-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(1): 8-13
doi:10.5923/j.ajdv.20190801.03

Slapped Neck Solar Melanosis: Is It a New Entity or a Variant of Poikiloderma of Civatte?? (Clinical and Histopathological Study)
Khalifa E. Sharquie1, Adil A. Noaimi2, Ansam B. Kaftan3
1Department of Dermatology, College of Medicine, University of Baghdad
2Iraqi and Arab Board for Dermatology and Venereology, Dermatology Center, Medical City, Baghdad, Iraq
3Dermatology Center, Medical City, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Poikiloderma of Civatte although is a common complaint among population, especially European, still it was not reported in dark skin people as in Iraqi population. Objectives: To study all the clinical and histopathological features of Poikiloderma of Civatte in Iraqi population. Patients and Methods: This study is descriptive, clinical and histopathological study. It was carried out at the Dermatology Center, Medical City, Baghdad, Iraq, from September 2017 to October 2018. Thirty-one patients with Poikiloderma of Civatte were included and evaluated by history, physical examination, Wood’s light examination. Lesional skin biopsies were obtained from 9 patients, with histological examination of the sections stained with Hematoxylin and Eosin (H&E) and Fontana-Masson stain. Results: Thirty-one patients were included in this study, with mean age +/- SD was 53.32+/-10 years, and all patients were males. Twenty-six patients (84%) were with skin phenotype III&IV, The pigmentation was either mainly erythematous (22.5%), mainly dark brown pigmentation (29%), and mixed type of pigmentation (48.5%). These lesions were distributed on the sides of the neck and the face and the V shaped area of the chest. Twenty-four (77.5%) patients had associated Melasma on their faces. Histopathologically the most prominent finding was the increase in the melanin stores mainly in the basal layer of the epidermis in all the 9 biopsies, with few scattered dermal melanophages in 55%, dilated dermal blood vessels in 78% and mild superficial perivascular mixed inflammatory infiltrate in 55%. Conclusion: This new clinical condition has many features that are different from the ordinary Poikiloderma of Civatte as it is a disease of middle age male patients that appears as pigmentation on the sides of the neck and the face , as if these areas are being slapped by sunlight but no poikilodermatous features. Also there is increase in the melanin stores of the epidermis but no dermal elastosis. Hence this condition deserves the name slapped neck solar melanosis that could be either a new entity or an undescribed variant of Poikiloderma of Civatte.
Keywords: Poikiloderma of Civatte, Slapped Neck Solar Melanosis, Basal melanin stores
Cite this paper: Khalifa E. Sharquie, Adil A. Noaimi, Ansam B. Kaftan, Slapped Neck Solar Melanosis: Is It a New Entity or a Variant of Poikiloderma of Civatte?? (Clinical and Histopathological Study), American Journal of Dermatology and Venereology, Vol. 8 No. 1, 2019, pp. 8-13. doi: 10.5923/j.ajdv.20190801.03.
Article Outline
1. Introduction
- Poikiloderma of Civatte, is acquired poikiloderma of the face and neck, a common benign dermatosis often affecting fair-skinned, middle-aged and elderly people. It symmetrically involves the sides and V-shaped area of the chest as well as the lateral parts of the face, with sparing of anatomically shaded areas [1]. Incidence and prevalence are unclear as mild cases are underreported [2]. It is most often seen in women at a premenopausal stage [3]. Lighter-skin phototypes (I–III) are more commonly affected, as well as those engaged in outdoor occupations or leisure activities [4].The etiopathogenesis of PC appears to be multifactorial. Involvement of sun-exposed areas of the neck and face, while anatomically shaded areas are spared, suggests that solar radiation plays a major role [4]. Familial cases of PC have been reported, and a genetic basis has been suggested [5]. It has also been speculated that photoactive substances in perfumes and cosmetics possibly induce a photo allergic or photoxic reaction that triggers the disease process [4, 6].The condition is often asymptomatic, but occasionally, a mild pruritus or a burning sensation is reported [3, 4]. Based on the predominant clinical feature, PC has been classified into erythematotelangiectatic, pigmented, and mixed types [3]. Among them, the erythematotelangiectatic type appears to be the most common [7]. Poikiloderma of Civatte has slowly progressive and irreversible course [2].Poikiloderma of Civatte is histopathologically characterized by thinning of the spinous layer, hydropic degeneration of the basal cell layer, presence of melanophages in the papillary dermis and dilatation of the papillary dermal capillaries [2, 8].During the daily clinical practice, we had noticed many cases of Poikiloderma of Civatte, exclusively among adult males, despite the fact that the rash was different from what has been described in the classical cases of PC, still, the distribution of the rash was in the same sites. There was always a doubt whether these cases are actual cases of PC or represent a different condition.Hence, the objectives of the present work are to record all the cases of this condition and to be compared with PC in order to reach a final conclusion whether this condition is a part of PC or a different skin problem.
2. Patients and Methods
- This is descriptive, clinical and histopathological study that was carried out in the Dermatology Center, Medical City, Baghdad, Iraq, from September 2017 to October 2018. A total of 31 male patients were included in this study, all of them had Poikiloderma of Civatte- like skin lesions in the sides of neck and upper anterior chest. Their ages ranged from 39-74 years, with mean age +/- SD 53.32 +/- 10 years.
2.1. Inclusion Criteria
- Patients clinically presented with two or more of the followings: erythema, telangiectasia, atrophy, hypo- or hyper-pigmentation involving sides of neck, sides of face and upper chest, were included in this study.
2.2. Exclusion Criteria
- Any patient presented with Congenital Poikiloderma, Poikiloderma due to connective tissue diseases and Poikilodermatous Mycosis Fungoides, and Poikiloderma due to topical steroids and other medications or radiotherapy were excluded from this study.
2.3. History
- Full history was taken from all the patients including the following: age, occupation, history and duration of outdoor sun exposure, duration of disease, site of lesions, any symptom like itching and burning, any exacerbating factors, and history of regular use of perfumes, family history of the same condition, medical history and drug history. All patients did not present to the Dermatology center complaining from Poikiloderma of Civatte, instead they were either companions of other patients or seeking medical advice for other dermatological disorders.
2.4. Physical Examination
- Clinical examination was done for each patient regarding the following:Site, size, shape, edge and color of lesions, degree of erythema, pigmentation and atrophy, type and severity of telangiectasia, skin phenotype and associated Melasma. Also, full evaluation of skin, mucous membranes, hair and nails was carried out.
2.5. Wood’s Light Examination
- Was done for all patients to assess the depth of pigmentation whether epidermal, dermal or mixed.
2.6. Histopathological Evaluation
- Incisional biopsies from lesional skin were taken from 9 patients for histopathological examination. Hematoxylin and Eosin stain in addition to Fontana-Masson stain were done for all these biopsies. Histopathological examination was done using light microscope Micros.Informed consent was taken from all included patients after full explanation about the nature, course, complications, and prognosis of the disease and the procedure of biopsy before taking biopsy of the skin and before taking photographs of the lesions in the same places with good illumination. IPhone 6Splus camera was used for photography. The ethical approval was obtained from Scientific Council of Dermatology and Venereology – Iraqi Board for Medical Specializations.
3. Results
3.1. Clinical Study
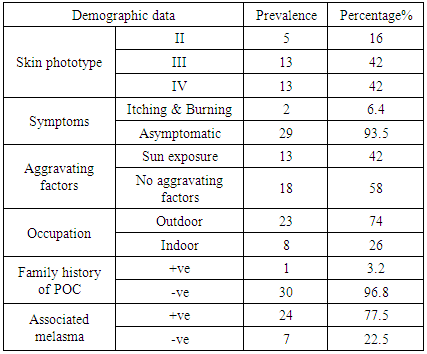
- Thirty one patients with the Piokiloderma of Civatte-like skin lesions were included in this study, all were males, and the mean age 53.32 +/- 10 SD years.Five (16%) out of 31 patients had skin phenotype II, 13 (42%) patients had skin phenotype III while 13 (42%) had skin phenotype IV.All patients had obvious pigmentation and erythema that were distributed symmetrically on the sides of the neck extending up to retro auricular area, sparing the anatomically shaded sites including the sub mental region and skin fold, with 26 (84%) patients had involvement of the V shaped and upper central chest.Six (19.5%) patients had extension of pigmentation into the mandibular area, and 13 (42%) patients had involvement of the sides of the face.Those lesions were distributed on the sides of the neck and the face in a way as if those sites are being slapped by sunlight.The lesions were either erythematous in 7 (22.5%) patients, dark brown pigmentation in 9 (29%) patients, and mixed type of pigmentation in the remainder 15 (48.5%) patients.The actual picture of Poikiloderma was not fulfilled in all the patients of the current study. Still 6 (19%) patients had some atrophy in the involved area, and minimal telangiectasia was noticed in 18 (58%) of patients.All patients had gradual onset and did not complaint from this medical problem and considered it as a cosmetic problem and not an actual disease. Still after detailed questioning, 2 (6.4%) patients mentioned that they experienced some itching and burning sensation, especially on outdoor activities.Twenty three (74%) patients reported having significant sun exposure with an outdoor occupations or activities, while 8 (26%) had an indoor occupation and did not had history of extensive sun exposure.Thirteen (42%) patients reported exacerbation in intensity of rash with sun exposure, and the other 18 (58%) did not report any exacerbating factors.Twenty four (77.5) of the 31 patients had typical melasma involving their foreheads, cheeks and other sites on their faces.Only one (3.2%) patient reported positive family history of Poikiloderma of Civatte in his father.
|
3.2. Wood’s Light Examination
- All patients showed increase in the contrast of pigmentation with wood’s light, indicating an epidermal pattern of pigmentation.
3.3. Histopathological Findings
3.3.1. Hematoxylin and Eosin Stain
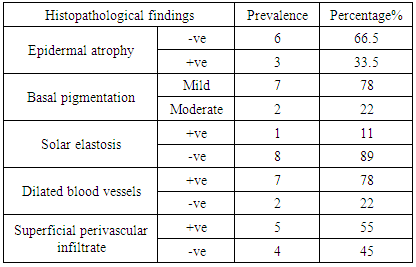
- The epidermis showed atrophy, mainly flattening of rete ridges in 3 (33.5%) of patients.All of the 9 patients showed increased basal Melanosis, 7 (78%) of them was mild degree, and the other 2 (22%) showed moderate increase in basal pigmentation.The dermis showed dilated superficial blood vessels in 7 (78%) patients with mild mixed superficial perivascular inflammatory reaction in 5 (55%) patients, and solar elastosis was identified in a single patient.Focal damage to basal layer with a band of hyalinization of basal cell layer and increased vascularity was detected in a single biopsy.
3.3.2. Fontana – Masson Stain
- Using this stain all patients showed intense basal Melanosis, 7 (78%) demonstrated mild supra-basal Melanosis and the other 2 (22%) had intense supra-basal pigmentation that extends up to stratum corneum.Dermal melanophages were scanty in number, and were detected in 5 (55%) biopsies.
|
4. Discussion
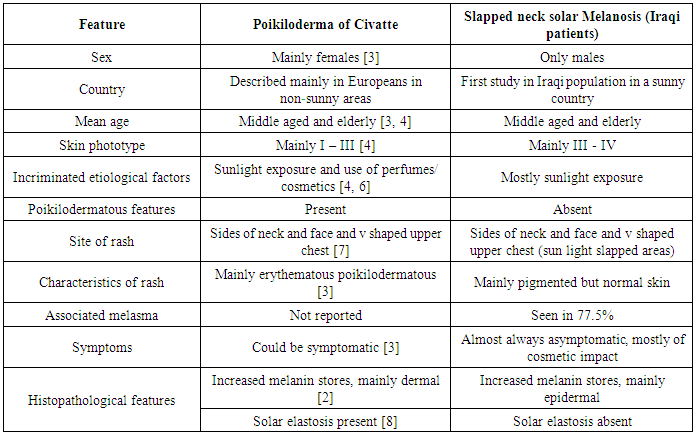
- The present study showed marked differences between PC and the clinical features of the patients of the present work (Table 3).Looking at the table 3, there are many features in this new condition which are absent in Poikiloderma of Civatte but commonly seen in Iraqi patients, which can be summarized as follow:This disease is seen in Middle East, including Iraq, seen exclusively in males, mostly affecting individuals with skin phototype III and IV, where sunlight exposure is incriminated as the major etiological factor. The rash is mainly pigmented and distributed on the areas that are slapped by sunlight, mainly the sides of the neck, sides of the face and V shaped area of the chest. But the features of Poikiloderma as atrophy, telangiectasia, hypo and hyperpigmentation are not evident in Iraqi patients. Melasma is a common association in this disease. Lastly, the histopathological features are different, as the melanin stores are increased mainly in the epidermis and solar elastosis is lacking.Hence we can conclude that this condition is either a new entity by itself or a described new variant of Poikiloderma of Civatte. And since sunlight was strongly incriminated in its pathogenesis and it is clinically involving the sides of the neck and the face as if they are being slapped by sunlight, this condition deserves the name Slapped Neck Solar Melanosis.
 | Figure 1. Fifty-one year old male showed en erythematous rash on the sides of the neck and V shaped area of the chest, but there were no features of Poikiloderma |
 | Figure 2. Fifty-six year old male showed pigmentation on the sides of the neck and retro auricular area, but there were no features of Poikiloderma |
 | Figure 3. Forty-three year old male showed mixed type of pigmentation with little erythema on the sides of the neck, but there were no features of Poikiloderma |
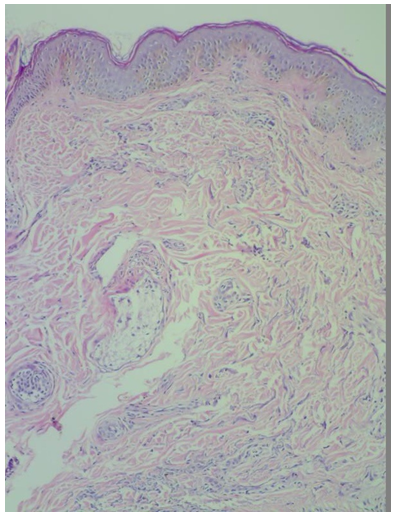 | Figure 4. Increased basal melanin stores with mild superficial and deep mixed perivascular inflammatory infiltrate. Heamatoxylline and Eosin stain. X40 |
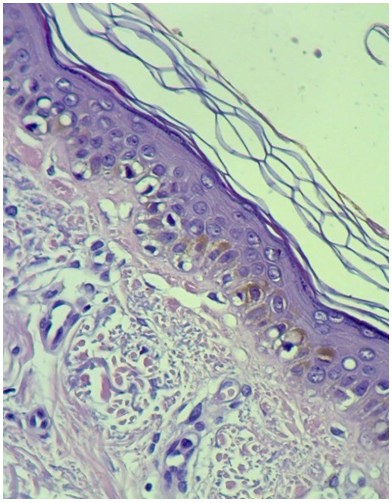 | Figure 5. Epidermis is flattened with mild atrophy, increased basal melanin stores with dilated superficial blood vessels. Hematoxylin and Eosin stain. X400 |
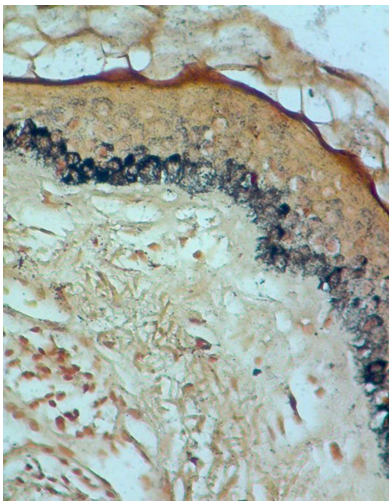 | Figure 6. Epidermis is flattened and atrophied, intense increase in basal melanin stores with mild suprabasal pigmentation. Fontana-Masson stain. X400 |
|
5. Conclusions
- The condition described in this study is not an uncommon problem among Iraqi population where only males are affected in their middle ages and it is only of cosmetic concern.The pigmented variety was the commonest type, in contrast to European countries where the erythematous type is the predominant one.The main site of involvement is the neck, but melasma was also seen among these patients.The histopathological evaluation showed increase in the epidermal melanin stores with no dermal melanosis, in contrast to European studies in which only dermal melanosis was reported.In all these cases sunlight was strongly incriminated in the eitiopathogenesis, hence slapped neck solar melanosis is a term that is suitable for this medical condition.
ACKNOWLEDGEMENTS
- I would like to express my special thanks and gratitude to Doctor Salwa F. Alani and Doctor Ghaith A. Altameemi for their support, technical help and writing assistance.
DISCLOSURE
- This study was independent and not funded by any drug company or organization.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML