-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(4): 55-60
doi:10.5923/j.ajdv.20190804.01

Granulomatous Reaction at the Site of Positive Tuberculin Skin Test is a Marker of Active TB (Clinical and Histopathological Study)
Khalifa E. Sharquie1, 2, Adil A. Noaimi1, Fatima A. Khalaf3
1Department of Dermatology, College of Medicine, University of Baghdad, Iraq
2Iraqi and Arab Board for Dermatology and Venereology, Center of Dermatology and Venereology, Medical City, Baghdad, Iraq
3Center of Dermatology and Venereology, Medical City, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

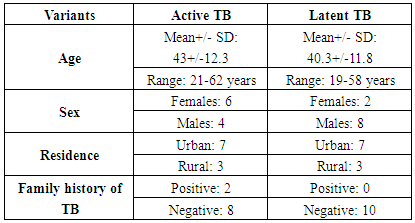
Background: Medical authorities all over the world did not pay much attention to diagnostic value of positive tuberculin test but our observation suggest that the tuberculin test with histopathological evaluation could be very helpful in establishing clinical diagnosis of tuberculosis (TB) without the essential need for other diagnostic tools. Objective: To study all positive tuberculin reaction and to do histopathological examination in order to get objective findings in that are helpful for clinical diagnosis of TB. Patients and Methods: This is descriptive and histopathological study, carried out in Center of Dermatology and Venereology, Baghdad Teaching Hospital from January 2017 to January 2018. Twenty patients were enrolled in the current study, their ages ranged between 19-62(53.32 +/- 11.9) years, full history taken including personal or family history of pulmonary or extra-pulmonary TB, BCG vaccination, and the measurement of TST as had carried out in The Specialist National Center for Pulmonary Diseases and those with positive tuberculin 10 mm and more were included. Punch biopsy taken from the site of positive TST after (2) days of doing the test in (10) patients, and around (10) days in (8) patients and in (2) patients 6 weeks after positive reaction and these biopsies were processed for H&Estain. Results: The total biopsies from positive TST were 20, 10 of them taken from patients diagnosed with active TB, anti TB therapy was started for them. The other 10 biopsies taken from patients diagnosed latent TB. Regarding the patients with active TB, their histopathological results revealed: 10(100%) biopsies had superficial and deep perivascular and periadnexial lymphocytic and lymphohistiocytic infiltrate, vascular dilatation, dermal edema, 9(90%) had basal liquefactive degeneration, 2(20%) biopsies revealed dermatitis like picture while panniculitis was seen in 4(40%) biopsies. Granuloma was detected in 7(70%) patients. While in latent TB patients including 10 patients, the biopsies of positive tuberculin test site had shown the following: 10(100%) biopsies had superficial and deep perivascular and periadnexial lymphocytic and lymphohistiocytic infiltrate, vascular dilatation, dermal edema, 9(90%) basal liquefactive degeneration, 2(20%) biopsies dermatitis like picture while panniculitis in 3(30%) biopsies and granuloma in 4(40%) patients. Conclusion: The degree of inflammatory reaction at the positive TST might predict the future risk of developing TB in a patient with a latent TB. While the presence of granuloma is more suggestive of the present active TB or having a higher risk of developing active TB in the near future.
Keywords: Active tuberculosis, Latent tuberculosis tuberculin skin test, Granuloma
Cite this paper: Khalifa E. Sharquie, Adil A. Noaimi, Fatima A. Khalaf, Granulomatous Reaction at the Site of Positive Tuberculin Skin Test is a Marker of Active TB (Clinical and Histopathological Study), American Journal of Dermatology and Venereology, Vol. 8 No. 4, 2019, pp. 55-60. doi: 10.5923/j.ajdv.20190804.01.
1. Introduction
- Tuberculosis (TB) still endemic in many countries, including Iraq. Confirmatory diagnostic tests might be needed in some cases with suspected clinical diagnosis. Pathophysiology of tuberculosis is either: active infection which occurs when containment by the immune system (T-cells/macrophages) is inadequate. It can arise from primary infection, or re-activation of previously latent disease. Transmission of TB is via inhalation of aerosol droplets containing bacterium [1] or latent TB which occurs when a person has the TB bacteria within their body, but the bacteria are present in very small numbers. They are kept under control by the body’s immune system and do not cause any symptoms [2].A person with latent TB does not feel sick and is not infectious. They cannot pass the TB bacteria on to other people. In addition they will usually have a normal chest X-ray and a negative sputum test. It is often only known that someone has latent TB because they have had a TB test, such as the TB skin test [3]. The two types of clinical manifestation of tuberculosis (TB) are pulmonary TB (PTB) and extrapulmonary TB (EPTB). The former is most common. EPTB refers to TB involving organs other than the lungs (e.g.: pleura, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, or meninges) [4].Tuberculosis of skin takes many variants like: tuberculous chancre, lupus vulgaris, warty TB, scrofuloderma, miliary tuberculosis, cold abscess, etc... [5]. Several circumstances may suggest the diagnosis of cutaneous tuberculosis including: clinical history, physical signs, positive TST, the presence of acid-fast bacilli in histopathology of the lesion, the presence of active tuberculosis elsewhere in the body and the effect of specific therapy as a therapeutic trial [6].The histopathological evaluation of cutaneous lesion might be enough to establish clinical diagnosis of the disease. But in many cases the histopathological examination can give a nonspecific picture and hence is not helpful for diagnosis [1,2].In these cases tuberculin testing could be carried out which have sensitivity and specificity to (94.7%), (80%) respectively [7]. During clinical practice we came across a patient with warty lesions on his buttock where the histopathology showed a picture of viral wart but on the clinical ground there was a high suspicion of tuberculosis. In this patient tuberculin test was carried out and it was positive (20 mm). When a biopsy was done for this test, it showed a granuloma, hence patient was treated with anti-TB therapy and the patient responded within weeks and complete resolution occurred within few months. This observation had encouraged us to arrange the present study by taking a biopsy from all patients with positive tuberculin testing and to be evaluated histopathologically looking for inflammatory reaction including granuloma formation and to be compared with clinical findings.Tuberculin skin test is designed to detect a memory cell–mediated immune response to M. tuberculosis. The test becomes positive 2–10 weeks after infection and remains positive for many years, although it may wane with age [8]. BCG vaccine as an antigen has proved its effectiveness as an immunotherapy for viral warts, possibly through its immunological action. It might cause disfiguring scar at injection site [9] and has a potential to cause serious adverse reactions especially in immune-compromised patients. Sharquie et al found that BCG alone showed complete recovery in 39%, while patients received distilled water showed a recovery rate 13.7% and no recurrence had been reported during the follow up period [9]. In split study where intralesional tuberculin was injected in one side and intralesional distilled water at the other side of the forearm, 23.3% showed complete cure while those patients treated with distilled water showed no cure. These results do suggest that BCG had systemic immunological effect while intralesional tuberculin had mainly localized immunological action [10]. Hence the objective of present work is to do tuberculin testing for patients with latent and active TB and study the histopathological findings of positive tuberculin in order to get objective findings that are helpful for diagnosis of TB.
2. Patients and Methods
- Twenty patients attending Center of Dermatology and Venereology, Baghdad Teaching Hospital from January 2017 to January 2018, were enrolled in the current study. These were 12 males and 8 females, and their ages ranged between (19-62) years, with median and mean age were 41, 42 years respectively. These patients were sent for TST for different purposes, 11 of them did TST as baseline investigation before starting biological or immunosuppressive treatment while 7 of them sent for TST to exclude or confirm clinically suspected pulmonary TB and 2 were suspected cutaneous TB.Inclusion criteria: all patients included had positive tuberculin test more than 10 mm in diameter, older than 15 years, included in this study.Full history was taken (Table-1), including name, age, sex, occupation, productive cough, weight loss, night sweating, personal or family history of pulmonary or extrapulmonary TB, BCG vaccination, the current cause of doing TST, and the measurement of TST as had carried out by health officer in Center of Pulmonary Disease, medical, surgical and drug history was obtained.
|
|
3. Results
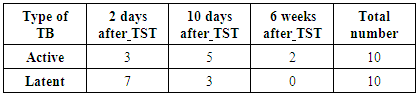
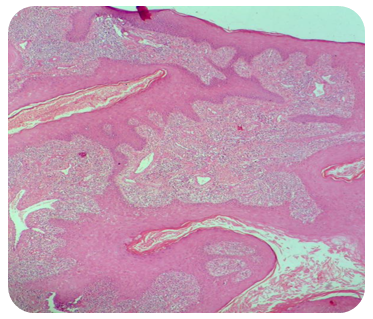
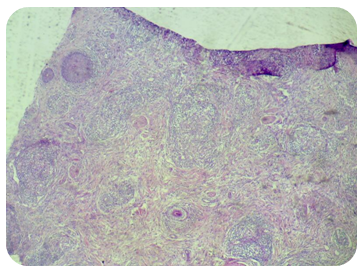
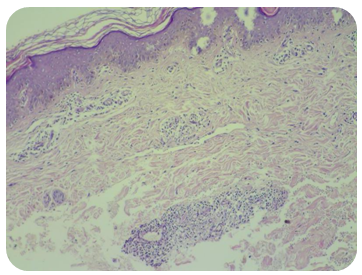
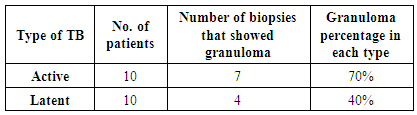
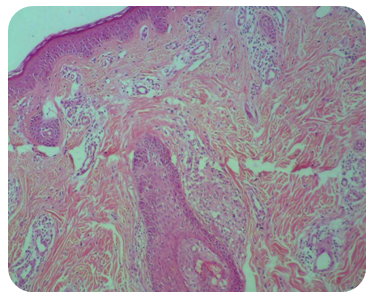
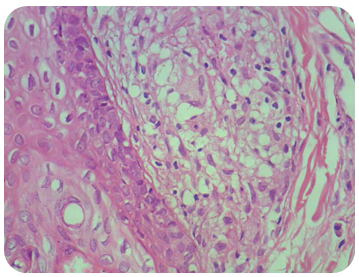
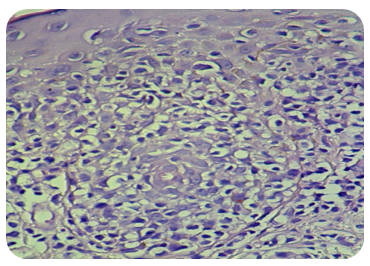
- The total biopsies from positive TST were done on 20 patients. Ten of them taken from patients diagnosed active while the other 10 biopsies taken from patients diagnosed latent TB.Regarding the patients with active TB, the biopsies were taken at different interval after doing the TST: after 2 days in 3 patients which had symptoms suggestive of pulmonary TB (productive cough, weight loss, fever, hemoptysis), anti-TB started for them while in 5 patients after 10 days in, 2 of them sent for TST by medical specialist because of their symptoms that suggest pulmonary TB, anti-TB started for them. The other 3 patients sent for TST as baseline investigation mandatory before starting biological treatment (Etanrecept), and their biological treatment postponed for 2 months through which prophylactic anti-TB was taken.While after 6 weeks in 2 patients, the first one had active cutaneous TB (LV), anti-TB started for him. The second one had large polypoid, warty lesions in perianal area for many years, as shown in (Figure-1A) with previous diagnosis of giant genital wart, he had multiple histopathological reports of lesional biopsies, assigned as genital wart without any granuloma (Figure-1B). In spite of that, clinical suspicion was toward cutaneous TB (warty TB), TST done and was positive (20) mm, biopsy from TST site taken after 6 weeks which revealed obvious granuloma (Figure-2A, B). Anti TB started for him, perianal lesion disappeared after 6 months of treatment as shown in (Figure-2C). This case was an initiator of this current work.The histopathological results of positive TST from active TB patients revealed: 10(100%) biopsies had superficial and deep perivascular and periadnexial lymphocytic and lymphohistiocytic infiltrate, vascular dilatation, dermal edema, 9(90%) had basal liquefactive degeneration (Figure-3). In 2(20%) biopsies revealed dermatitis like picture, with spongiosis, exocytosis and pautrier microabcess. Panniculitis was seen in 4(40%) biopsies (Figure-4). Granuloma seen in 7(70%) patients as shown in table-3, one of them was xanthomatous granuloma (Figure-5-A, B).While in latent TB patients (10 patients), the biopsies were taken at different interval after doing the TST: after 2 days in 7 patients sent for TST as baseline investigation before (Etanrecept), their biological treatment postponed for 2 months through which prophylactic anti-TB was taken. After 10 days in 3 patients, the 1st one did TST as baseline investigation; the other 2 were suspected pulmonary TB. Their histopathological results revealed: 10(100%) biopsies had superficial and deep perivascular and periadnexial lymphocytic and lymphohistiocytic infiltrate, vascular dilatation, dermal edema, 9(90%) had basal liquefactive degeneration (Figure-6). In 2(20%) biopsies revealed dermatitis like picture. Panniculitis was seen in 3(30%) biopsies while granuloma was detected in 4(40%) biopsies of these patients. (Table-3).
 | Figure 1A. A 37 years old male with 5 years history of large warty lesions on the left gluteal region and the primary diagnosis was genital warts |
 | Figure 2A. The same patient in (fiure1-A) showing granuloma at positive tuberculin site (100x) |
 | Figure 2B. The same patient showing well recognized giant cell formation at granuloma site (400x) |
 | Figure 2C. Clearance of the same patient in figure (1-A) after 6 months of starting anti-TB |
 | Figure 3. Thirty years old patient with positive tuberculin skin test after 2days, showing sever inflammatory reaction with lymphocytic invasion in addition to spongiosis (400x) |
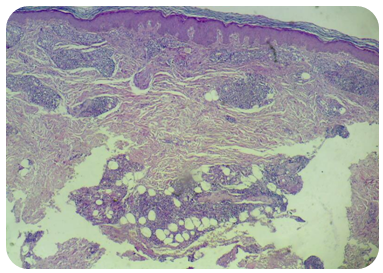 | Figure 4. A 38 male patient with positive tuberculin skin test after 10 days showing acanthosis, superficial and deep perivascular infiltrate in addition to panniculitis (100x) |
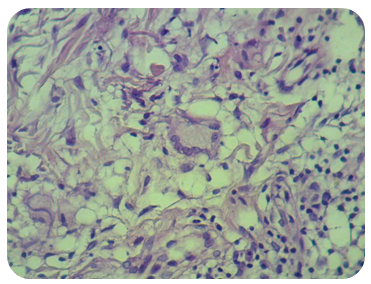 | Figure 5B. The same patient showing well recognized giant cells at the site of tuberculin test (400x) |
|
4. Discussion
- Diagnosis of skin TB after full clinical evaluation might need many investigative tools like histopathological evaluation, TST, IGRA, PCR, tissue culture and AFB stain [6]. The sensitivity and specificity of Mantoux test reach (94.7%), (80%) respectively [7]. Meanwhile IGRA sensitivity and specificity for the diagnosis of EPTB was 72% and 82%, respectively, for QuantiFERON-TB Gold. 90% and 68%, respectively, for T-SPOT.TB [11]. Histopathology of positive tuberculin was not well studied and evaluated in medical literature and there are two studies that showed:In the first study that was published in 1939 and was conducted in USA [12], where the histopathological evaluation was done after 2 weeks of positive TST and showed histiocytic cells infiltrate of dermis, some of these were suggestive of epitheliod cells while others resemble fibroblasts but no granuloma reaction detected.While the second study that carried out in Turkey 2008 [13] and showed inflammatory reaction at the site of positive TST and were classified into three types: Perivascular (PV)-type, basal spongiotic dermatitis (BSD)-type and erythema multiforme (EM)-type but no granuloma was seen.In the present study and during clinical practice, we noticed that some patients although had skin tuberculosis but the histopathology of biopsy showed non-specific changes, while the biopsy of positive tuberculin test showed granuloma formation.This observation had encouraged us to conduct the present work as all positive tuberculin test in patients with clinical diagnosis of TB was biopsied and histopathological evaluation was carried out.In all tuberculin positive patients, including active and latent TB, severe inflammatory reaction, mainly superficial and deep perivascular infiltrate were observed and in some patients even panniculitis was noticed.This reaction usually seen after 2 days of positive TST and became more florid after 10 days and even more after 6 weeks.Granuloma was noticed at the site of tuberculin reaction in 70% of cases of active TB (Table-3), while these granuloma were noticed in 40% of patients with so called latent TB. Accordingly patients with active TB (70%) had higher result when compared with latent TB (40%). The presence of severe inflammatory reaction at site of positive TST does suggest that patient had some localized activity of TB especially in so called latent TB, while the presence of granuloma strongly suggest that the patients had active TB whether skin or systemic.So the presence of this tuberculin positive granuloma is a very helpful for diagnosis of active tuberculosis when compared with other laboratory tests especially in suspected cases.
5. Conclusions
- We conclude that the degree of inflammatory reaction at the positive TST might predict the future risk of developing TB in a patient who had apparently no obvious TB. But the presence of granuloma at positive tuberculin test is more suggestive of the present active TB or has high risk of developing TB in the near future.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML