-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2019; 8(1): 1-4
doi:10.5923/j.ajdv.20190801.01

Strange Case of Kaposi's Sarcoma that Followed PRP Injection of Lesion
Khalifa E. Sharquie1, Adil R. Al-Saadawi2, Fatema A. Al-Jaralla3
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology &Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
2Department of Pathology, Baghdad Medical City Complex, Baghdad, Iraq
3Department of Dermatology, College of Medicine, Baghdad University, Baghdad, Iraq
Correspondence to: Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board for Dermatology &Venereology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Kaposi's Sarcoma is a spindle-cell tumor thought to be derived from endothelial cell lineage. This condition carries a variable clinical course ranging from minimal mucocutaneous disease to extensive organ involvement. In Iraq, there are upsurge of cases of Kaposi's since 1991 as a result of exposure to depleted uranium in South of Iraq and South to Baghdad. We report one case of Kaposi's sarcoma in a 27 year old female with a history of face PRP injection in very early course of the disease and she presented with a nine months history of bilateral asymmetrical dusky red plaques involving the periorbital area, cheeks, followed by spread to other parts of body like chest, arms and thighs. The diagnosis was confirmed by histopathological findings on biopsy, and positive HHV-8 immunostaining. PRP injection might share in the aggressive course of Kaposi's sarcoma and its rapid spread to other parts of body.
Keywords: Kaposi's Sarcoma, PRP Injection, Strange case, Iraq
Cite this paper: Khalifa E. Sharquie, Adil R. Al-Saadawi, Fatema A. Al-Jaralla, Strange Case of Kaposi's Sarcoma that Followed PRP Injection of Lesion, American Journal of Dermatology and Venereology, Vol. 8 No. 1, 2019, pp. 1-4. doi: 10.5923/j.ajdv.20190801.01.
1. Introduction
- Kaposi's sarcoma (KS) is a type of spindle cell malignancy that arises from the vascular endothelium, usually presenting as violaceous papules and plaques. KS is a multifocal systemic disease with four principal clinical variants: 1- chronic or classic KS; 2- African endemic KS, including a fulminant lymphadenopathic type; 3- KS due to iatrogenic immunosuppression; 4-AIDS-related epidemic KS. Cutaneous lesions can vary from pink patches to dark violet plaques, nodules or polyps, depending on clinical variant and stage. All clinical variants are viewed as virally induced disease, with human herpes virus-8 (HHV-8) the implicated agent [1]. Typically classic KS follows a benign course and predominantly occurs in elderly people, particularly men of Mediterranean, Eastern European, or Middle Eastern descent [2, 4]. African lymphadenopathic KS is aggressive, often terminating fatally within 2 years of onset. Also AIDS-related KS has a fulminant, progressive course with nodal and systemic involvement. While the course of the disease is variable in patients who develop immunosuppression-related KS from causes other than AIDS [5]. In Iraq, the striking difference is the great increase in the number of the cases. In a previous study, 21 patients were seen in a period of 10 years, while a study published in 2003 recorded 20 patients in one year in the same centre. This increase in the frequency of the cases might be related to depleted uranium exposure during Gulf war in 1991 [6] and the disease is still increasing till now. The course of this Kaposi's sarcoma is rapid and more aggressive and wide spread that seen in more younger people.Platelet-rich plasma (PRP) is an autologous preparation of platelets in concentrated plasma. Various growth factors, including platelet-derived growth factor (PDGF), transforming growth factor (TGF), vascular endothelial growth factor (VEGF), and insulin-like growth factor (IGF), are secreted from the α-granules of concentrated platelets activated by aggregation inducers. These factors are known to regulate processes including cell migration, attachment, proliferation and differentiation, and promote extracellular matrix (ECM) accumulation by binding to specific cell surface receptors.Due to the presence of high concentrations of these growth factors, PRP has been used in a wide variety of surgical procedures and clinical treatments, including the treatment of problematic wounds and maxillofacial bone defects, cosmetic surgeries, and gastrointestinal surgeries [7]. The objective of present paper is to present unusual and strange case of KS which had very rapid and aggressive course that followed PRP injection at the initial lesion of undiagnosed Kaposi 's lesion of face.
2. The Present Case
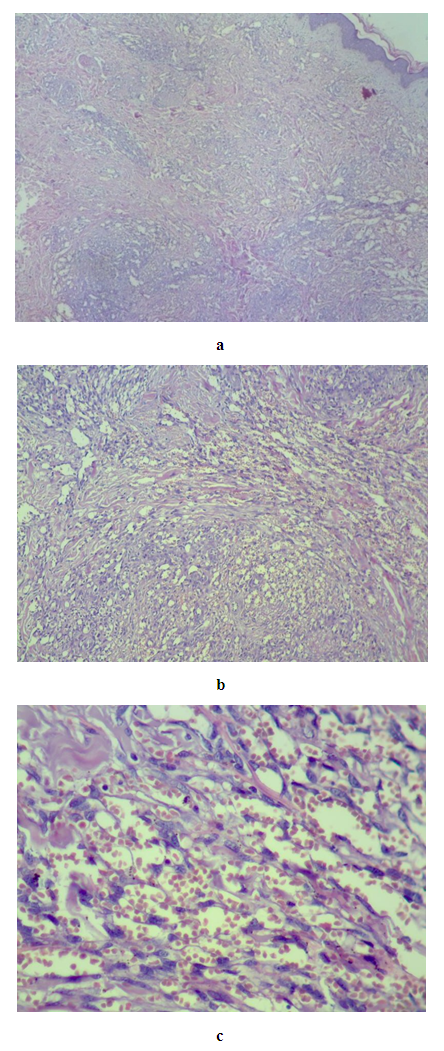
- A 27-year old female presented to skin department with a facial rash and swelling of nine months duration and the condition started as bruise-like discoloration and slight swelling around both eyes which slowly increased over three months “Figure. 1”. The patient seeked private clinic in Jordan and skin biopsy showed mucin deposition and she was received peri-ocular PRP injections “Figure. 2”, afterwards, new lesions appeared more rapidly in the face and then after months other parts of the body skin were affected and the patient felt severely ill with difficulty in breathing and swallowing.
 | Figure 1. Showing swelling and bruises around the eyes as initial manifestation of the disease and before PRP injection |
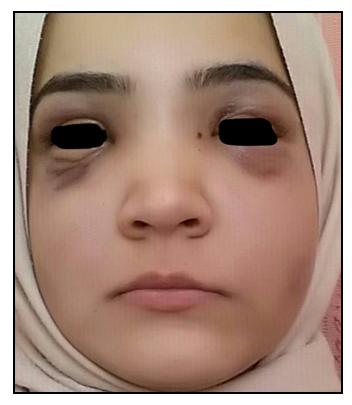 | Figure 2. The patient at 3 months duration, bruise like discoloration and slight swelling around both eyes short time after PRP injection |
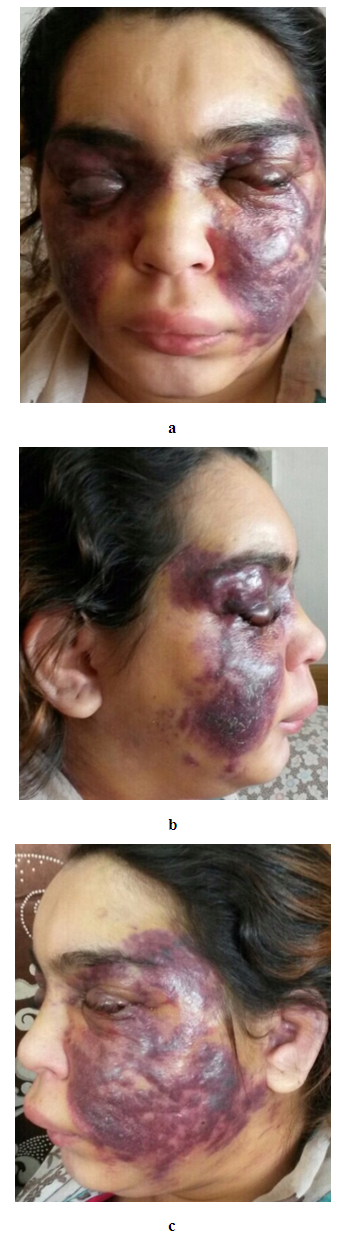 | Figure 3(a, b, c). The patient at time of presentation with multiple bilateral asymmetrical dusky red plaques, nodules and swelling involving the periorbital area, cheeks and parts of ear lobes |
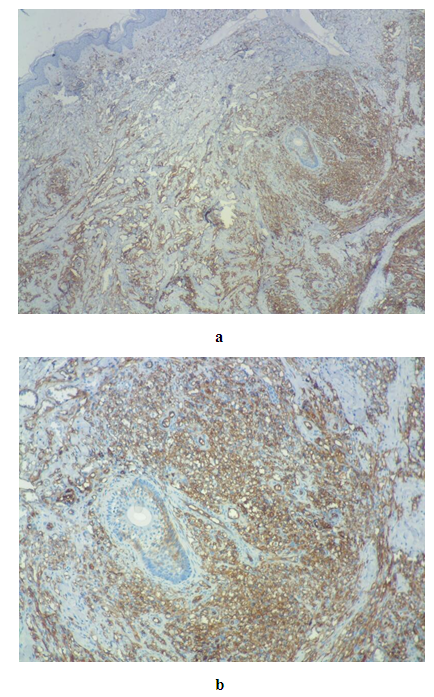
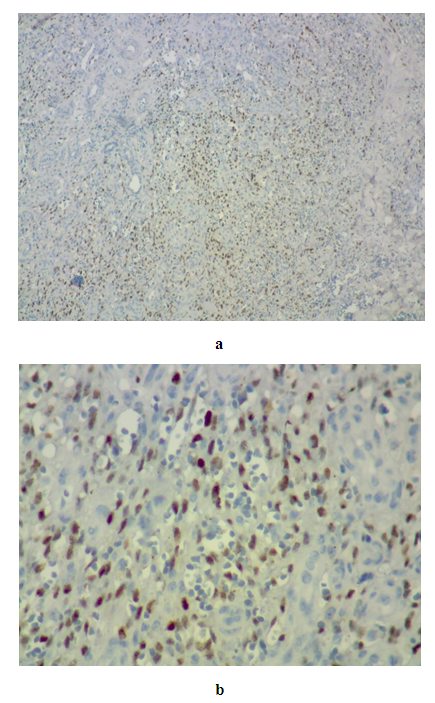 | Figure 5(a, b). HHV-8 positive immunostaining a × 40, b × 400 |
 | Figure 6(a, b). PositiveCD34 staining; a × 40, b × 100 |
3. Discussion
- The present case had many unusual features mainly, the initial sites of involvement as started around eyes in apparently healthy female. Also there was no history of preceding ill health or a disease. There were no history of immune suppressive disease or drug intake but with rapid aggressive course, she received PRP intralesional injection at the very early initial course of the disease which followed by severe deterioration in the skin rash and general health. All these features make this present case very unique that necessitates its rapid reporting.Platelet-rich plasma (PRP) means abundant platelets that are concentrated into a small volume of plasma. The pivotal discovery of platelet-derived growth factor (PDGF) in promoting wound healing, angiogenesis and tissue remodeling threw light on this novel autologous therapeutic modality [8].Degranulation of the pre-packaged GFs in platelets occurs upon "activation" i.e., on coming in contact with coagulation triggers. The secreted GFs in turn bind to their respective transmembrane receptors expressed over adult mesenchymal stem cells, osteoblasts, fibroblasts, endothelial cells, and epidermal cells [9]. The possible correlation between aggressive and relatively rapid development of KS in the present patient and PRP is unclear and needs further investigation but we can speculate that these growth factors had helped in the spread of the disease and behaving aggressive course. Accordingly, we recommend that any suspected case of KS should not be given PRP injection.
4. Conclusions
- Very strange aggressive case of KS in a young apparently previously healthy female without any immunosuppressive agents and the rash started as bruises-like around the eyes that became aggressive and rapidly spreading after periorbital PRP injection.
Disclosure
- This study was an independent study and not funded by any drug companies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML