-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(2): 33-35
doi:10.5923/j.ajdv.20190802.04

Symmetrical Giant Facial Plaque-Type Juvenile Xanthogranuloma; A New Case Report
Khalifa E. Sharquie1, Fatema A. Al-Jaralla2, Adil R. Al-Saadawi3
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
2Department of Dermatology, College of Medicine, Baghdad University, Baghdad, Iraq
3Department of Pathology, Baghdad Medical City Complex, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Juvenile xanthogranuloma is the most common non-Langerhans histiocytosis (non-LCH). The vast majority of lesions are diagnosed within the first year of life and about 80% of cases are solitary. Symmetrical giant facial plaque-type juvenile xanthogranuloma (SGFP-JXG) is a rare and new variant of juvenile xanthogranuloma (JXG), reported only in three cases in the medical literature and it was originally reported by Gunson & Birchall in 2008. Herein we report a new case of SGFP-JXG as a thirty months old girl, presented with seven months history of a diffuse asymptomatic yellowish to orange butterfly plague eruption on the face, and papular eruption on the trunk and upper limbs. A skin biopsy with immunohistochemistry showed a Non-langerhan histiocytosis type juvenile xanthogranuloma. We emphasise the importance of knowing this rare variant with atypical presentation that makes the diagnosis of JXG extremely challenging.
Keywords: Juvenile xanthogranuloma, Symmetrical giant facial JXG, JXG
Cite this paper: Khalifa E. Sharquie, Fatema A. Al-Jaralla, Adil R. Al-Saadawi, Symmetrical Giant Facial Plaque-Type Juvenile Xanthogranuloma; A New Case Report, American Journal of Dermatology and Venereology, Vol. 8 No. 2, 2019, pp. 33-35. doi: 10.5923/j.ajdv.20190802.04.
1. Introduction
- JXG is a non-Langerhans histiocytosis occurring predominantly in infancy and early childhood. It usually manifests as asymptomatic, red-brown papule which slowly enlarges to a diameter of 1 to 2 cm. Evolution into a yellow-brown papule, plaque, or nodule often occurs, followed by spontaneous resolution that may leave an atrophic scar. [1]The symmetrical giant facial plaque variant of JXG (SGFP-JXG) is very rare. It was originally reported by Gunson & Birchall in 2008 [2]. To the best of our knowledge, the present case is the fourth case with SGFP-JXG. Gunson & Birchall described SGFP-JXG lesions as multiple large, flat, symmetrically distributed plaques of over 2 cm in diameter. [2] The case in the literature had facial lesions, without any JXG lesions on other body sites. Herein we report a thirty months old girl with SGFP-JXG on the face, trunk and upper limbs.
2. The Present Case
- A 30 months old girl, presented with seven months history of a diffuse symmetrical butterfly asymptomatic yellowish to orange plaque eruption, on the face, and pa1pular rash on the trunk and limbs. The rash was first noticed in the form of red macules at approximately 23 months of age, which slowly evolved over the following seven months. She is otherwise well. There was no family history of neurofibromatosis. Physical examination revealed symmetrical butterfly, yellow-orange colour, indurated facial plaques (Fig 1a and 1b) as there was bilateral involvement of the upper and lower eyelids, cheeks, and chin, sparing the forehead, upper and lower lips. Areas of the body involved include abdomen, back and upper extremities. (Fig 1c and 1d). There was no oral mucosal involvement and no cutaneous manifestations of type I neurofibromatosis. There was no palpable hepatosplenomegaly or lymphadenopathy. An ophthalmological examination was normal. A biopsy of lesional skin showed a mixed dermal inflammatory cell infiltrate rich with foamy histiocytes extending into the deep dermis (Fig 2 a, 2 b) while Touton giant was not found. CD68 staining was positive once but when repeated on the same biopsy block in different lab, it was negative while lyzozymes staining was positive (Fig 2c). Hence the clinical and histologic diagnosis was that of xanthogranuloma.Blood investigations, including full blood count, liver function tests, albumin, cholesterol studies, fasting glucose, and renal function, were all within normal limits.So the final diagnosis of a symmetrical giant facial plaque-type variant of juvenile xanthogranuloma (JXG) was established.
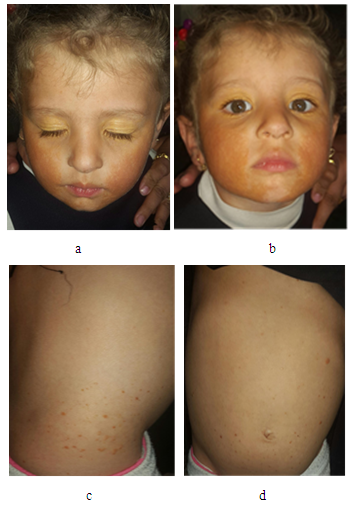 | Figure 1. a and b- Showing involvement of the face with diffuse yellowish to orange plague eruption, while figure c-and d showing papular involvement of the trunk |
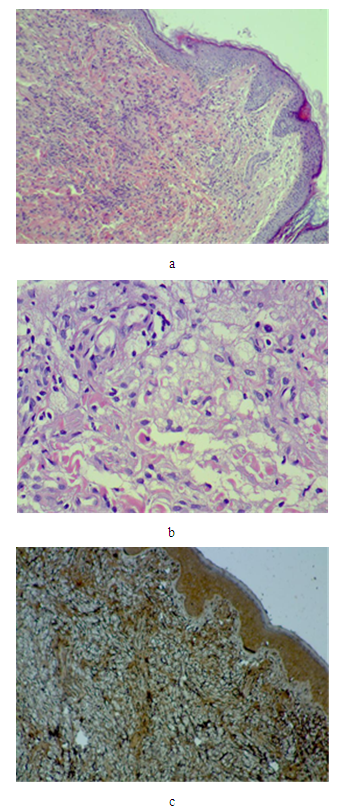 | Figure 2. (a) microscopic view showing foamy histeocytes H&E stain × 40 while (b) H&E stain ×400 while (c) ×40 showing positive immunohistochemistry with lysozymes |
3. Discussion
- SGFP-JXG was first reported by Gunson & Birchall. [2] in 2008. After extensive review of medical literature and to the best of our knowledge, the present case is the fourth SGFP-JXG. to be reported. Gunson & Birchall described SGFP-JXG as multiple large, flat, symmetrically distributed facial plaques of over 2 cm in diameter [2] but without any JXG lesions on other body sites. The lesions had been present for > 6 years and had shown no sign of spontaneous resolution. [2]The second case was described in 2013 and also had the facial lesions for 10 years without any noticeable tendency of spontaneous resolution. Interestingly, he had also had JXG rash on the arms that tended to spontaneously resolve. [3] The third reported case was a 3-year-old Korean boy with bilateral yellowish indurated plaques on both cheeks since 1 year after birth. The lesions showed no signs of regression and thus were treated with a single session of fractional ablative CO2 laser, which resulted in a significant reduction of the lesion. [4]The rash in this new variant of xanthogranuloma had no tendency for spontaneous resolution in contrast to ordinary xanthogranuloma where natural spontaneous regression is a part of the course the disease [5, 6, 7, and 8]. CD68 staining was positive once and when repeated on the same biopsy block was negative section, while lyzozymes staining was positive, showing the inconclusive and inconsistent nature of immunohistochemistry staining techniques. Accordingly the clinical picture and histopathology, in addition to clinical vigilance are more important to relay on in diagnosing challenging cases of xanthogranuloma. Unfortunately, the therapeutic options are limited given the large and cosmetically sensitive areas involved but still resolution might occur.
4. Conclusions
- SGFP-JXG is a very rare variant of xanthogranuloma presenting with typical clinical picture. The present patient is considered the fourth case to be reported. The histopathology showed foamy histiocytes while CD68 had inconsistent results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML