-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2018; 7(1): 1-5
doi:10.5923/j.ajdv.20180701.01

The Prevalence of Vitiligo Variants in Association with Helicobacter pylori Infection
Tamara A. A. Abdelmoneim1, Ahmed N. Aljarbou2, 3, Khalid O. Alfarouk3, Sari T. Alhoufi4, Abdel Rahman M. A. Ramadan4, Adil H. H. Bashir5
1Department of Medicine, University of Medical Sciences and Technology, Khartoum, Sudan
2College of Pharmacy, Qassim University, Burydah, Al-Qassim, KSA
3Al-Gahd International Colleges for Applied Medical Sciences, Al-Madinah Al-Munawarah, KSA
4Taibah University, Al-Madinah Al-Munawarah, KSA
5Institute of Endemic Diseases, University of Khartoum, Khartoum, Sudan
Correspondence to: Adil H. H. Bashir, Institute of Endemic Diseases, University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2018 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

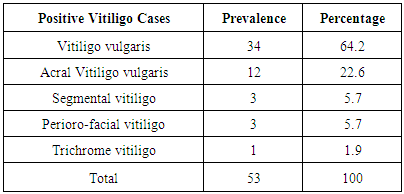
Background: More than 50% of the world’s population is infected with H. pylori (Helicobacter pylori). Its prevalence continues to increase and is more prevalent in developing countries and those living in unsanitary conditions. On the other hand; Vitiligo is a progressive disease of unknown etiology, poorly responding to treatment and has a severe impact on patient's lives. Objectives: This study is aimed to determine the prevalence of vitiligo variants and to detect whether or not there is an association between vitiligo and H. pylori infection. Patients and Methods: An observational case finding hospital-based study was carried out over a period of 3 months from October 2011-December 2011. A total of 64 vitiligo patients attended the clinic in Al Jawda Medical Centre in Khartoum; the patients had a thorough medical history taken from them and underwent a complete physical examination, and were tested for H. pylori using different laboratory methods. Questionnaires with relevant information have been completed. Results: H. pylori showed 53 positive cases out of the total number of 64 vitiligo cases which revealed an H. pylori prevalence of (82.8 %) which is considered as very high incidence rate. However, statistically, a p-value of more than 0.05 (p-value 0.729) renders it statistically insignificant and therefore an association between vitiligo and H. pylori is unlikely. The commonest vitiligo variant diagnosed in those with a positive H. pylori infection was Vitiligo vulgaris which constituted 64.2% of the total number of cases. Conclusion: There was a very high prevalence rate of H. pylori among vitiligo patients, and this should urge further larger scale research specifically well-designed case controls or cohorts regarding the association between vitiligo and H. pylori infection.
Keywords: Vitiligo, Helicobacter pylori, Sudan
Cite this paper: Tamara A. A. Abdelmoneim, Ahmed N. Aljarbou, Khalid O. Alfarouk, Sari T. Alhoufi, Abdel Rahman M. A. Ramadan, Adil H. H. Bashir, The Prevalence of Vitiligo Variants in Association with Helicobacter pylori Infection, American Journal of Dermatology and Venereology, Vol. 7 No. 1, 2018, pp. 1-5. doi: 10.5923/j.ajdv.20180701.01.
Article Outline
1. Background
- Helicobacter pylori, previously named Campylobacter pyloridis, is a Gram-negative, microaerophilic bacterium found in the human stomach. It was first identified and isolated in 1982 by Barry Marshall and Robin Warren, who concluded that it was present in patients with chronic gastritis and gastric ulcers. Colonization of the stomach with H. pylori leads to a variety of upper gastrointestinal disorders, such as chronic gastritis, peptic ulcer disease, gastric mucosa-associated lymphoid tissue (MALT) lymphoma. It is the first formally recognized bacterial carcinogen and is linked to the development of gastric cancer. [1].
2. Introduction
- More than 50% of the world's population harbor H. pylori in their upper gastrointestinal tract. [2] The prevalence of H. pylori in industrialized countries is relatively constant and remains under 40% and is lower in children/adolescents than in adults/senior citizens. Within geographical regions, the prevalence of H. pylori inversely correlates with socioeconomic status and in relation to living conditions during childhood. [1] Infections are usually acquired in early childhood, and if left untreated may persist throughout a person’s lifetime. H. pylori are contagious, although the exact route of transmission is not known, direct person-to-person transmission via the oral-oral or fecal-oral or gastro-oral route is most likely. [3] Food prepared in less than ideal conditions or exposed to contaminated water or soil may increase the risk of transmission of H. pylori. Lack of hygiene, low social class, and high-density living conditions seem to be related to a higher prevalence of H. pylori infection as transmission of H. pylori is facilitated. Accurate and simple tests for the detection of H. pylori infection are available. They include serologic tests, urea breath tests, stool antigen tests, and endoscopic biopsies which are available in hospital or clinic settings. [4]On the other hand, Vitiligo is an acquired pigmentary disorder of the skin and mucous membranes, and it is characterized by circumscribed depigmented macules and patches. Vitiligo is a progressive depigmentation disorder resulting from an autoimmune response targeting epidermal melanocytes. Vitiligo affects 0.5-2% of the world population, and the average age of onset is 20 years. [5] Vitiligo is a multifactorial polygenic disorder with a complex pathogenesis. Although several theories have been proposed about the pathogenesis of vitiligo, the exact cause is unknown. Generally agreed upon principles are an absence of functional melanocytes in vitiligo skin and a loss of histochemically recognized melanocytes, owing to their destruction. Current complex theories regarding the destruction of melanocytes include autoimmune mechanisms, cytotoxic mechanisms, and an intrinsic defect of melanocytes, oxidant-antioxidant mechanisms, and neural mechanisms. [5, 6] The most accepted hypothesis is the autoimmune theory which is based on the presence of melanocyte-specific antibodies that can initiate necrosis of cultured human melanocytes. [7] The most widely used classification of vitiligo is localized (Focal, Segmental, Mucosal), generalized (Acrofacial, Vulgaris, Mixed) and universal types and is based on the distribution. When progression, prognosis, and treatment are considered, vitiligo can be classified into two major clinical types: segmental and non-segmental.RationaleThis study was raised as a proposal trying to correlate between Vitiligo and H. pylori infection as highly antigenic bacterium.Vitiligo is well known as one of the autoimmune diseases and H. pylori is also known as highly antigenic bacterium, and then proposed as possible underlying cause for Vitiligo.
3. Purpose of the Study
- H. pylori have been reported to affect approximately 50 percent of the world’s population [8], and recent evidence suggests that H. pylori infection plays a role in the pathogenesis of a variety of skin diseases. The eradication of H. pylori has been shown to be effective in a number of patients with chronic autoimmune urticaria, psoriasis, alopecia areata and Schönlein-Henoch purpura. Conflicting data exists regarding the association of H. pylori infection with Behçet’s disease, scleroderma, and autoimmune bullous diseases. [9]Despite the magnitude and high incidence of H. pylori, no research has been conducted to determine if an association between vitiligo and H. pylori infection is present. In recent literature, an association between H. pylori and extra-digestive manifestations has been proposed. One large clinico-epidemiological study carried out by Bashir et al 2011 [10] on 3,723 Sudanese patients, to detect the prevalence of extra-digestive (extra-gastric) H. pylori skin manifestations, and to determine the influence of H. pylori eradication through triple therapy. The study was conducted on patients with the clinical prognosis of patients with chronic idiopathic urticaria (CIU), Urticarial vasculitis, Atopic dermatitis and some other skin conditions. This study revealed that 20.6% (746/3723) of the skin cases examined have extra-digestive H. pylori skin manifestations. Authors of this study highly recommended performing H. pylori test is in suspected skin cases; skin diseases associated with gastric, respiratory and joint manifestations, as well as diabetes mellitus and vascular manifestations. Since H. Pylori positive cases (37.0%) dramatically responded to H. pylori eradication therapy and 60.8% showed a good clinical response, authors also recommended commencing 12 weeks of eradication antimicrobial triple therapy. [10] H. pylori is a very common bacterium that has become a burden to many communities, health systems and those it manifests on whether financially, socially or psychologically. On the other hand, vitiligo is a deforming disease with an increasing incidence. This study is aimed to determine the prevalence of vitiligo variants and to detect whether or not there is an association between vitiligo and H. pylori infection.
4. Patients and Methods
- An Observational case-finding hospital based study was conducted at the Dermatology clinic at the Al Jawda Medical Centre JMC, Khartoum, Sudan. The study duration was a total of 6 months, from September 2011 till February 2012. The study subjects were patients attending the dermatology outpatient clinic in the specified period. Those clinically diagnosed with vitiligo underwent an H. pylori test through either H. pylori ICT, ELISA, or a Stool Antigen test. All vitiligo variants have been included in the study. In total 64 patients attended the dermatology clinic during the specified period. A detailed history was obtained from patients, and then a thorough physical examination was performed by the consultant dermatologist. A clinical diagnosis of vitiligo according to the distribution of lesions was made by the dermatologist. The skin lesions were reported and documented considering the distribution, configuration, morphology and colour of the lesions. All patients diagnosed with vitiligo underwent a set of H. pylori confirmatory investigations.
5. Results and Discussion
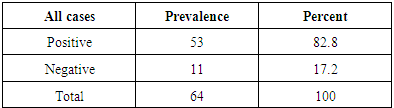
- Data was entered from the questionnaires and later analyzed by the Statistical Package for the Social Sciences (SPSS) version 20. The significance of testing was conducted using a Chi- square test and a p-value of 0.05 or less was considered significant.Background characteristics of those diagnosed with vitiligoA total of sixty-four patients were diagnosed with vitiligo and were included in this study. Of those, 36 (56.3%) of them were females, and 28 (43.8%) were males. When the respondents were classified according to their different ages, it was found that 25 (39.1%) fell within the (20 – 39 years) age group. Whereas 19 (29.7%) were between the ages of (40 – 64), with an average age of 26 years among those included in the study. Upon classification of the study subjects according to marital status, 36 (56.3%) were found to be single whereas 23 (35.9%) were married and a minority were divorced or widowed, two and three patients, respectively. Since the clinic is located in the capital, Khartoum, naturally most patients (96.9%) were from urban regions whereas two patients traveled from rural areas. Forty-nine (76.6%) patients were originally from the North of Sudan, whereas only 6 (9.4%) originated from the West. Five patients (7.8%) were from East Sudan, and four patients (6.3%) were originally from central Sudan. When patients were classified according to their level of education, 20 (31.3%) patients were found to have received primary level education, whereas 43 (67.2%) were found to have either secondary or university education.The most notable symptom patients presented with was hypopigmentation in 38 (59.4%) patients. A minority complained of additional symptoms such as pruritus and dryness of the skin accompanying the skin hypopigmentation. A total of 60 (93.8%) patients were found to have a history of disease duration lasting years except for 4 (6.3%) patients who noted a history of days or months. When physically examined, the majority of patients (76.6%) had widespread, scattered, bilateral and symmetrical cutaneous lesions, while only a minority had localized single or clustered lesions. The morphology of individual lesions among the study subjects was documented and showed that 55 (85.9%) of them were found to have both macules and patches, whereas 6 (9.4%) were found to have macules or patches (3.7%) only. When the color of lesions among study subjects was examined, it was noted that 35 (54.7%) of the patients were found to have milky white lesions, whereas 13 (20.3%) were found to have porcelain white lesions. Eleven (17.2%) had trichrome vitiliginous lesions, and only one patient had erythematous lesions. After a clinical diagnosis of vitiligo was made, vitiligo cases were classified according to the distribution of lesions as presented in the figure 1 below. The majority of patients, 40 (62.5%) were found to have Vitiligo vulgaris.
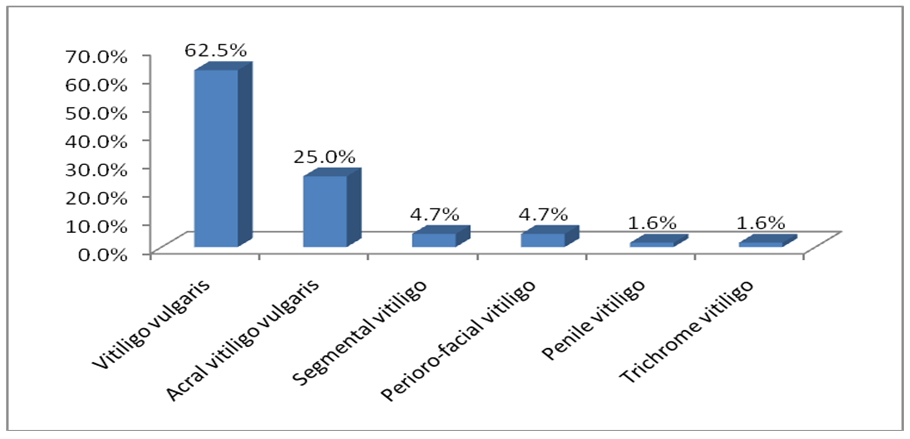 | Figure (1). Showed the Diagnoses of Vitiligo variants (n=64) |
|
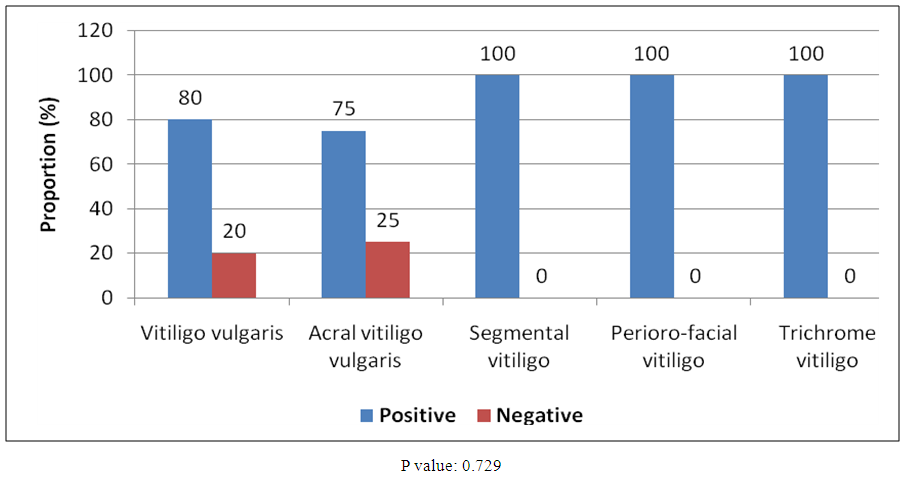 | Figure (2). Showed the relationship between vitiligo and H. pylori (n=63) |
|
6. Conclusions and Recommendations
- This study revealed that 53 H. pylori positive cases out of the total number of 64 vitiligo cases, which resulted in an H. pylori prevalence of 82.8%. This prevalence rate, though considered high, showed a p-value of more than 0.05 (p-value: 0.729) which rendered it statistically insignificant in spite of the high association between Vitiligo and H. pylori positive cases. This should call for further controlled study.1) Although H. pylori infection is primarily confined to the gastric mucosa, evidence in the current literature suggested its association with various several extra digestive diseases [10]. 2) Eradication of H. pylori has proven to be effective in some cases of autoimmune urticaria, psoriasis, alopecia areata and Schönlein-Henoch purpura [10]. The evidence is marginal regarding the association of H. pylori infection with Behçet’s disease, scleroderma, and autoimmune bullous diseases and currently, few researches has been conducted on the association of H. pylori infection with other skin autoimmune diseases, such as vitiligo.3) This should urge larger scale systematic studies evaluating the relationship between H. pylori and dermatologic diseases as well as documentation of the effect of H. pylori eradication therapy on these different diseases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML