-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(1): 5-7
doi:10.5923/j.ajdv.20190801.02

Can Post Blast Injury Sarcoidal Foreign Body Granuloma Change into Systemic Sarcoidosis in the Future?
Khalifa E. Sharquie1, Salwa F. Alani2
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology and Venereology, Dermatology Center, Medical City, Baghdad, Iraq
2Dermatology Center, Medical City, Baghdad, Iraq
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Explosive blasts can cause multiple forms of damage that are more complex than those caused by other wounding agents. Wounds or penetrating injuries accidentally contaminated with silica may be followed some years later by the formation of a sarcoid like foreign body granulomatous reaction. It usually remains localized to the skin but sometimes migration of foreign material via lymphatic's to regional lymph nodes leading to nodal granulomas and rarely to systemic organs, hence can simulate systemic sarcoidosis clinically and histopathologically. In this report, we described a 37 year old man, a victim of blast injury in 2014 with retained shells in the right side of face, neck and left palm and damage of the right eye, presented with 10 months history of asymptomatic papulonodular eruption limited to sites previously traumatized by shell explosion and it was associated with right cervical, right submandibular and left parotid lymphadenopathy. Histopathology report revealed well demarcated, naked and noncaseating granulomas in both skin and lymph node specimens. Careful evaluation shows no systemic involvement but follow up is recommended to detect any further progression of the disease in the future. Although there are thousands of victims of blast injury encountered in Iraq since the United States led coalition forces invasion in 2003, this is the first reported case of sarcoidal foreign body granuloma post blast injury in Iraqi population and this could be related to genetic susceptibility to sarcoid granuloma and sarcoidosis and we can assume this genetic diathesis is absent in Iraq as ordinary sarcoidosis is very rarely reported in this country.
Keywords: Sarcoidosis, Blast injury, Foreign body granuloma, Iraq
Cite this paper: Khalifa E. Sharquie, Salwa F. Alani, Can Post Blast Injury Sarcoidal Foreign Body Granuloma Change into Systemic Sarcoidosis in the Future?, American Journal of Dermatology and Venereology, Vol. 8 No. 1, 2019, pp. 5-7. doi: 10.5923/j.ajdv.20190801.02.
1. Introduction
- Several publications regarding the delayed effect of traumatic embedding of foreign bodies in the skin appeared first in the 1930s and 1950s. Wounds or penetrating injuries accidentally contaminated with silica contained in sand, soil, rocks and glass may be followed some years later by the formation of a foreign body reaction. The period between inoculation and development of a reaction may be as long as 25 years [1].Some theories have been published concerning the possible pathogenesis of silica granulomas. It has been suggested that silica must be in a soluble (colloid) form to elicit a tissue reaction. The latent period observed clinically might represent the time required in body tissues to convert insoluble forms of silica to soluble forms capable of eliciting a granulomatous response. Also there are some thoughts suggesting that silica may be involved in the pathogenesis of certain cases of ordinary sarcoidosis [2].Ordinary cutaneous sarcoidosis occurs preferentially within scar tissue, at traumatized skin sites, and around embedded foreign material such as silica. Scars become inflamed and infiltrated with sarcoidal granulomas. Inflammation of old scars may go parallel or precede systemic sarcoidal disease activity. Hence scar sarcoidosis may be the only cutaneous finding in a patient with systemic sarcoidosis [3].The histopathological differential diagnosis between cutaneous lesions of systemic sarcoidosis and cutaneous sarcoid granulomas of other aetiology may be very difficult. For this reason, the detection of non‐caseating granulomas in the skin is not sufficient to confirm the diagnosis of sarcoidosis in the absence of other organ involvement [4]. Those cases with cutaneous sarcoid granulomas of unknown aetiology are better considered as idiopathic sarcoid reactions. These patients should be followed up because some of them will develop involvement of other organs and thus fulfill the diagnostic criteria for sarcoidosis [4].
2. Case Description
- A 37 year old man, a victim of blast injury in 2014 with retained shells in the right side of face, neck and left hand and damage of the right eye, presented with 10 months history of asymptomatic papulonodular eruption limited to sites previously traumatized by shell explosion including right side of face and neck and left palm. The rash was asymptomatic except for its cosmetic appearance. The patient's family and medical histories were non remarkable. Physical examination revealed pigmented-brownish firm papules and nodules limited to the right side of face, neck and left hand, associated with right cervical, right submandibular lymphadenopathy and left parotid enlargement (Figures -1, 2). The lungs and heart were clear and no hepatosplenomegaly was noticed on clinical examination. Ophthalmologic evaluation, including slit-lamp examination, did not reveal ocular involvement suggestive of sarcoidosis, but vision was impaired in the right eye.
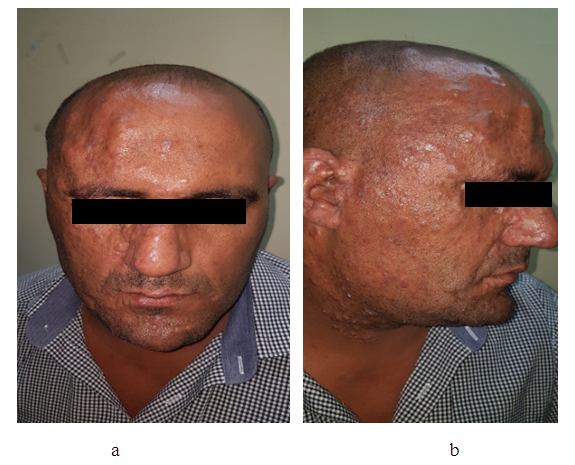 | Figure 1. Showing a 37 year male patient with post blast foreign body sarcoidal rash of face (a,b) |
 | Figure 2. Showing the left palm of the same patient affected by foreign body sarcoidal rash |
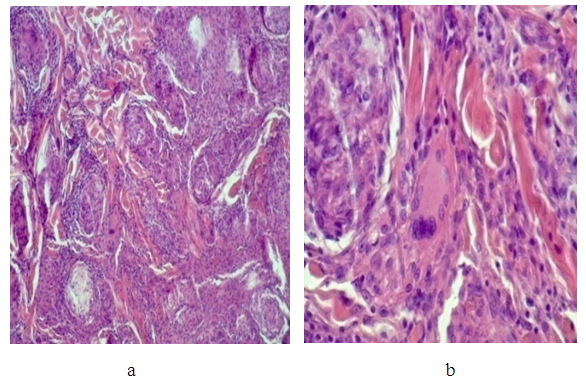 | Figure 3. H&E stained section of skin showing well demarcated naked non caseating granuloma (a- low mag.x40 and b-high mag.x400) |
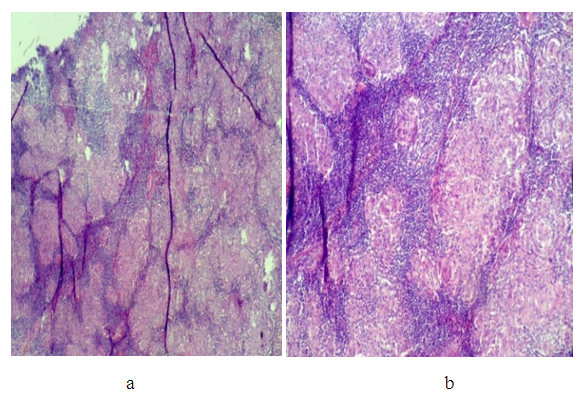 | Figure 4. H&E stained section of Lymph node showing well demarcated non caseating granuloma (a- low mag.x40 and b-medium magx100) |
3. Discussion
- Explosive blasts can cause multiple forms of injuries that are more complicated than those caused by other ordinary wounding agents. The acute physical and psychological impacts in those who survive blast explosions can be great and devastating. The long term consequences are less clear [5].Although there are thousands of victims of blast injury encountered in Iraq since the United States led coalition forces invasion in 2003, this is the first reported case of sarcoidal foreign body granuloma post blast injury in Iraqi population and as sarcoidosis is very rare in Iraq, so we can speculate that there is no genetic susceptibility for sarcoid granuloma and sarcoidosis in Iraqi people.The current case represents a typical picture of blast explosion related sarcoidal foreign body granuloma, where biopsy specimens of both skin and lymph node showed classical sarcoidal granulomatous reaction. This reaction can sometimes be the only sign of cutaneous or underlying systematic sarcoidosis. So in such cases it is appropriate to conduct additional studies and regular follow-up.A confirmed diagnosis of sarcoidosis requires proof of granulomatous involvement in at least two separate organs [6]. In the present case, there were typical well demarcated, naked and noncaseating granulomas in both skin and regional lymph nodes. This could be related to possible migration of foreign material via lymphatic's to regional lymph nodes leading to nodal granulomas and palpable lymphadenopathy.We could not conduct further tests that help to assess systemic involvement like serum angiotensin-converting enzyme level, gallium 67 scan and PET scan, because there were not available at the time being in Baghdad.In this case, several features support the diagnosis of foreign-body granulomas: skin lesions limited to traumatized sites, the absence of generalized lymphadenopathy or hepatosplenomegaly, and the lack of ophthalmologic and skeletal findings. But regular follow up is required as we assume that genetic susceptibility to develop sarcoid granuloma may predispose the patient to develop systemic sarcoidosis in the future.
4. Conclusions
- Although blast injuries is a common problem in Iraqi population but sarcoid foreign body granuloma, to the best of our knowledge, is not reported in Iraqi medical literature. This is the first case to be reported that shows typical picture of post blast sarcoidal foreign body granuloma whereas systemic sarcoidosis could not be excluded and further follow up is essentially needed to detect any further progression of the disease in the future.
Disclosure
- This case report was independent and not funded by any drug company or organization.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML