Shereen Y. Alamin1, Abdelhameed Hifny2, Hytham A. Agla3, Ahmed N. Aljarbou4, Khalid O. Alfarouk5, 6, Intisar A. Bashir7, Yousif Tibin8, Adil H. H. Bashir1
1University of Khartoum, Khartoum, Sudan
2Al-Azhar University, Cairo, Egypt
3King Fahd Hospital, Al-Madinah Al-Munwarah, KSA
4College of Pharmacy, Qassim University, Qassim, Saudi Arabia
5Alfarouk Biomedical Research LLC, Temple Terrace, Florida, USA
6Al-Ghad International College for Applied Medical Sciences, Al-Madinah Al-Munwarah, KSA
7Zamzam University College, Khartoum, Sudan
8Faculty of Medicine, University of Bahri, Khartoum, Sudan
Correspondence to: Adil H. H. Bashir, University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Atopic dermatitis is a chronic, relapsing, pruritic inflammation of epidermis and dermis, often associated with a personal or family history of asthma, conjunctivitis, allergic rhinitis or atopic dermatitis. Objective: It was purposing to measure the prevalence of Atopic Dermatitis, to determine the demographic variations, the provocation factors, clinical presentation and the associated atopic diseases. Patients and Methods: This study is an observational, descriptive, prospective, cross-sectional, hospital-based. It was carried out during the period from September 2014 to January 2015. The study was conducted at Khartoum Dermatology and Venereology Teaching Hospital. The pre-designed questionnaire collected the data, and the diagnosis was followed Hanifin and Rajka criteria. Results: The prevalence of atopic dermatitis among Sudanese patients attending Khartoum hospital in the period from September 2014 - January 2015 was found to be (1.15%). The total number of patients with atopic dermatitis in this study was 60 patients, 33 of them represents (55%) were females, the most affected ages were infants (0-18 months) represented (41.7%). The majority of the patients represented (53.3%) were suffering from atopic dermatitis for months. Most of the patients represented (70%) had no other atopic. Atopic dermatitis was found in (15%) of patients’ siblings, (10%) of their mothers. Moreover, family history of atopic diseases was found among (55%) of the patient’s families. Localized atopic dermatitis was found in (65%) of the patients. Most of the patients were found in the acute stage (41.7%). Provocating factors were detected in all patients in form of contact irritants (33.3%), weather (25%), infection (11.7%), drug (10%), contact and weather (8.3%), dust (6.7%), food and weather (3.3%) and stress (1.7%). Most of the patients (28.3%) presented with macules, papules, pustules and crust and least (16.7%) with papules, vesicles, and crust with flexural distribution in most of them (26.7%).
Keywords:
Atopic Dermatitis, Dermatitis, Sudan
Cite this paper: Shereen Y. Alamin, Abdelhameed Hifny, Hytham A. Agla, Ahmed N. Aljarbou, Khalid O. Alfarouk, Intisar A. Bashir, Yousif Tibin, Adil H. H. Bashir, Atopic Dermatitis: Epidemiology and Clinical Pattern in Khartoum Dermatology and Venereology Teaching Hospital, American Journal of Dermatology and Venereology, Vol. 8 No. 2, 2019, pp. 19-27. doi: 10.5923/j.ajdv.20190802.02.
1. Introduction
The word ‘atopy’ was introduced by Coca in 1923 as a convenient collective term for a group of diseases, chief among which are asthma and hay fever, which occurs spontaneously in individuals who have a family history of susceptibility to this condition [1]. Atopic dermatitis is a difficult condition to define because it lacks a diagnostic test and shows variable clinical features. The following definition seems to be in accord with most consensus groups. Atopic dermatitis (which is synonymous with atopic eczema) is an itchy, chronic or chronically relapsing, inflammatory skin condition. The rash is characterized by itchy papules (occasional vesicles in infants), which typically in flexures lichenified and excoriated. Become excoriated and lichenified, and typically have a flexural distribution. Associated other conditions with atopic dermatitis are frequently seen in the individual himself, or The eruption is frequently associated with other atopic conditions in the individual or other family members [2, 3]. Atopic dermatitis is frequently defined by many authors as inflammatory chronic pruritic relapsing condition Atopic dermatitis is a chronic, relapsing, pruritic inflammation of the epidermis and dermis, often associated with a personal or family history of asthma, conjunctivitis, allergic rhinitis or atopic dermatitis.Multifactorial, environmental and genetic factors play a role in the pathogenesis of Atopic dermatitis, arises because of a complex interaction of genetic and environmental factors. These include defects in skin barrier function making the skin more susceptible to irritation by contact irritants, the weather, temperature and non-specific triggers [4]. The prevalence rate of atopic dermatitis is rising, and atopic dermatitis affects 15-30% of children and 2-10% of an adult. The figure shows the developed countries prevalence. Where atopic dermatitis rate seems is raising that is probably exposure to allergens and other factors like air pollution or infections with Staphylococcus aureus as well as decrease breastfeeding. Good hygiene awareness will increase children tolerance to irritants developed from microbes. This figure estimates the prevalence in developed countries [5]. The prevalence rate of atopic dermatitis seems to be rising probably due to higher exposure to indoor allergens, air pollution, and other factors like infection with Staphylococcus aureus, decrease breastfeeding, more awareness of the disease and hygiene hypothesis which state that increases tolerance of irritants develops when children are increasingly exposed to microbes [5]. Atopic dermatitis appearance variations between individuals are present. Skin in between attacks looks normal, and from time to time skin flares and becomes weepy blistered patches. There is variation in the appearance of atopic eczema between individuals. From time to time, most people have acute flares with inflamed, sometimes blistered and weepy patches. In between flares, the skin may appear normal or suffer from chronic eczema with dry, thickened and itchy areas. [4] The presence of infection or an additional skin condition, the creams applied, the age of the person, their ethnic origin, and other factors can alter the way eczema looks and feels [5]. Xerosis, lichenification, and eczematous lesions are primary findings of atopic dermatitis, as well excoriations and crusting. Age of the patients affects eczema morphology are seen in different locations. Include xerosis, lichenification, and eczematous lesions. Excoriations and crusting are common. The eczematous changes and its morphology are seen in different locations depending on the age of the patient [6]. In Infancy, Atopic dermatitis is usually noticed soon after birth, Xerosis occurs early and often involves the whole body, and the earliest lesions affect the creases, with erythema and exudation. Over the following few weeks, lesions are usually localized to the cheeks, the forehead and scalp, and the extensors of the lower legs [7, 8]. In childhood xerosis often generalized, the skin is flaky and rough, lichenification is characteristic of childhood atopic dermatitis. Face pallor is common and lesions around eyes like erythema and scales seen. Pallor of the face is common, erythema and scaling occur around the eyes, Flexural creases, particularly the antecubital and popliteal fossae [7, 8]. In adulthood, lesions become more diffuse with an underlying background of erythema. The face is commonly involved and is dry and scaly, xerosis is prominent, and lichenification may be present [7, 8].
2. Results
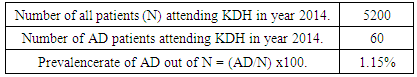
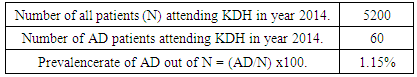
The prevalence of atopic dermatitis among Sudanese patients attending Khartoum Dermatology and Venereology Teaching Hospital Was found to be (1.15%) (Table 1).Table (1). Showed prevalence rate of AD among patients attending Khartoum dermatology hospital in the year 2014
 |
| |
|
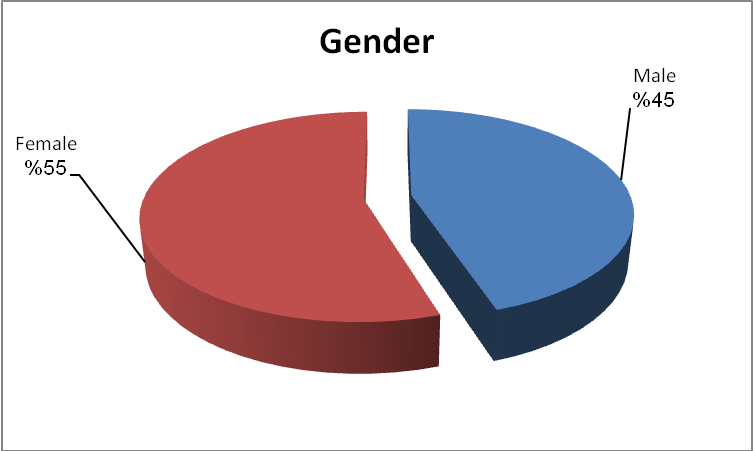
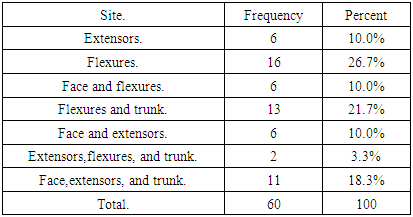
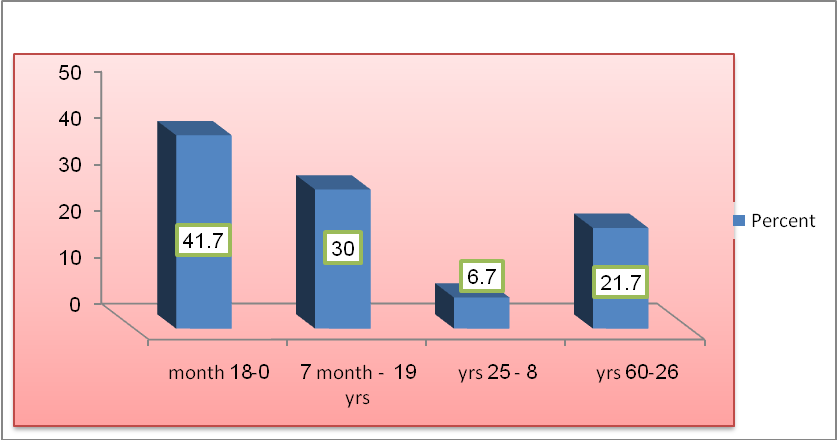
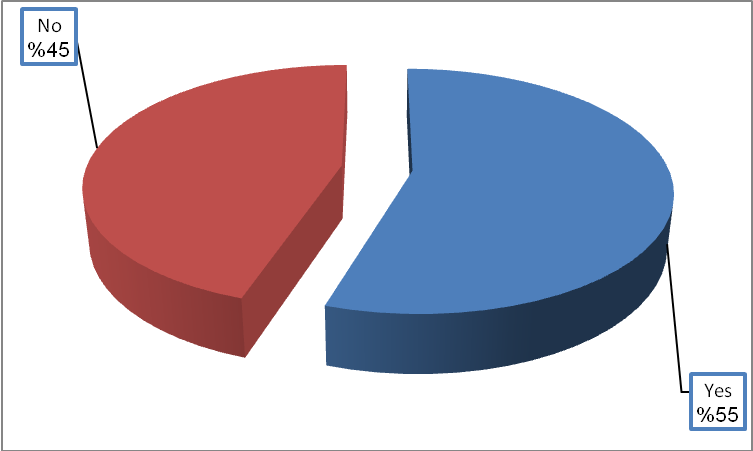
Age distribution (Figure 1). Showed that the common age group in the sample was 0-18 months that represented (41.7%) then 19 month -7 years represented (30%) then 26 - 60 years represented (21.7%) and the less frequent age group was 8-25 years represented (6.7%). Females represented (55%) of the sample and males represented (45%) (Figure 2).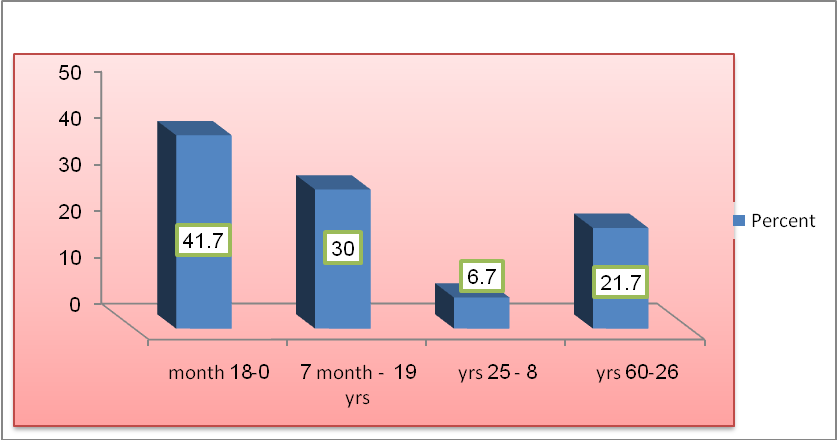 | Figure (1). Showed age group of atopic dermatitis patients in KHD during the period from September 2014 – January 2015 |
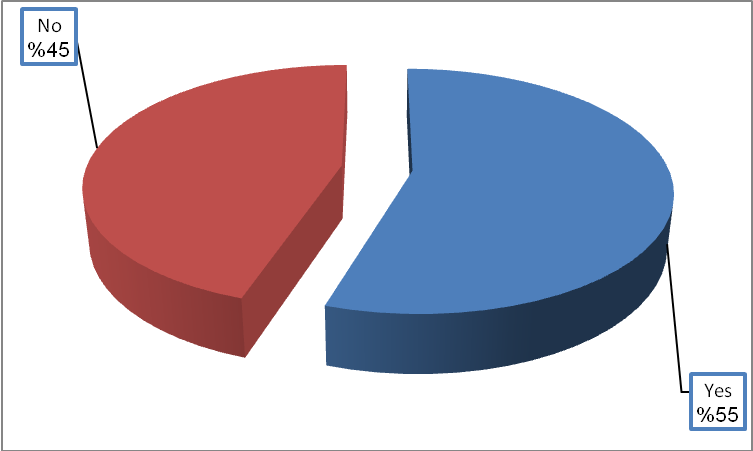
 | Figure (2). Showed gender distribution of AD patient in KDH during the period from September 2014 – January 2015 |
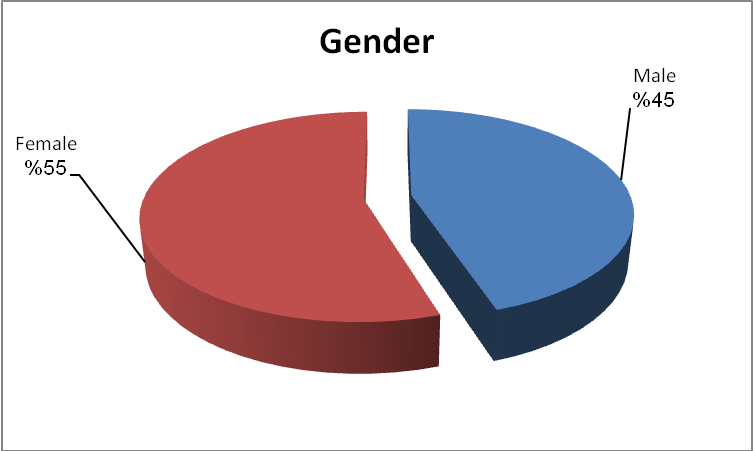
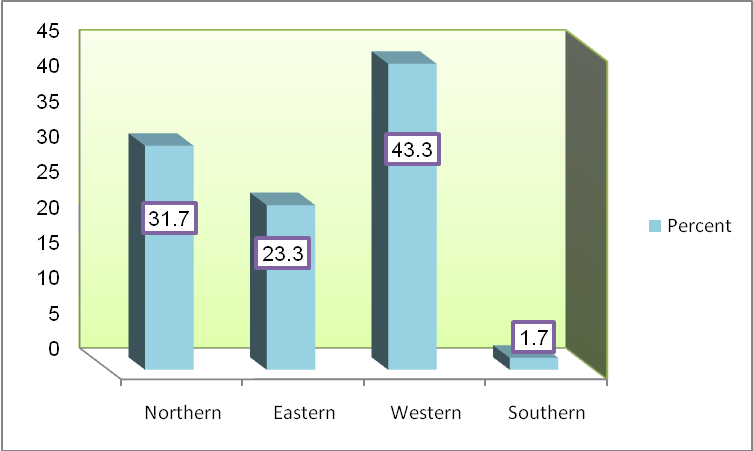
The majority (78.3%) came from central residential areas, (6.7%) from east, (6.7%) from West, (5%) from north and only (3.3%) from south, tribal distribution showed that most of the patients (43.3%) of western tribes, (31.7%) of northern tribes, (23,3%) from eastern tribes and only (1.7%) from southern tribes (Figures 3 and 4).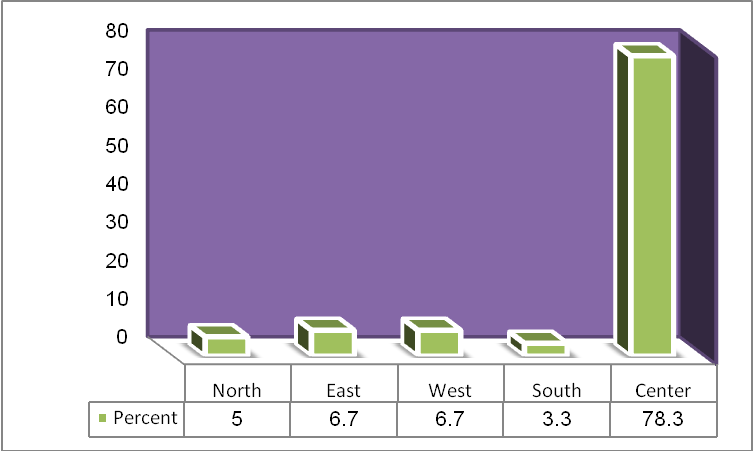 | Figure (3). Showed residence of the AD patient attending KDH during the period from September 2014 – January 2015 |
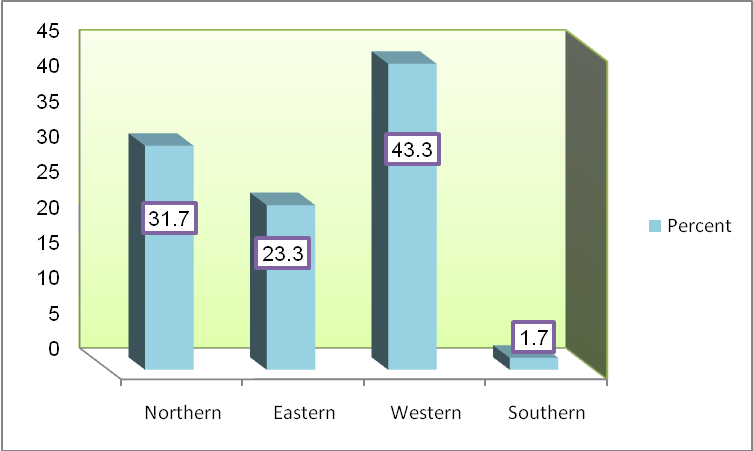 | Figure (4). Showed tribe of AD patients attending KDH during the period from September 2014 – January 2015 |
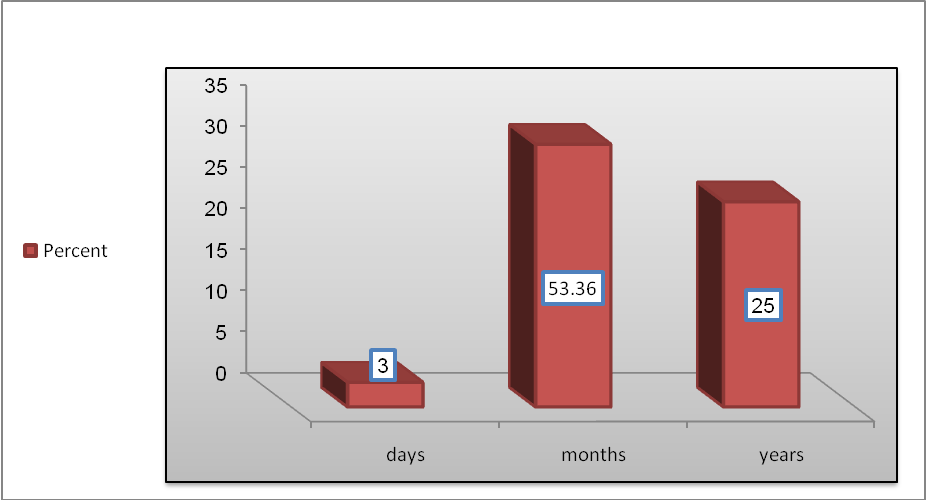
As shown in Figure (5), for most of the patients (53.3%) affected with atopic dermatitis for months, (41.7%) for years and (5%) for days.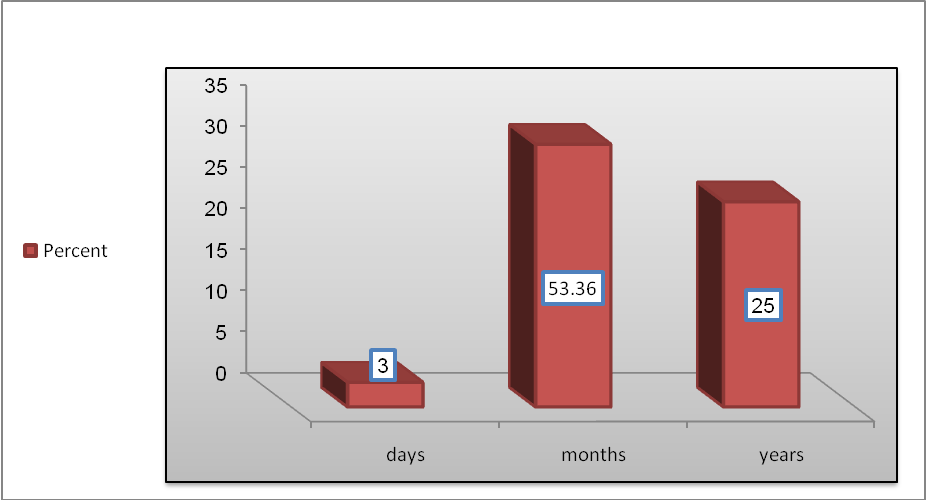 | Figure (5). Showed duration of the atopic dermatitis in patients attending KDH during the period from September 2014 – January 2015 |
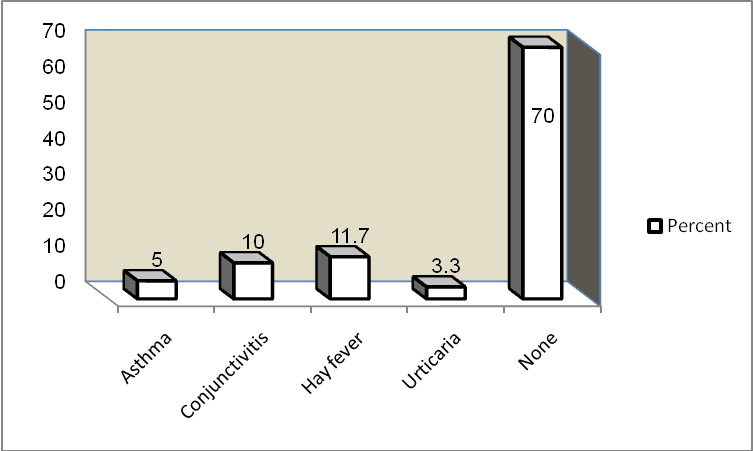
Most of the patients (70%) had no associated condition, the rest of them had Hay fever (11.7%), conjunctivitis (10%), asthma (5%) and urticaria (3.3%) respectively. (Figure 6).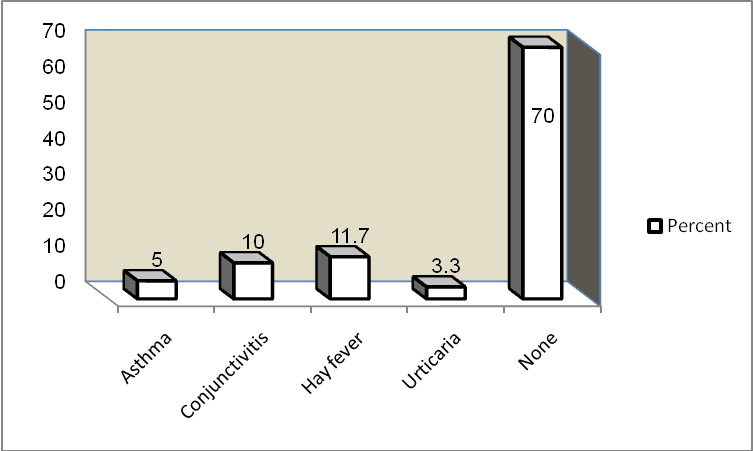 | Figure (6). Showed associated conditions in AD patients in KDH during the period from September 2014 – January 2015 |
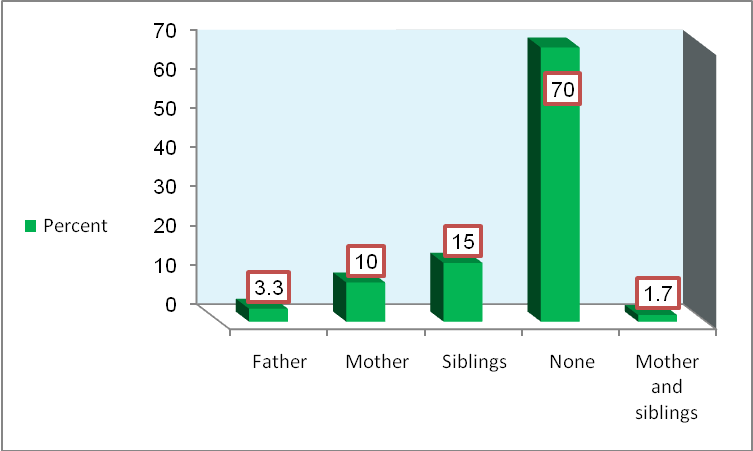
Results in (Figures 7 and 8) showed that similar condition was found in 15% of patients, siblings, (10%) of their mothers (3.3)% of their fathers and (1.7%) of their mothers and siblings. Moreover, family history of atopic diseases was found among (55%) of the patient’s families. 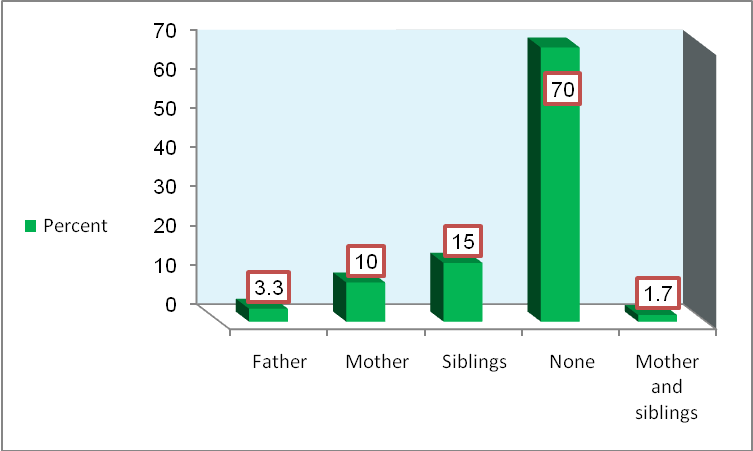 | Figure (7). Showed similar condition in the family in AD patients attending KDH during the period from September 2014 – January 2015 |
 | Figure (8). Showed family history of atopic diseases in AD patients attending KDH in the period from September 2014 – January 2015 |
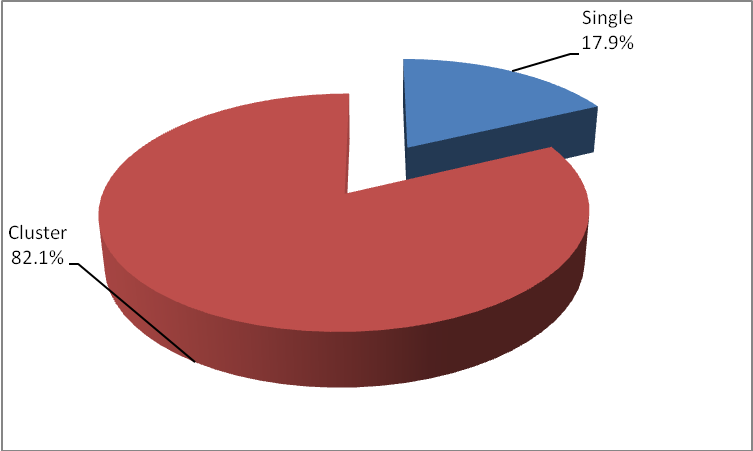
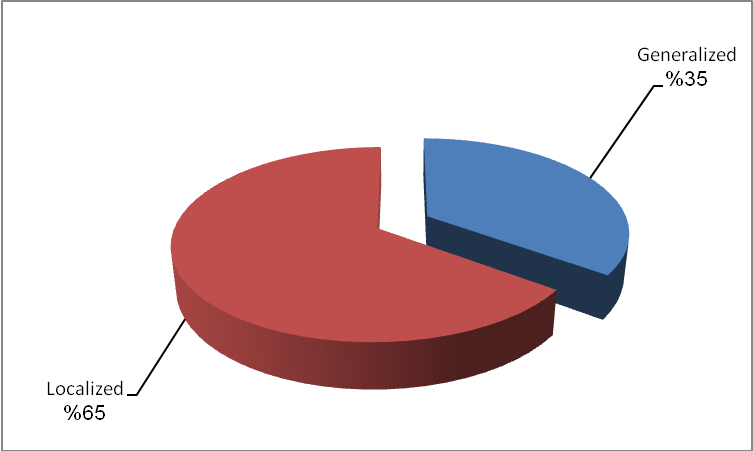
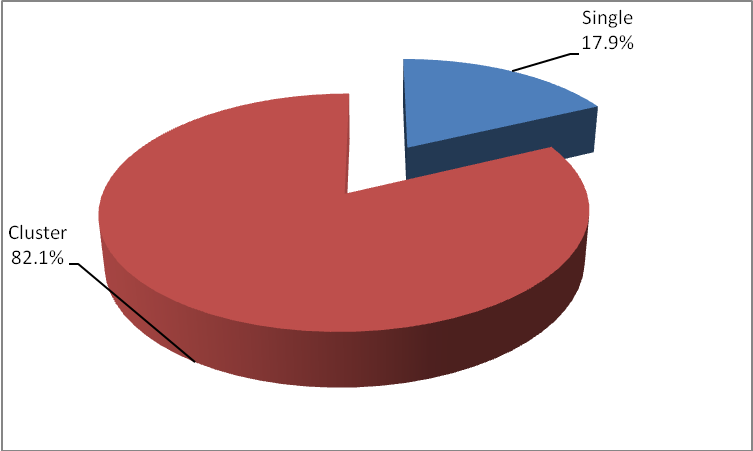
Localized atopic dermatitis was detected in (65%) of the patients, 32 of them represented (82.1%) exhibited cluster type, and seven patients represented (17.9%) was of a single type (Figures 9 and 10).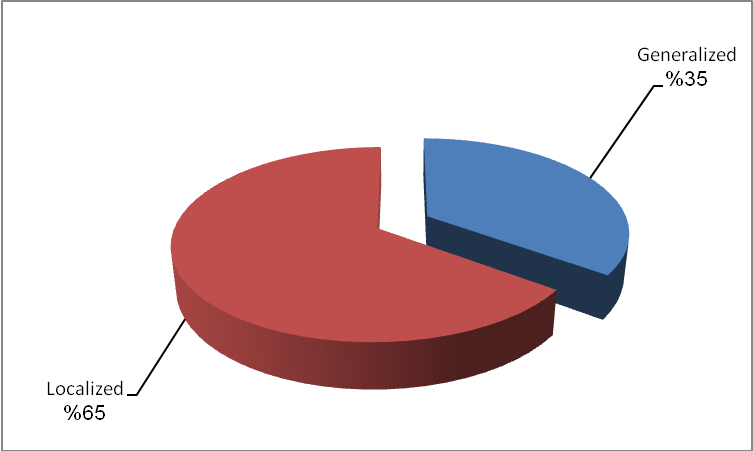 | Figure (9). Showed distribution of the skin lesions in AD patients in KDH during the period from September 2014 – January 2015 |
 | Figure (10). Showed types of localized distribution of lesions in AD patients in KDH during the period from September 2014 – January 2015 |
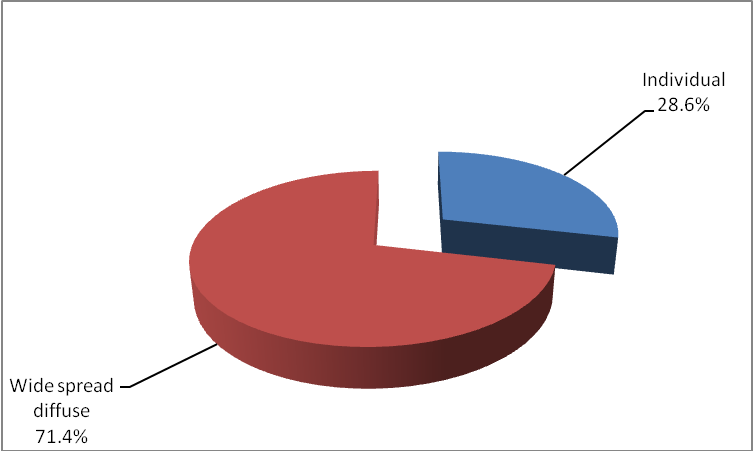
Widespread atopic dermatitis was found among (35%) of the patients, out of the 15 represented (71.4%) exhibited diffuse type, and six patients represented (28.6%) was of a single type ( Figures 9 and 11).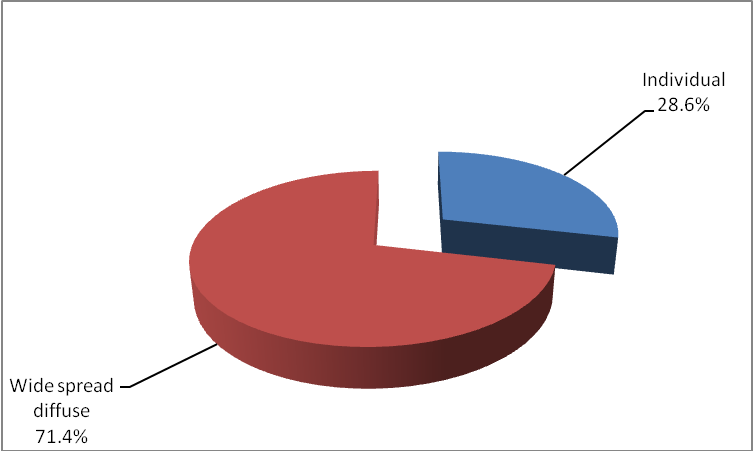 | Figure (11). Showed types of widespread distribution in AD patients in KDH during the period from September 2014 – January 2015 |
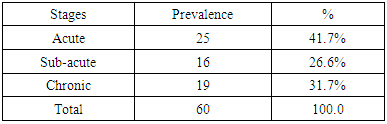
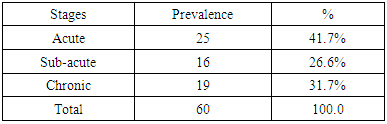
In Table (2) majority of patients presented in acute stage 25 case represented (41.7%) while 19 patient represented (31.7%) were presented with chronic stage and minority16 case represented (26.6%) were in the sub-acute stage.Table (2). Showed stages of atopic dermatitis in AD patients attending KDH in the period from September 2014 – January 2015
 |
| |
|
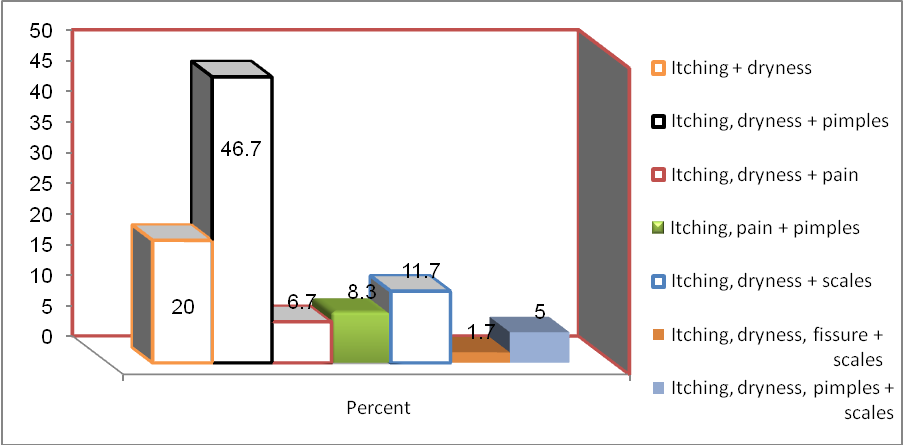
Presenting complaints as shown in Figure (12) include itching, dryness and pimples represented (46.7%), itching and dryness (20%), itching, dryness and scales (11.7%), itching, pain and pimples (8.3%), itching, dryness and pain (6.7%), itching, dryness, pimples and scales (5%) and itching, dryness, fissure and scales (1.7%).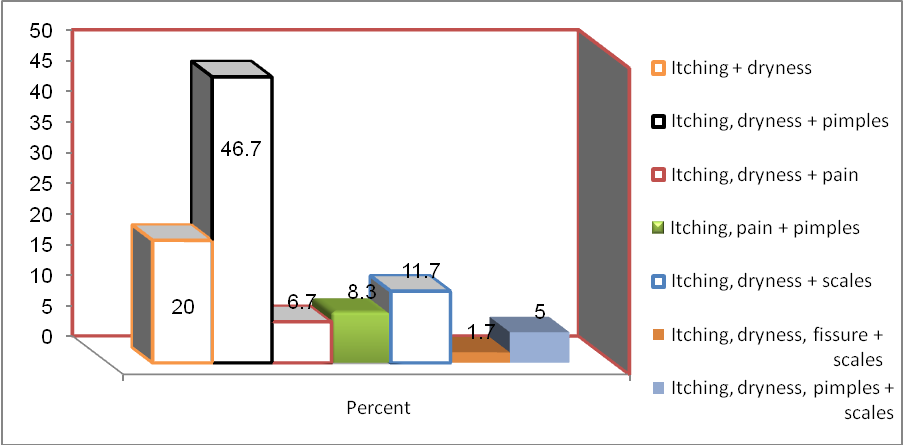 | Figure (12). Showed presenting complain in AD patients attending KDH in the period from September 2014 – January 2015 |
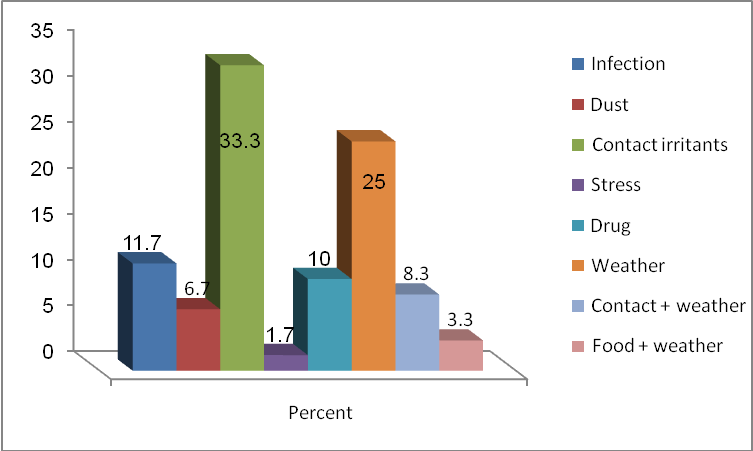
As shown in Figure (13) provocating factors include contact irritants represented (33.3%), weather (25%), infection (11.7%), drug (10%), contact and weather (8.3%), dust (6.7%), food and weather (3.3%) and stress (1.7%) consequently.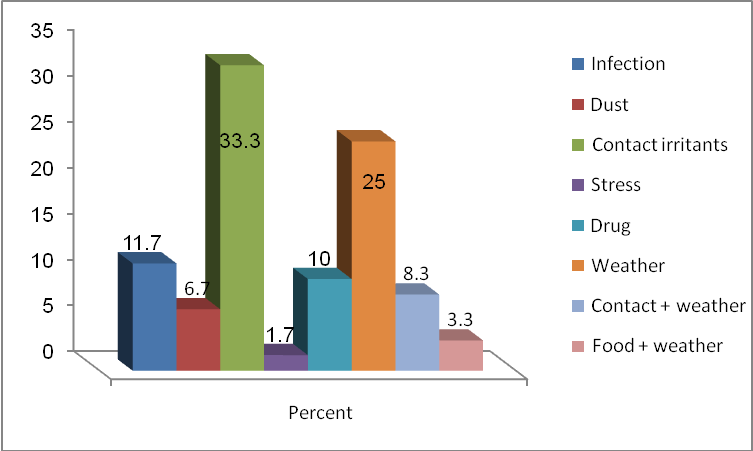 | Figure (13). Showed provocating factors in AD patients in KDH during the period from September 2014 – January 2015 |
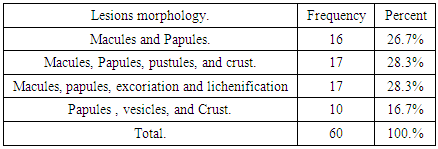
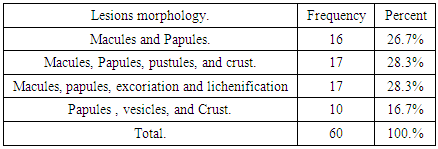
Table (3) showed that lesions morphology were macules, papules, pustules and crust (28.3%), macules, papules, excoriation and lichenification (28.3%), macules and papules (26.7%) and papules, vesicles and crust (16.7%).Table (3). Showed lesions morphology in AD patients in KDH during the period from September 2014 – January 2015
 |
| |
|
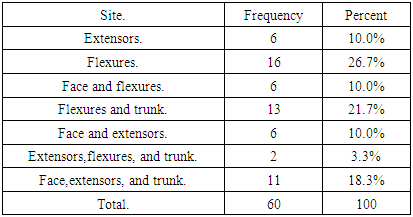
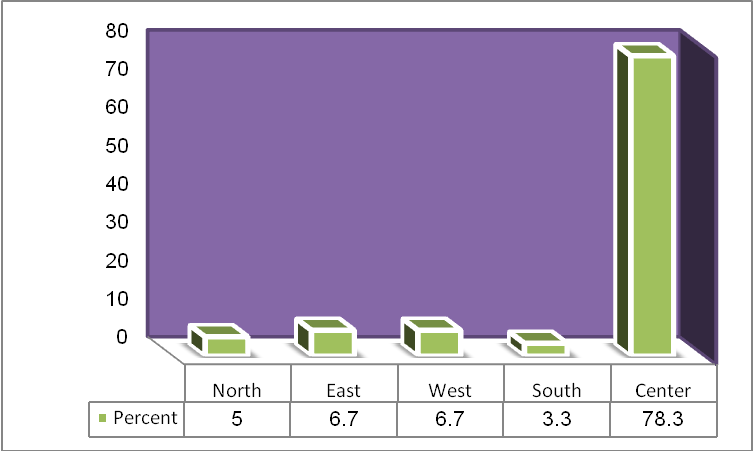
Table (4) showed that the sites of lesions were flexures which represented (26.7%), while flexures and trunk (21.7%), face, extensors and trunk (18.3%), extensors (10%), face and flexures (10%), face and extensors (10%) and extensors, flexures and trunk (3.3%).Table (4). Showed site of the lesions in AD patients in KDH during the period from September 2014 – January 2015
 |
| |
|
3. Discussion
In this study, sixty (60) patients with atopic dermatitis enrolled to identify the epidemiology and clinical patterns of atopic dermatitis in Khartoum Dermatology and Venereology Teaching Hospital.The prevalence of atopic dermatitis among Sudanese patients attending Khartoum hospital in the year 2014 was found to be (1.15%) which is less than The prevalence in the same hospital in 2007 the which was (6.9%), also it is less than in South-Eastern Nigeria [9] as represented (8.5%), US (10.7%) [10] and in Tunis was (8.3%) [11]. It may be due to the difference in weather as Sudan is drier and not like Nigeria that is more humid that act as a provocating factor.The most affected age was infants (0-18 months) represented (41.7%) and the less affected age group was (8-25 years) represented (6.7%) as differs from study done in Khartoum Dermatology and Venereology Teaching Hospital in 2007 that showed the most affected age was (6 months -2 yrs) represented (34.1%) while the less affected age group is (12-18 yrs) represented (7.1%), compared to study in UK [12], with high frequency in age group (6-18 months) represented (25.6%) and less frequency in age-grouped (30 -40 months) represented (19.9%) which might be referred to cold, humid weather.Females affected more than male (55%) and (45%) respectively while sex ratio was equal in a study done in Singapore [13]. Girls outnumbered boys in a ratio of 1.3:1.0 as showed in the study in North Europe [14].The majority in this study, which represented (78.3%) came from central residential areas, and only (5%) from north, while tribal distribution showed that most of the patients represented (43.3%) were from western tribes that are might be due to high consanguinity prevalence in that area lead to increase incidence of AD among them, contact with animal dander, pollens and grass because western of Sudan is area of agriculture and animal grazing, where only (1.7%) came from southern tribes.The majority of the patients in this study represented (53.3%) were suffering from atopic dermatitis for months, while (41.7%) Duration of the condition continues for years and (5%) for days. Thatis indicated a relapsing, and a chronic course was progressive.Most of the patients (70%) had no other atopic diseases, and the minority had Hay fever (11.7%) which is the most common associated atopic disease then conjunctivitis (10%), asthma (5%) and urticaria (3.3%), compared to study in Khartoum Hospital of Dermatology in 2007 hay fever represented (5.8%) then asthma (3.5%) Unlike that study done in North Europe [14] which showed that AD is more often had a personal history of asthma, indicated that increase in frequency of atopic diseases in atopic dermatitis patient most probably due to increasing exposure to inhalant allergens like dust, smoke, house dust mite, and mold.Atopic dermatitis was found in 15% of patient’s siblings, (10%) of their mothers and (3.3%) of their fathers. Moreover, family history of atopic diseases was found among (55%) of the patient’s families most probably due to the high frequency of intermarriage between relatives.Localized atopic dermatitis was found in (65%) of the patients; 32 cases out of them represented (82.1%) showed cluster type and 7 cases represented (17.9%) showed single type. Widespread atopic dermatitis was found among (35%) of the patients, out of the 15 cases represented (71.4%) exhibited diffuse type and 6 cases represented (28.6%) individual-type. So overall patients presented with a localized distribution more than widespread.Most of the patients (46.7%) presented with itching, dryness, and pimples and the least of them presented with itching, dryness, fissure, and scales (1.7%). Over the entire most frequent symptom is dryness and itching associated with pimples most probably due to lack of use of emollient that is the mainstay of treatment beside another treatment.In this study, Irritant contacts like soaps and non-cotton clothes represented (33.3%) were the most provocating factor for AD, that’s might be because patients use soap and water excessively which lead to more irritation and dryness, both cold and hot weather provocative AD in (25%), infection (11.7%), and drug (10%) may be due to using of oral antibiotic containing penicillin mainly that become widely used without medical prescription, contact, and weather (8.3%), dust represented (6.7%) due to increasing air pollution and house dust mite, food and weather (3.3%) it may be attributable to food additives like artificial flavours and colours. Stress represented (1.7%). Most of the patients were presented with macules, papules, pustules, and crust (28.3%), and macules, papules, excoriation and lichenification (28.3%) and least with papules, vesicles, and crust (16.7%).Most of the patients were found an acute stage (41.7%) and the least was in thesub-acute one (26.7%). Acute stages may be associated with systemic symptoms like fever, malaise, and lymphadenitis especially in infants and children, so their parents seek urgent medical advice, unlike the sub-acute and chronic stages.The most common sites of lesions were flexures represented (26.7%), flexures and trunk (21.7%), face, extensors and trunk (18.3%), extensors per se (10%), face and flexures (10%), face and extensors (10%) and extensors, flexures and trunk (3.3%).Although the number of affected infants (41.7%) were more than children and adults separately, the most common sites of lesions were found to be in the flexures (26.7%), than in the extensors (10%), contrast to expected regarding age of the patients which should be coincided with results of extensors in infants this is explained by the number of children and adults together is more significant than infants alone so that the frequency of flexural distribution is more than extensors that it does not conflict with characteristic distribution of AD.
4. Conclusions
The prevalence of atopic dermatitis was found to be (1.15%). Regarding AD patients (55%) had a positive family history while (70%) of patients had no personal history of atopic disease and the rest of them had hay fever (11.7%), conjunctivitis (10%), asthma (5%) and urticaria (3.3%) consequently.
5. Recommendations
1. This study showed that atopic dermatitis is a chronic annoying disease that in the majority of patients has a psychological and social impact. Therefore, explanation of these findings to the patients is recommended to be a crucial part of the management of the disease.2. Further multicentral studies should be performed with large sample size to determine the exact magnitude of the problem.3. It is recommended to encourage the relationship between physician/ and patient for better management of atopic dermatitis.4. Parents should do regular visits to the dermatologist especially in the case of atopic infantile and childhood dermatitis for moral support and a better understanding of the nature of the disease.5. Most of the patients were found to be affected by contact irritants and weather so skin care should be recommended during different seasons. So, it is highly recommended preventing dryness of the skin as possible by applying emollients.6. Atopic dermatitis was found to be precipitated or provocation by secondary infections, so treatment of any disease associated with atopic dermatitis is mandatory.
References
| [1] | Coca AF, Cooke RA. On the Classification of the Phenomena of Hypersensitiveness. J Immunol. 1923 May 1; 8(3): 163–82. |
| [2] | Williams H. Disease definition and measures of disease frequency. J Am Acad Dermatol. 2001 Jul;45(1 Suppl): S33-6. |
| [3] | Hanifin J, Saurat JH. Understanding atopic dermatitis: pathophysiology and etiology. Introduction. J Am Acad Dermatol. 2001 Jul; 45(1 Suppl): S1. |
| [4] | Simpson EL, Hanifin JM. Atopic dermatitis. J Am Acad Dermatol. 2005 Jul; 53(1): 115–28. |
| [5] | Williams HC, Pembroke AC, Forsdyke H, Boodoo G, Hay RJ, Burney PG. London-born black Caribbean children are at increased risk of atopic dermatitis. J Am Acad Dermatol. 1995 Feb; 32(2 Pt 1): 212–7. |
| [6] | Anturaniemi J, Uusitalo L, Hielm-Björkman A. Environmental and phenotype-related risk factors for owner-reported allergic/atopic skin symptoms and for canine atopic dermatitis verified by veterinarian in a Finnish dog population. Simon M, editor. PLoS One. 2017 Jun 1; 12(6): e0178771. |
| [7] | Margolis JS, Abuabara K, Bilker W, Hoffstad O, Margolis DJ. Persistence of Mild to Moderate Atopic Dermatitis. JAMA Dermatology. 2014 Jun 1; 150(6): 593. |
| [8] | Silverberg JI. Persistence of Childhood Eczema Into Adulthood. JAMA Dermatology. 2014 Jun 1; 150(6): 591. |
| [9] | Nnoruka EN. Current epidemiology of atopic dermatitis in south-eastern Nigeria. Int J Dermatol. 2004 Oct; 43(10): 739–44. |
| [10] | Shaw TE, Currie GP, Koudelka CW, Simpson EL. Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health. J Invest Dermatol. 2011 Jan; 131(1): 67–73. |
| [11] | Khaldi F, Fakhfakh R, Mattoussi N, Ben Ali B, Zouari S, Khémiri M. Prevalence and severity of asthma, allergic rhinoconjunctivitis and atopic eczema in "Grand Tunis" schoolchildren: ISAAC. Tunis Med. 2005 May; 83(5): 269–73. |
| [12] | Wadonda-Kabondo N, Sterne JAC, Golding J, Kennedy CTC, Archer CB, Dunnill MGS, et al. A prospective study of the prevalence and incidence of atopic dermatitis in children aged 0-42 months. Br J Dermatol. 2003 Nov; 149(5): 1023–8. |
| [13] | Tay Y-K, Kong K-H, Khoo L, Goh C-L, Giam Y-C. The prevalence and descriptive epidemiology of atopic dermatitis in Singapore school children. Br J Dermatol. 2002 Jan; 146(1): 101–6. |
| [14] | Schultz Larsen F, Diepgen T, Svensson A. The occurrence of atopic dermatitis in north Europe: an international questionnaire study. J Am Acad Dermatol. 1996 May; 34(5 Pt 1): 760–4. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML