-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(3): 37-40
doi:10.5923/j.ajdv.20190803.01

Post-Scabietic Mastocytoid Nodules: A Clinical and Histopathological Evaluation with New Pearls
Khalifa E. Sharquie1, Mohammed M. Shanshal2
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology and Venereology, Center of Dermatology and Venereology, Medical City, Baghdad, Iraq
2Center of Dermatology and Venereology, Medical City, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology and Venereology, Center of Dermatology and Venereology, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Post-scabietic nodules are a result of a persistent immunological reaction that might continue for months after the effective treatment of scabies. Objective: To evaluate the clinical and histopathological features of post-scabietic nodules in order to reach a new insight into its etiopathogenesis. Patients and methods: This study was done in the center of Dermatology and Venereology -Baghdad Teaching Hospital, during the period from April 2017- November 2018. Thirty-four patients with post scabietic nodules were enrolled and full clinical evaluation of the rash was carried out. Excisional biopsies were taken from 22 patients, these biopsies were processed and stained with Hematoxylin- Eosin and Giemsa stain. Results: Clinical evaluation showed that post scabietic nodules had features like the peau d'orange appearance and Darier sign simulating the rash of mastocytosis. During histopathological evaluation three patterns of the inflammatory infiltrate in post scabietic nodules were observed, eosinophils predominant, mast cells predominant and a mixed cellular variant of eosinophil and mast cells. Conclusion: post-scabietic nodules had many characteristic clinical and new histopatholical features that might resemble mastocytosis, hence the term post-scabietic mastocytoid nodules was used.
Keywords: Post-scabietic nodules, Post-scabietic mastocytoid nodules, Histopathology, Mastocytosis and scabies
Cite this paper: Khalifa E. Sharquie, Mohammed M. Shanshal, Post-Scabietic Mastocytoid Nodules: A Clinical and Histopathological Evaluation with New Pearls, American Journal of Dermatology and Venereology, Vol. 8 No. 3, 2019, pp. 37-40. doi: 10.5923/j.ajdv.20190803.01.
1. Introduction
- Scabies is a common parasitic infection caused by the mite Sarcoptes scabiei variety hominis, an arthropod of the order Acarina. Scabies was added to the World Health Organization (WHO) list of neglected tropical diseases in 2013 and is estimated to affect more than 130 million people globally at any time. [1] The infection is endemic in many impoverished communities, but prevalence rates vary widely; seasonal outbreaks and documented peaks during times of war are probably related to crowding and population movements. [2]After treatment of scabies, many patients gets complete clearance of symptoms and signs, but 7-10% of the patients might have continuous itching and rash which are related to a persistent immunological reaction, one of these is the post scabietic nodules. Post scabietic nodules presented as erythematous to violaceous pruritic, smooth, non-excoriated, nodules ranging from 2-20 millimeters in diameter. These nodules occur in certain predilection sites, particularly on the axilla, groins, scrotum and penis. [3] The histopathology of post scabietic nodules is always dynamic, while Sharquie et al 1997, showed that the predominant cells in the inflammatory infiltrate of the post scabietic nodules were the eosinophils and hence the name eosinophilioma was used. [4] In a subsequent study, Sharquie et al, 2013; have reassessed the histopathology of the post scabietic nodules and showed that the dermal infiltrate of post scabietic nodules was mainly diffuse dense lymphocytic reaching the degree of similarity to lymphoma, regarding the eosinophils surprisingly, they were absent in all the tissue sections while mast cell infiltrate was not evaluated. [5] So unfortunately, no study was carried out to detect the presence of the mast cells in the infiltrate of post scabietic nodules. Accordingly, the objective of the present work is to do a full clinical and histopathological evaluation of the post -scabietic nodules including mast cells infiltrate.
2. Patients and Methods
- This observational clinical and histopathological study was done in the center of Dermatology and Venereology -Baghdad Teaching Hospital, Medical City; Baghdad; Iraq during the period from April 2017- November 2018.All patients with post scabietic nodules were enrolled in this study, based on the medical history of scabies and clinical examination. Patients had been treated by different scabicides. Four patients had post scabietic nodules in the presence of active scabies, while thirty patients had no active scabies at the time of attendance to the hospital and were considered post-scabietic. Relevant data was recorded for patients regarding: name, age, sex, occupation, residence, and previous personal and family history of scabies. All the patients were examined for the numbers, sites and the sizes of the post scabietic nodules. Examination for Darier sign was done for all patients by gentle rubbing or stroking of one or more of the lesions. Formal consent was taken from all enrolled patients after the nature of the current study was fully explained. Ethical approval was performed by the Scientific Council of Dermatology and Venereology-Arab Board for Medical Specializations. Local anesthesia using lidocaine was injected to the site of biopsy then excisional biopsies were taken from the post scabietic nodules. Excisional biopsies were taken from 22 patients (64.70%) while the other 12 patients (35.29%) refused the biopsy. These biopsies were processed for histopathological examination and stained with Hematoxylin-Eosin stain. Giemsa stain was carried out mainly to demonstrate the presence of mast cells in the dermis of affected patients. The Photographs were taken using the iPhone 6 smartphone (8.0 megapixels).
3. Results
- Thirty-four patients with post- scabietic nodules were enrolled in this study, 30 (88.23%) males and 4 (11.76%) females with a male to female ratio 7.5: 1, the age range of males at presentation was from 2-67 years with a mean ± SD 28.56 ±15.31 years; while the age range of females at presentation was from 19-54 years with a mean ± SD 35.75 ±16.47 years. The nodules started to appear simultaneously with the onset of scabies but did not resolve after eradication of the infestation with different scabicide modalities. The nodules persisted for a duration ranged from 1 week to 8 weeks with a mean± SD 3.56 ± 2.16 weeks.Clinical findings during the examination: The nodules in most of the patients were darkly pigmented dusky red in color and not excoriated, some of them had the peau d'orange appearance simulating the rash of nodular mastocytosis. The number of lesions ranged from 1-20 lesions with a mean ± SD 5.79 ± 4.53 lesions. Their sizes ranged between 0.5cm – 2cm (mostly < 1cm) (85%). These nodules were more heavily involving scrotum in 19 patients (55.88%) and penile shaft in 17 patients (50%) and less commonly involving the upper thigh, axilla, lower abdomen, buttock and breast. Examination for Darier sign was done for all patients by gentle rubbing or stroking of one or more of the lesions. It was positive in only three patients (8.82%) where gentle rubbing or stroking of the lesions, was followed by local itching, erythema and wheal formation within 2-5 min. This might persist from 30min to several hours (Figure 1).
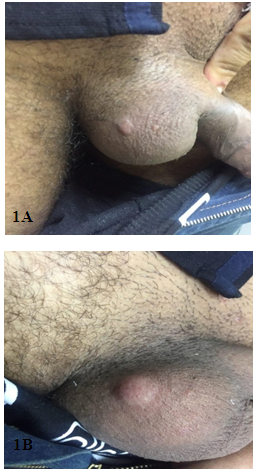 | Figure 1. Post-scabietic nodules showing twenty-four years old male patient with post scabietic nodules before (1A) and after (1B) rubbing of the lesion, demonstrating positive Darier sign |
 | Figure 2. Showing two patients with post scabietic nodules demonstrating typical grouping (2A) and sporotrichoid-like pattern (2B) |
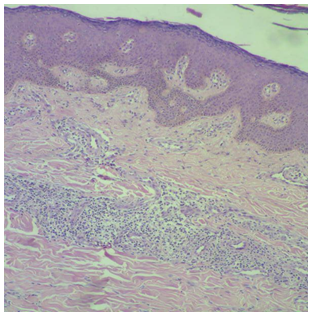 | Figure 3. Histopathology of post scabietic nodules showing pseudoepithelial hyperplasia with superficial, deep and perivascular inflammatory infiltrate. Heamatoxylline - Eosin stain X40 |
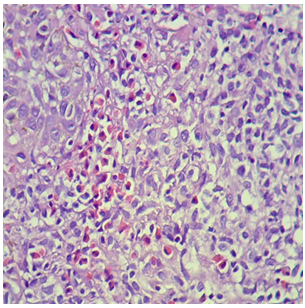 | Figure 4. Histopathology of post scabietic nodules showing predominant eosinophils. Heamatoxylline - Eosin stain X400 |
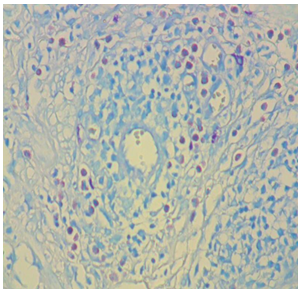 | Figure 5. Histopathology of post scabietic nodules showing predominant mast cells. Giemsa stain X400 |
4. Discussion
- Although scabies is an endemic disease in Iraq but from now and then it runs an epidemic state, especially in a war situation. So scabies is a common disease among the population and it’s the commonest cause of itching in Iraq. Its therapy is relatively successful by different scabicides modalities, but sulfur ointment is still the main standard of therapy for the cure of scabies. [6] Even patients when they get cure from scabies, they might continue to have itching for weeks or longer. Although the specific features of scabies like burrows will disappear, many of the patients had persisting itching with post scabietic nodulation that was mainly located in the scrotum, penile shaft, and axilla that might stay for a long time as seen in the present study. The etiopathogenesis of the post scabietic nodules is not well explained in the medical literature, but we can hypothesize that there might be persisting antigen either in the skin, blood or both that might stimulate cell-mediated reaction, thus forming these post scabietic nodules and this rash will disappear only when these antigens are cleared up from the body. From extensive clinical observation in patients with post scabietic nodules, we have noticed many features that resemble nodular mastocytosis including the nodular appearance with absent excoriation, the dusky red color, the peau de orange appearance, the positive Darier sign and the chronicity of both conditions. [7, 8]Accordingly, the objective of this study was to do a full clinical and histopathological evaluation of post scabietic nodules and to be compared with the rash of mastocytosis.Clinical features:In the current study, Post scabietic nodules were non excoriated, pigmented dusky red in color and had a tendency to occur in specific predilection areas like a scrotum in 55.88%, penile shaft in 50%, in addition to the thigh, axilla, lower abdomen, and buttock. In some patients, there were typical grouping and in two patients there was a sporotrichoid pattern. Darier sign similar to that observed in mastocytosis was positive in three patients (8.82%). This Darier sign was already described with post scabietic nodules in two case reports only. [7, 8] Histopathological evaluation: The histopathology of post scabietic nodules is a dynamic feature as the previous studies showed that the predominant cells in the inflammatory infiltrate are eosinophils and lymphocytes and hence the terms pseudolymphoma and eosinophilioma were used respectively in the past, but no specific stain was carried out for detection of the mast cells. [4, 5]The present study evaluated the histopathology of post scabietic nodules using H&E and Giemsa stains and showed: (1) hyperkeratosis (18.18%), acanthosis (90.9%), spongiosis (36.36%) and pseudoepithelial hyperplasia (18.18%). Eosinophils were seen infiltrating the dermis in (9.09%) of the cases. (2) The dermis with dilated blood vessels (72.72%) and diffuse inflammatory infiltrate involving the papillary and reticular dermis, in addition to perivascular infiltrate (90.9%) (3) The inflammatory infiltrate consisted of lymphocytes (90.9%), eosinophils (72.72%). The density of eosinophils was classified into severe in 50%, moderate in 25% and scanty in 25%) and plasma cells in (4.54%).Giemsa stain showed that only mast cells were found in (27.27%) while mixed infiltrate of mast cells and eosinophils was found in (36.36%).From H&E stain and Giemsa stains, we concluded that there were three patterns of the inflammatory infiltrate in post scabietic nodules: eosinophils predominant variant 36.36%, mast cells predominant variant in 27.27% and a mixed cellular variant of eosinophils and mast cells in 36.36%. These histopathological patterns were not reported before in the medical literature.
5. Conclusions
- This study showed a classical picture of the post- scabietic nodules as all the patients demonstrated non excoriated, pigmented dusky red in color nodules with a tendency to occur in specific predilection areas and in some patients, there were typical grouping. Darier sign similar to that observed in mastocytosis was positive in 8.82%. Also, the histopathological picture of post scabietic nodules showed three patterns of the inflammatory infiltrate in post scabietic nodules were observed: eosinophils predominant variant in 36.36%, mast cells predominant variant in 27.27% and a mixed cellular variant of eosinophils and mast cells in 36.36%. Accordingly, there are many clinical and histopatholigal features that resemble nodular mastocytosis, hence the term post scabietic mastocytoid nodules was introduced.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML