-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(2): 15-18
doi:10.5923/j.ajdv.20190802.01

A Case of Porokeratosis of Hands and Feet Turning into a Squamous Cell Carcinoma
Khalifa E. Sharquie1, Fatema A. Al-Jaralla2
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
2Department of Dermatology, College of Medicine, Baghdad University, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology & Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Porokeratosis is comprised of heterogeneous group of diseases that inherited as autosomal dominant pattern. It is a disorder of keratinization characterized by one or more atrophic macules or patches, each surrounded by a distinctive hyperkeratotic, ridge-like border called a cornoid lamella. Multiple clinical variants of porokeratosis exist, some of them have genetic inheritance while others are acquired and malignant transformation occurs in a minority of cases. In Iraq, the inherited commonly described entities of porokeratosis are rarely seen, but every now and then localized forms like porokeratosis of the scrotum and other parts of the body were seen. In addition solar facial porokeratosis is an acquired disease not uncommonly seen in young females which disappear over time. The aim of the present report is to record an unusual case of localised porokeratosis of both hands and feet with multiple squamous cell carcinomas with negative family history.
Keywords: Porokeratosis, Squamous cell carcinoma
Cite this paper: Khalifa E. Sharquie, Fatema A. Al-Jaralla, A Case of Porokeratosis of Hands and Feet Turning into a Squamous Cell Carcinoma, American Journal of Dermatology and Venereology, Vol. 8 No. 2, 2019, pp. 15-18. doi: 10.5923/j.ajdv.20190802.01.
1. Introduction
- Porokeratosis is a clonal disorder of keratinization characterized by one or more atrophic patches surrounded by a clinically and histologically distinctive hyperkeratotic ridge like border called the cornoid lamella. Historically, porokeratosis is a misnomer that was erroneously coined on the assumptions that cornoid lamellae emerged from pores of the sweat glands [1]. Multiple clinical variants of porokeratosis are recognized. Malignancies, typically squamous cell carcinomas, may develop within lesions of porokeratosis.The most common forms of porokeratosis are as follows:Classic porokeratosis of Mibelli (PM) [2].Disseminated superficial actinic porokeratosis (DSAP) and its non-actinic variant disseminated superficial porokeratosis (DSP).Linear porokeratosisPorokeratosis palmaris et plantaris disseminata (PPPD)Punctate porokeratosis, which might represent a variant of PPPD [3].Porokeratosis in general is not a common problem in Iraqi population, but Sharquie et al in 2003 [4], described a new entity; so called solar facial porokeratosis which is commonly seen on the face of young females, which probably will vanish over time as it not seen in later ages without malignancy complications. The common genetic porokeratosis types are very rare in this country, but every now and then we see a localized porokeratosis only in one or two sites of the body like the case described in the scrotum [5].We report a very unusual case of porokeratosis of hands and feet.Malignant transformation can occur in about 7.5% of patients [6-8]. Lesions that are large, long-standing, or linear have the greatest risk of developing an associated malignancy [9]. Chromosomal instability and reduced immune surveillance with overexpression of p53 are hypothesized to play a role in the development of cutaneous malignancies within porokeratosis [10-14].The porokeratosis-associated squamous cell carcinomas may very rarely metastasize and cause death [15, 16].
2. The Present Case
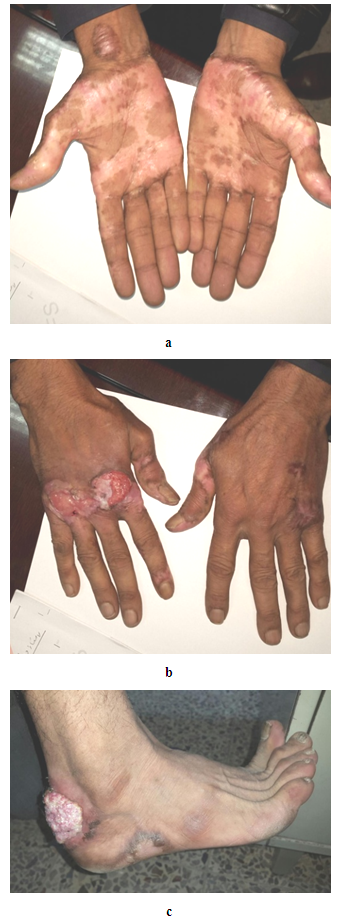
- A 45-year old farmer presented to dermatology centre with a multiple bilateral rash of both hands and feet, since the age of eleven. This rash is mostly asymptomatic except for mild burning and discomfort. No positive family history was recorded. On examination, multiple bilateral well defined depigmented patches with elevated hyperpigmented borders and depressed centres that were located on both dorsal and ventral aspects of the hands and feet and were gradually progressive with time. Multiple tumors that appeared simultaneously within the lesions of porokeratosis of five months duration Figure. 1 a, b and c.
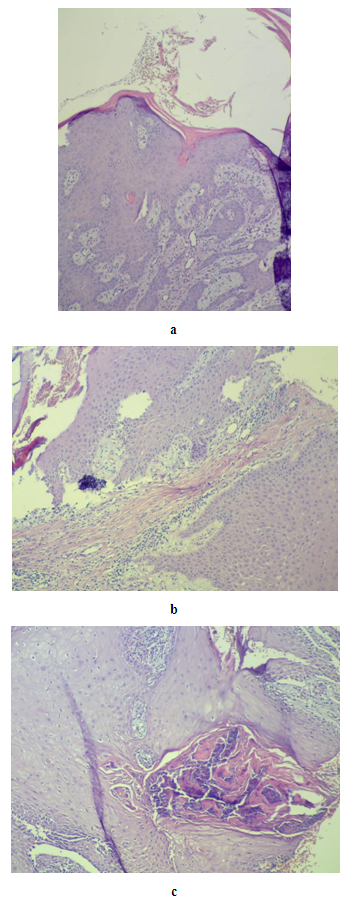 | Figure 2. (a, b, c). Microscopic view showing squamous cell carcinoma and cornoid lamellae H&E stain × 40 (a) H&E stain ×100 (b), and (c) |
3. Discussion
- Porokeratosis is a primary disorder of epidermal keratinization of unknown aetiology. It can be classified into localized and generalized forms. The localized forms include porokeratosis of Mibelli, linear porokeratosis, and punctate porokeratosis, and the generalized variants include disseminated superficial porokeratosis, disseminated superficial actinic porokeratosis, and disseminated palmoplantar porokeratosis [17].The most important complication to watch for is the development of cutaneous malignancy. Large lesions of porokeratosis, linear porokeratosis, or porokeratosis in an immunocompromised patients should be monitored carefully for the development of cutaneous malignancies within the porokeratosis lesions.The present case imposes a diagnostic challenge because of the unusual presentation and the negative family history, the diagnosis of porokeratosis was delayed for years and the patient presented with one of the dreaded complications of this disease; squamous cell carcinoma, on hands and feet. The patient required radiotherapy in addition to surgical excision of the tumors. The occurrence of malignancies in porokeratotic lesions is clinical evidence of the pre- cancerous nature of this disease. Malignancies have been reported for porokeratosis of Mibelli, linear porokeratosis, porokeratosis palmaris et plantaris and DSAP [18-21]. The associated malignancies are squamous cell carcinoma, Bowen's disease and basal cell carcinoma. Squamous cell carcinoma arising in the classic type of porokeratosis of Mibelli is well-documented, but there are only a few reports of squamous cell carcinoma in DSAP [18, 19]. All of the reported squamous cell carcinoma cases arising from DSAP lesions have originated in the distal extremities. These findings indicate that there is a significant role of UV light on the evolution of squamous cell carcinoma from DSAP. In addition, results from previous reports showed that p53 gene mutations are responsible for the progression of porokeratosis to SCC in at least some cases [22].In the present case, the SCC also appeared on sun exposed areas where lesions are located. Also cornoild lamella was observed inside squamous cell carcinoma pathology and this, strongly suggest the possibility that the carcinoma developed from clones of abnormal epithelial cells.
4. Conclusions
- The present case showed this unusual presentation of localized porokeratosis affecting both hands and feet with atypical presentation since the age of eleven but developed multiple carcinomas at the age of 45years. We should emphasize that localized porokeratosis might change into squamous cell carcinoma and the patient should be watched carefully for this complication.
DISCLOSURE
- This study was an independent study and not funded by any drug companies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML