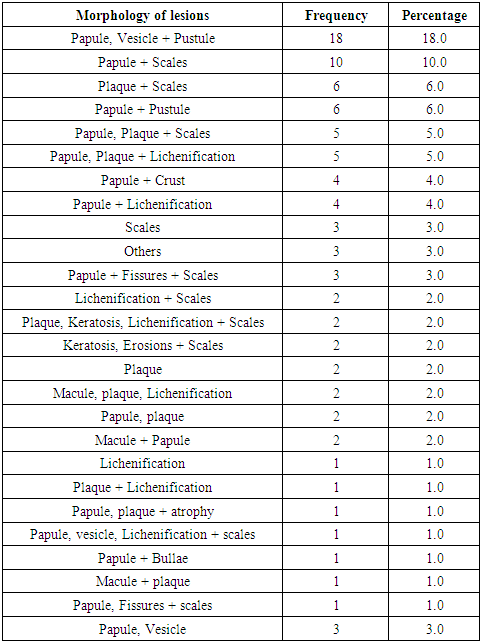
Table 8: Showed morphology of the lesions among the study population, 18 patients represented (18.0%) patients had papule, vesicle and pustule, 10 (10.0%) patients had papule and scales. 6 patients (6.0%) had plaque with scales and plaque with pustule, 5 patients (5.0%) had papule, plaque with scales or lichenification, 4 (4.0%) patients had papule with crust or lichenification, and 3 (3.0%) patients had scales alone.Table 8. Showed that Morphology of lesions in pruritus in DM in period (August-December) 2014
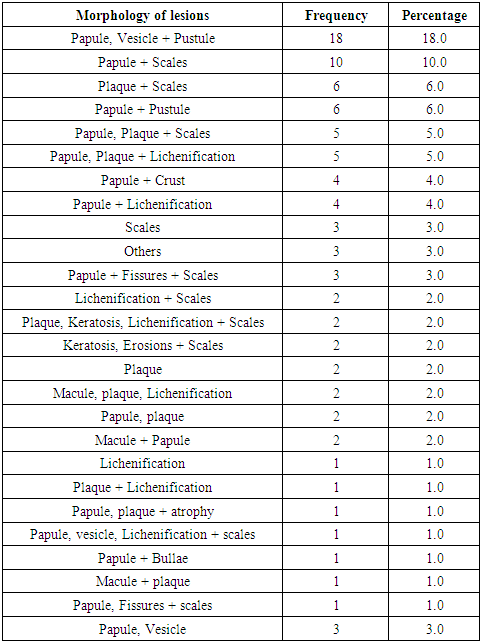 |
| |
|
4. Discussion
In this study which aimed to detect the Clinicoepidemiological prevalence of pruritus in 100 diabetic patients at Jabir Abu Eliz Diabetic Centre, 2014; males were 42 (42.0%), and females were 58 (58.0%). This, in contrast with the previous study conducted by Harish et al., which stated that males were predominant, 88(64.7%) and 48 (35.3%) were females [8]. Most of the study population 67 (67.0%) were in the age group 26-60 years, followed by 32 patients (32.0%) in the age group >60 years. This coincided with the previous study, which reported that the maximum numbers of patients were in the age group of 51 to 60 years (32.36%) [8]. This can be explained by the fact that the increase of cutaneous involvement of Diabetes Mellitus may be attributed to the long duration of diabetes in this age group of patients.In this study, 87 patients (87.0%) were married. According to the finding of Anna S, 2003 which is five focus interviews; who reported that vaginal dryness and pain during intercourse are problems may find in type 2 DM, these predisposing factors may result into injury and so vaginal thrush [9].Twenty-six patients (26.0%) were professionals. This result on conformity with the study of Kyoko et al., 2007 [10], who assessed the association between job stress and somatic symptoms and their correlation with co-morbidities like diabetes and they found that skin itching is one of the somatic symptoms.Most of the study population (94.0%) had type 2 Diabetes Mellitus, and (3.0%) had type 1. This was like that found in a previous study [10], which showed that type 2 DM seen in 130 (95.6%) patients and 6 (4.4%) patients had type 1 DM [8].The majority of patients in these studies (92%) had duration of diabetes for years, this was similar to Bhat et al., 2006, Ahmed et al., in their studies, this Can be explained by the fact that as the duration of diabetes increased, there was non-enzymatic glycosylation of dermal collagen and mucopolysaccharides, leading to various dermatological manifestations and complications included pruritus [11,12].A previous study, Bhat et al., showed a positive association between postprandial blood glucose and generalized pruritus and suggested that better control of postprandial glucose might be beneficial to relieve generalized pruritus in diabetic patients [11,13]. Therefore, in this study, fasting blood sugar and HbA1c was measured for (72.0%) of the study population, FBS for 25 (25.0%), also HbA1c for 3 (3.0%).History of associated diseases among the study population showed that (38%) had hypertension, (1%) had thyroid, and (3%) had others. This coincided with previous literature of Palot et al., 2008, which reported that hypothyroidism, chronic lymphocytic leukemia, hepatitis C, hepatitis B, diabetes mellitus, lung cancer, and uremia were associated with pruritus in diabetic patients [14].In this study, 61% of patients had localized pruritus, and 39.0% had widespread pruritus that attributed to diabetes, which indicates a high rate of pruritus than that was reported in 10% of the people with diabetes by Mahajan et al., 2003 [15], and in 4.5% by Nigam et al., 2003 [16].Other symptoms associated with pruritus among the study population were eruption (29.0%), dark pigmentation associated with an eruption in (10.0%) patients, dryness with eruption (8.0%) patients, dryness (7.0%). This online with a literature review which stated that other symptoms associated were the presence of xerotic skin, a feature which can predispose to pruritus [17]. Also, in this study, more aggravating factors of itching were dryness (13.0%).The seasonal variations of itching, 65.0% of study population itching not associated with seasonal, while in 16 (16.0%) in summer, 15 (15.0%) in winter. This finding indicates that the onset of itching is not seasonal-dependent and may attribute to other factors like low immunity and diminished peripheral circulation in diabetic patients. In this study, Pruritus of the scalp was 2%, whereas Scribner, 1977 recognized it as a predominant manifestation of diabetes and is usually resistant to antipruritic measures [18].In this study most of the patients had lesions in lower limbs, where these sites represent location of fungal infection like Tinea Pedis, this coincided with the local study of Bashir et al., 2004 [19], but in contrast with the local study where Candidal Vulvo Vaginitis was 12%, only 5% had lesions in genitalia in this study, while the distribution of lesions was localized in 23 patients represented (23.0%) included local insulin reaction, that similar to local study of Bashir et al., 2004 [19].
5. Conclusions
The prevalence of diabetic patients who were complaining of itching on Jabir Abu Eliz Diabetic Centre was 23.3% represented as 42.0% in males and 58.0% females. The main clinical features of pruritus in diabetic patients in this study were an eruption, dark pigmentation, and dryness. Localized pruritus that attributed to diabetes was common among the study population represented 23%.
6. Recommendations
§ Control and intensive management of Diabetes Mellitus to prevent dermatological complications, specifically pruritus, are highly recommended.§ Rising awareness of patients and relatives about seeking treatment for pruritus early in order to improve the quality life of patients with Diabetes Mellitus and to avoid more complications.§ Availability of anti/reliving pruritus agents at clinics and centers of Diabetes Mellitus treatment is mandatory.§ Further studies are needed for assertion more about the correlation of pruritus as dermatological manifestations per se among Diabetes Mellitus patients.
ACKNOWLEDGEMENTS
This work is supported partially by Orchid Life, LLC. We thank Linda Aurdal Wales for the nice discussion on topics.
References
| [1] | Ferringer, T.; Miller, F. Cutaneous manifestations of diabetes mellitus. Dermatol Clin 2002, 20, 483–92. |
| [2] | Duff, M.; Demidova, O.; Blackburn, S.; Shubrook, J. Cutaneous Manifestations of Diabetes Mellitus. Clin Diabetes 2015, 33, 40. |
| [3] | Dunger, D. B.; Todd, J. A. Prevention of type 1 diabetes: what next? Lancet 2008, 372, 1710–1711. |
| [4] | Grundmann, S.; Ständer, S. Chronic pruritus: clinics and treatment. Ann Dermatol 2011, 23, 1–11. |
| [5] | Nowak, D. A.; Yeung, J. Diagnosis and treatment of pruritus. Can Fam Physician 2017, 63, 918–924. |
| [6] | Nakatani, K.; Kurose, T.; Hyo, T.; Watanabe, K.; Yabe, D.; Kawamoto, T.; Seino, Y. Drug-induced generalized skin eruption in a diabetes mellitus patient receiving a dipeptidyl peptidase-4 inhibitor plus metformin. Diabetes Ther 2012, 3, 14. |
| [7] | Badik, J.; Chen, J.; Letvak, K.; So, T.-Y. Hypersensitivity Reaction to Insulin Glargine and Insulin Detemir in a Pediatric Patient: A Case Report. J Pediatr Pharmacol Ther 2016, 21, 85–91. |
| [8] | Harish MR, S. B. Association of Dermatoses with Diabetes-A Case Control Study. WebmedCentral DERMATOLOGY 2012, 3, 1–8. |
| [9] | Sarkadi, A.; Rosenqvist, U. Intimacy and Women With Type 2 Diabetes: An Exploratory Study Using Focus Group Interviews. Diabetes Educ 2003, 29, 641–652. |
| [10] | Nomura, K.; Nakao, M.; Sato, M.; Ishikawa, H.; Yano, E. The Association of the Reporting of Somatic Symptoms with Job Stress and Active Coping among Japanese White-collar Workers. J Occup Health 2007, 49, 370–375. |
| [11] | Bhat, Y. J.; Gupta, V.; Kudyar, R. P. Cutaneous manifestations of diabetes mellitus. Int J Diab Dev Ctries 2006, 26, 152–155. |
| [12] | Ahmed, K.; Muhammad, Z.; Qayum, I. Prevalence of cutaneous manifestations of diabetes mellitus. J Ayub Med Coll Abbottabad 21, 76–9. |
| [13] | Ko, M.-J.; Chiu, H.-C.; Jee, S.-H.; Hu, F.-C.; Tseng, C.-H. Postprandial blood glucose is associated with generalized pruritus in patients with type 2 diabetes. Eur J Dermatol 23, 688–93. |
| [14] | Polat, M.; Öztas, P.; İlhan, M. N.; Yalçin, B.; Alli, N. Generalized pruritus: a prospective study concerning etiology. Am J Clin Dermatol 2008, 9, 39–44, doi:10.2165/00128071-200809010-00004. |
| [15] | Mahajan, S.; Koranne, R. V; Sharma, S. K. Cutaneous manifestation of diabetes mellitus. Indian J Dermatol Venereol Leprol 69, 105–8. |
| [16] | Nigam, P. K.; Pande, S. Pattern of dermatoses in diabetics. Indian J Dermatol Venereol Leprol 69, 83–5. |
| [17] | DiGiovanna, J. J.; Robinson-Bostom, L. Ichthyosis: etiology, diagnosis, and management. Am J Clin Dermatol 2003, 4, 81–95, doi:10.2165/00128071-200304020-00002. |
| [18] | Scribner, M. Diabetes and pruritus of the scalp. JAMA 1977, 237, 1559. |
| [19] | Bashier, A. H.; Kordofani, Y. M. Clinico-epidemiological study of cutaneous manifestations of diabetes mellitus in Sudanese patients. Sudan J Dermatology 2005, 2, 54–60, doi:10.4314/sjd.v2i2.32842. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML