Nisreen A. O. Mustafa1, Abdel Rahaman M. A. Ramadan2, Khalid O. Alfarouk3, Ahmed Aljarbou3, Gamal O. Elhassan4, Abdel Khalig Muddathir5, Intisar A. Bashir5, Anas E. Halloul6, Adil H. H. Bashir7
1Khartoum Dermatology Teaching Hospital, Khartoum, Sudan
2College of Dentistry, Taibah University, Al-Madinah Al-Munawarah, KSA
3Al-Ghad International for Applied Medical Sciences, Al-Madinah Al-Munawarah, KSA
4Uneizah College of Pharmacy, Al-Qassim University, Qassim, KSA
5Faculty of Pharmacy, University of Khartoum, Khartoum, Sudan
6School of Public, University of South Florida, Tampa, Florida, USA
7Institute of Endemic Diseases, University of Khartoum, Sudan
Correspondence to: Adil H. H. Bashir, Institute of Endemic Diseases, University of Khartoum, Sudan.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
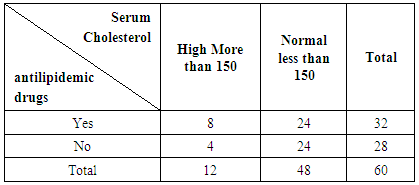
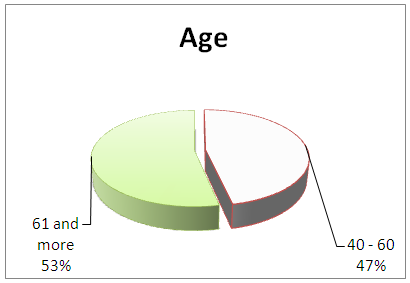
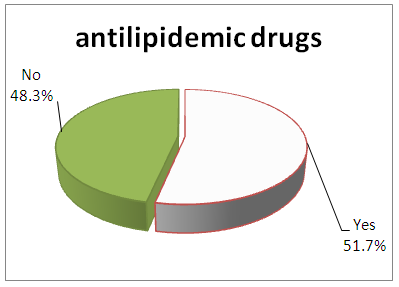
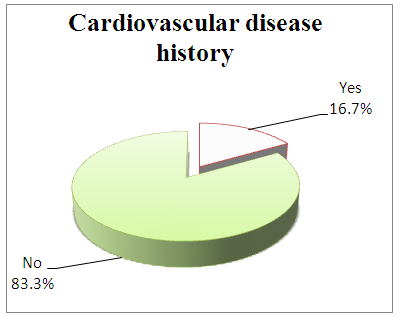
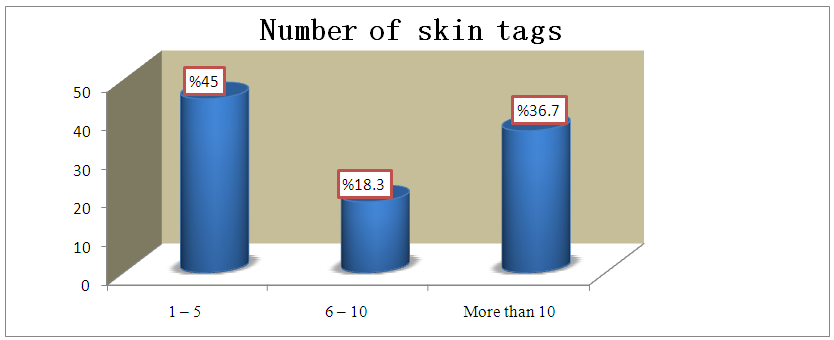
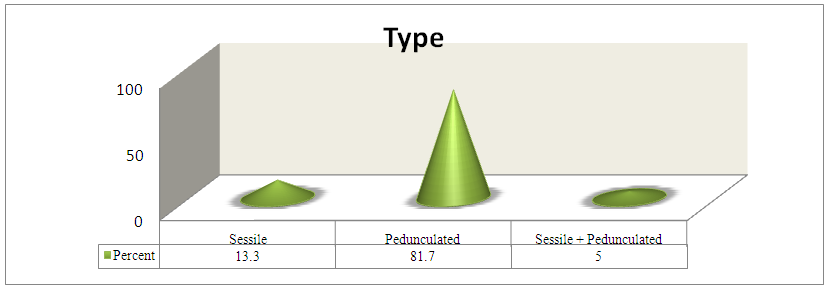
Introduction: Skin tags are common skin lesions, and they been reported that they might reflect insulin resistance states, and also state that the atherogenic profile is associated with diabetes mellitus, particularly the type 2 form, but not exclusively. The studies suggested that skin tags may be an important physical sign that should alert the clinician to look for possible impaired glucose tolerance or diabetes mellitus in patients who manifest them. Also, the presence of the atherogenic lipid profile should also be looked for in these individuals. Clinical signs can aid those patients for health care screening, and skin tags may be an indicator of higher cardiovascular risk that could be useful in general practices. Objectives: To correlate the relationship between Skin Tags, DM2 and atherogenic lipid profile. Patients and Methods: This is a cross sectional, observational, descriptive prospective hospital based study conducted in Jabir Abu Eliz Diabetes center outpatient clinic in the period from August to November 2015. Included 60 Diabetics type 2 patients presented with skin tags with known or unknown atherogenic history, with 20 patients as a control population. All patients underwent data collection using previously designed questionnaire, clinical examination, tested for lipid profile including Triglyceride, Cholesterol and analyzed by computer using SPSS program. Results: This study showed that skin tags study sample were 60 patients represented 9.4% of DM patients (640 patients). (Figure 1) Showed that higher prevalence was found in age group more 61 years represented 53.3%, while figure 2 showed that males were the more dominant with skin tags in DM (60%). It was found that 8.3% of study sample were suffering of hyperlipidaemia (5patients), in addition to 31 patients (51.7%) known to be hyperlipidaemics and taking antilipidemic medications with total percentage of (60%) positive results, while 34 patients (56.7%) had a history of hypertension (HT), history of cardiovascular diseases (CVD) was positive in 10 patients represented (16.7%). In the vast majority, 39 patients represented (65%), ST were small in size, in 49 patients (81.7%) they were pedunculated, while 38 patients (63.3%) have hyperpigmented ST. Conclusion: Skin tags with DM2 were found to be hyperlipidaemia in 60% of cases while in control it was found to be 50% associated with hyperlipideamia.
Keywords:
Skin Tags, Diabetes mellitus, Sudan
Cite this paper: Nisreen A. O. Mustafa, Abdel Rahaman M. A. Ramadan, Khalid O. Alfarouk, Ahmed Aljarbou, Gamal O. Elhassan, Abdel Khalig Muddathir, Intisar A. Bashir, Anas E. Halloul, Adil H. H. Bashir, Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center, American Journal of Dermatology and Venereology, Vol. 6 No. 3, 2017, pp. 41-50. doi: 10.5923/j.ajdv.20170603.01.
1. Introduction
Diabetes Mellitus (DM):Diabetes mellitus (DM) is metabolic disorder characterized by elevated fasting and postprandial blood glucose level and a variety of multisystem complications, mainly in the blood vessels, eye, kidney, nervous system and integument [1, 3]. Four main types can be distinguished:Type 1, is also known as insulin- dependent DM, or juvenile– onset diabetes (JOD).Type 2, is non-insulin-dependent DM, or adult onset diabetes (AOD).Type 3, secondary diabetes (SD) is an additional type of diabetes [1, 3].Type 4, is gestational diabetes (GD).Skin tag: Skin tags are common, benign lesions composed of loose fibrous tissue and occurring mainly on the neck and major flexures as small, soft, pedunculated protrusions. [6]Skin tags are known to be more common after the age of 40years [7]. These lesions are widespread women at the menopause or later.The lesions are pedunculated and may have a long stalk. They vary in size, about 2 mm in diameter on average. They are rounding, soft and inelastic. The color may be unchanged, but they are frequently hyper-pigmented. The protruding mass is connected to the skin by a narrow pedicle. The bulk of the lesion is loose fibrous tissue, similar to that of the papillary dermis. The epidermis is thin, and the basal cell layer is flat and often hyperpigmented. The most common site is on the sides of the neck, where they may be mixed with typical small, sessile, seborrhoeic keratosis. [6]When more profuse, they can extend on to the face or down to the back and chest. Similar lesions may be found in and around the axillae and groins, often associated with obesity, insulin resistance, and atherosclerosis. [7]Skin tags are thought to be relatively common skin lesions, and it has been reported that they might reflect insulin resistance states, that means the relatively higher lipid profile is associated with features of the insulin resistance. [8]We may state that the atherogenic profile is associated with diabetes mellitus, particularly the type 2 form, but not exclusively. This lipid profile is thought to be strongly associated with atherosclerosis and cardiovascular disease. [8]
2. Rationale
Skin tags may be a major skin marker, a physical sign that should alert the clinician to look for possible impaired glucose tolerance or diabetes mellitus in patients who manifest them. Also, the presence of the atherogenic lipid profile should also be looked for in these individuals. Clinical signs can aid these lection of patients for healthcare screening, and skin tags may be an indicator of higher cardiovascular risk that could be useful in general practices.
3. Objectives
General:To determine atherogenic lipid profile in diabetics type 2 patients with skin tags.Specific:1. To determine the clinical presentation of skin tags in diabetic patients with type 2 DM.2. To detect the prevalence of skin tags among skin manifestations of type 2 Diabetes Mellitus.3. To correlate the relationship between Skin Tags, DM2 and atherogenic lipid profile.
4. Patients and Methods
Study design:Cross sectional, observational, descriptive and prospective hospital based study were conducted.Study area:Jabir Abu Eliz Diabetes center in Khartoum and Khartoum Dermatology and Venereal diseases Hospital were considered.Study population: Include some population in that center with type 2 DM.Control population.Inclusion criteria: 1. Diabetic patients presented with skin tags with known or unknown atherogenic-history.2. Sudanese patients. 3. Type 2 DM.Exclusion criteria: 1. Type 1 DM 2. Non Sudanese.Sample size: A sample size of 60 diabetic patients with skin tags and 20 none diabetic patients with skin tags as a control.Sample type:Systemic samplingSample procedure: data collection: interview and clinical examination.Data collection:Data were collected using specifically designed questionnaire which includes: personal data, dermographic data; age, sex, occupation, tribes, duration of DM, treatment for DM, evolution of skin tags time, history of hyperlipidemia, drugs for hyperlipidemia, history of cardiovascular disease, history of hypertension, number, site, size, type, and color of ST. Associated symptoms like itching and pain.Another questionnaire was made for control sample differ only in asking about the history of DM instead of the question duration and treatment of DM.Medical ethics used:In a gentle and respectful ways, we assured all patients that all their obtained information would be treated in a confidential atmosphere and it will not affect their lives after taking verbal or written consent.Laboratory procedure: Lipid profile including Serum Triglyceride & Serum Cholesterol.Interpretation of results:Positive results: S. Cholesterol > 200mg/dl.S. TG > 150mg/dl.History results of hyperlipidemia and antilipidemic.Negative results: S. Cholesterol < 200mg/dl.S. TG< 150mg/dl.Statistical analysis:Statistical analysis was performed using statistical package for social science (SPSS). A descriptive analysis was done for all questionnaire parameters.
5. Results
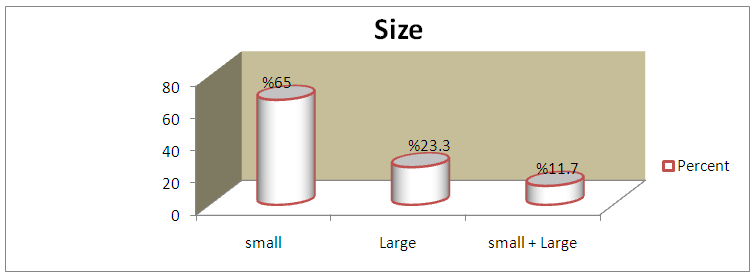
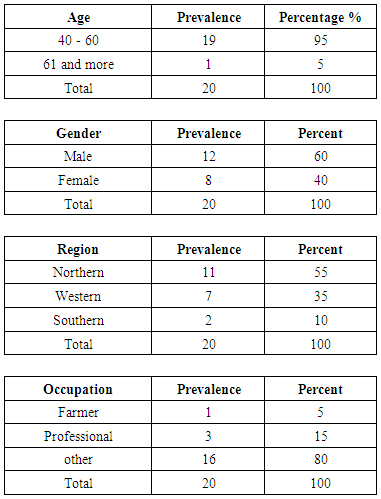
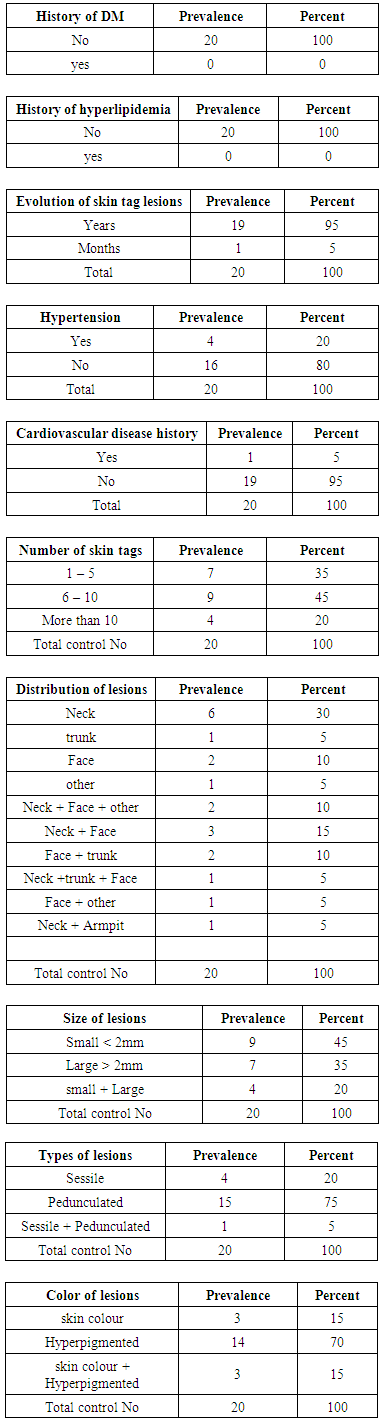
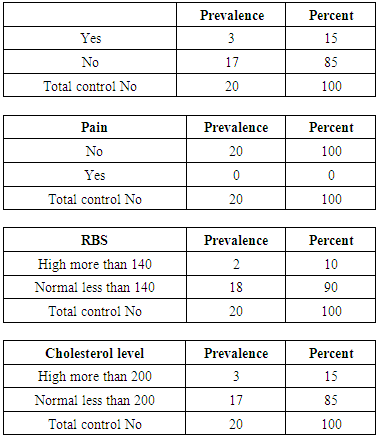
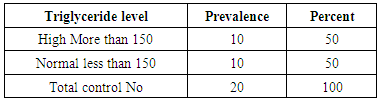
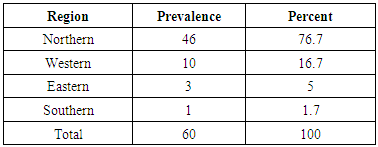
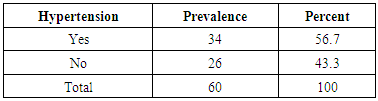
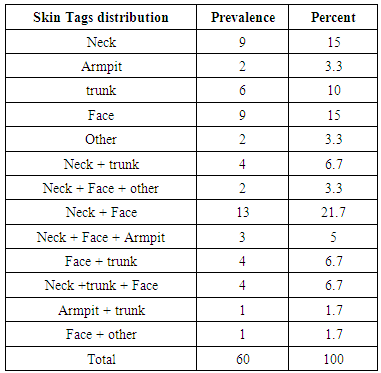
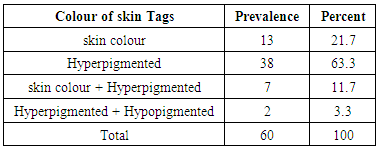
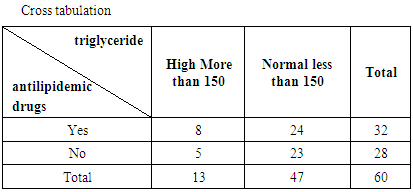
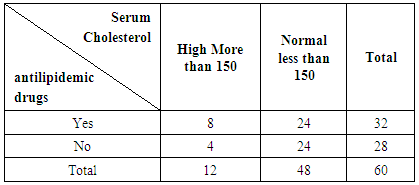
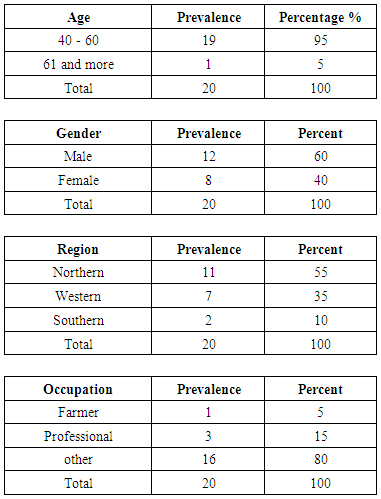
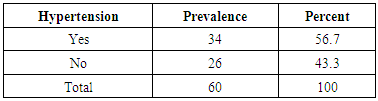
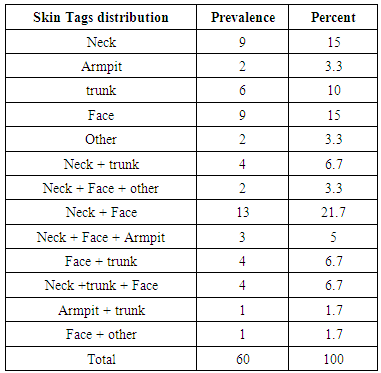
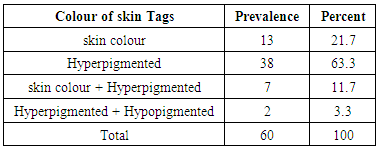
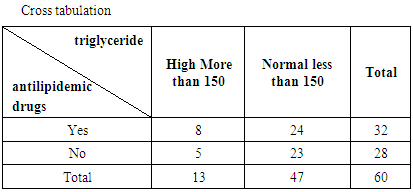
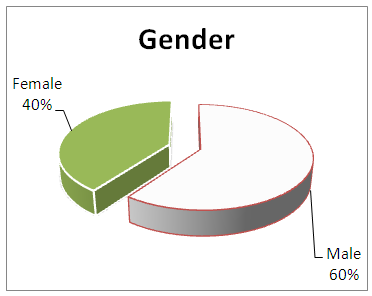
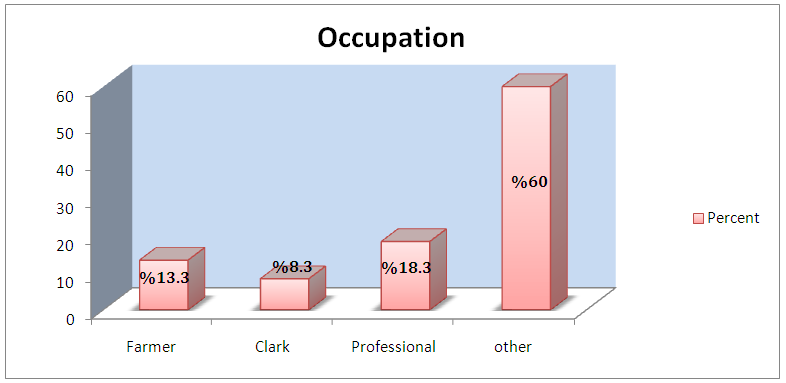
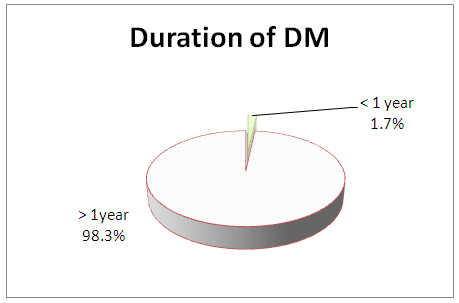
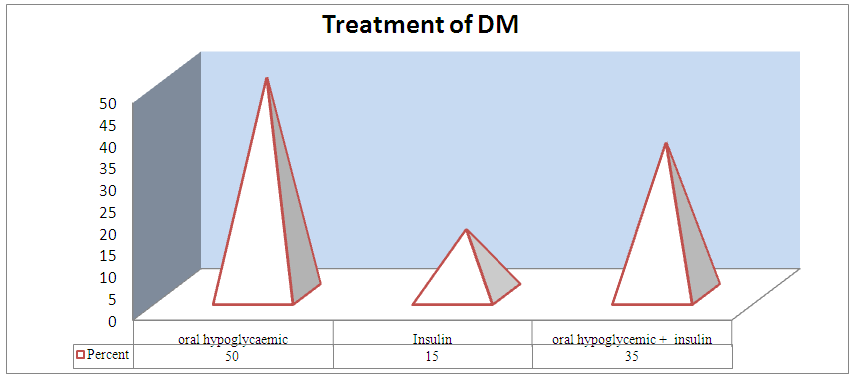
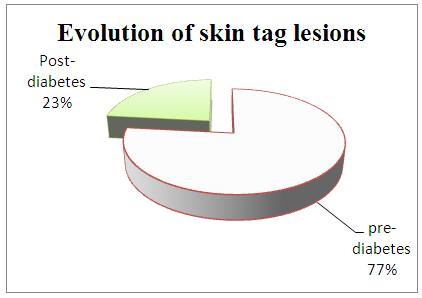
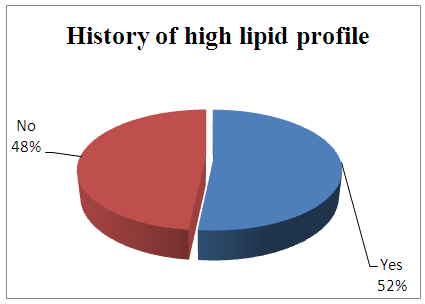
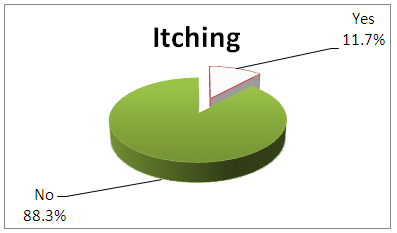
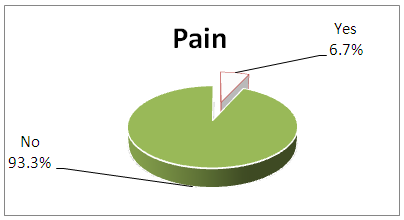
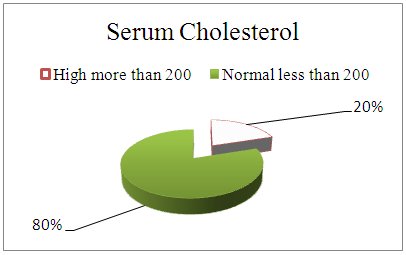
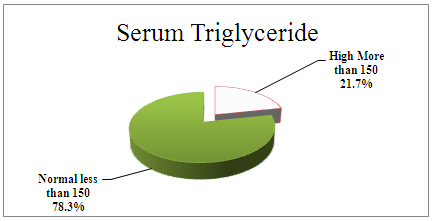
This study included 60 patients with type 2DM and skin tags, out of them 32 of the age group >60 years (53%) and 28 of the age group 40-60 (47%) as showed in (Figure 1).Most of them were male patients represented 36 patients (60%) and the rest, 24 (40%) were female patients (Figure 2). Forty-six patients were from Northern Sudan (76.7%), 10 patients from Western Sudan (16.7%), three from Eastern Sudan (5%) and only one from Southern Sudan 1.7% (Table 1).Regarding occupation among the study group, the majority was of uncertain jobs (free jobs) representing 36 (60%), whereas professional worker presented 11 patients represented (18.3%), farmers were 8 patients (13, 3%) while Clarks were only 5 (8.3%) among them (Figure 3).Concerning the duration of DM, 59 patients (98.3) were diagnosed as diabetic before years, and only one was diagnosed before months 1.7% (Figure 4).Regarding Treatment of DM, 30 patients were taking oral hypoglycemic drugs (50%) and 21 patients represented (35%) having a combination of hypoglycemic and insulin, whereas only 9 (15%) were taking insulin only (Figure 5).The evolution of S T in pre-diabetes was 46 patients (76.7%), and in the post, diabetes discovery was 14 patients 23.3% (figure 6).In 31 patients represented (51.7%), there was a positive history of high lipid profile, while 29 patients (48.3%) has no history of high lipid profile (Figure 7).Thirty-two patients represented (53.3%) were taking antilipidemic drugs, while the rest 28 patients (46.7%) were not.Regarding hypertension (HT) among the study sample, 34 patients (56.7%) had a history of HT, whereas 26 patients represented (43.3%) had no history of HT (Table 2). The history of cardiovascular diseases (CVD) was positive in 10 patients represented (16.7%), and 50 patients represented (83.3%) have negative history to CVD (Figure 9).Twenty-seven patients represented (45%) have ST number between 1-5. Eleven patients represented (18.3%) had a range of 6-10 ST, whereas 22 patients (36.7%) had some more than 10 ST (Figure 10).Distribution of lesions was mostly on more than one site, in 9 patients represented (15%) it was on the neck, 2 patients (3.3%) on armpit, 6 patients (10%) on the trunk, 9 patients (15%) on the face, 2 patients (3.3%) on other parts of the body, 4 patients (6.7%) had ST both on neck and trunk, 13 patients (21.7%) had it on face and neck, 3 patients (5%) has ST on neck, face and armpit,4 patients (4.7%) had ST on neck face and trunk, 2 patients (3.3%) on neck, face and other areas. One patient (1.7%) had ST on both armpit and trunk, and one patient (1.7%) also had ST on both face and thigh (Table 3).In the vast majority, 39 patients represented (65%) ST were small in size, 14 patients (23.3%) they were large and 7 patients (11.7%) had both large and small sized ST (Figure 11).Regarding the type of ST, in 49 patients represented (81.7%), they were pedunculated, 8 patients (13.3%) were the sessile type of ST and 3 patients 5% both types (Figure 12).Concerning the color of ST, 38 patients represented (63.3%) were hyperpigmented ST, 13 patients represented (21.7%) had skin colored ST, while in 7 patients (11.7%) were both skin colored and hyper-pigmented and 2 patients (3.3%) had both hypo and hyperpigmented ST (Table 3).The itching was negative in 53 patients represented (88.3%) and positive in 7 patients (11.7%)-(Figure 13), while the pain was negative in 56 patients (93.3%) and positive in only four patients 6.7% (Figure 14).Cholesterol level was high in 12 patients represented (20%) and was normal in 48 patients (80%) regardless antilipidemics (Figure 15).Triglyceride level was high in 13 patients represented (21.7%) and normal in 47 patients (78.3%) regardless antilipidemics (figure 16).Table 4: Showed relationship between antilipidemic drugs and serum triglyceride (TG) Level from which we can calculate those patients already taking antilipidemic drugs (32 patients), adding to the number of patients who were not taking antilipidemic but have high TG level (5 patients), with a total of 37 patients with positive results of the study (61.6%).Table 5: Showed relationship between antilipidemic drugs & serum cholesterol level from which we can calculate those patients already taking antilipidemic drugs (32 patients), adding to the number of patients who are not taking antilipidemic but have high cholesterol level (4 patients), with a total of 36 patients with positive results of the study (60%).Regarding Control group results, 2 patients represented (10%) found to have high RBS, while the rest 18 patients (90%) had normal RBS. Cholesterol level in control group was normal in 17 patients represented (85%) and high in 3 patients (15%), while TG level was high in 10 patients (50%) and normal in the other 10 Patients (50%).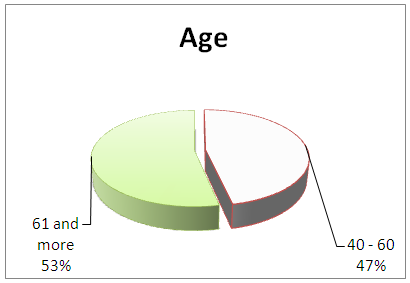 | Figure 1. Showed Age Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
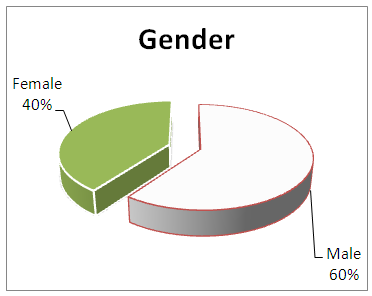 | Figure 2. Showed Gender Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
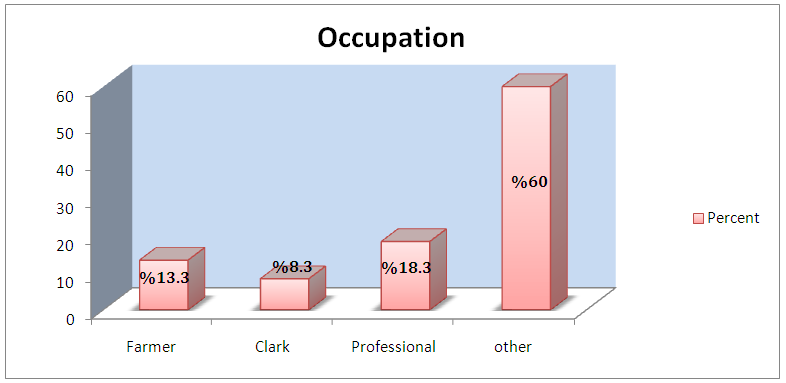 | Figure 3. Showed Occupation Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
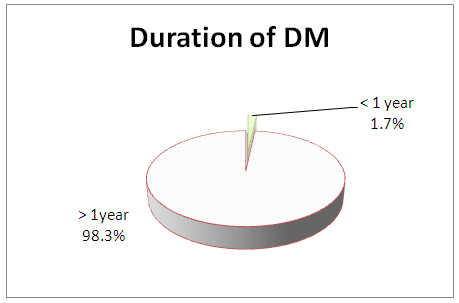 | Figure 4. Showed Duration of DM Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
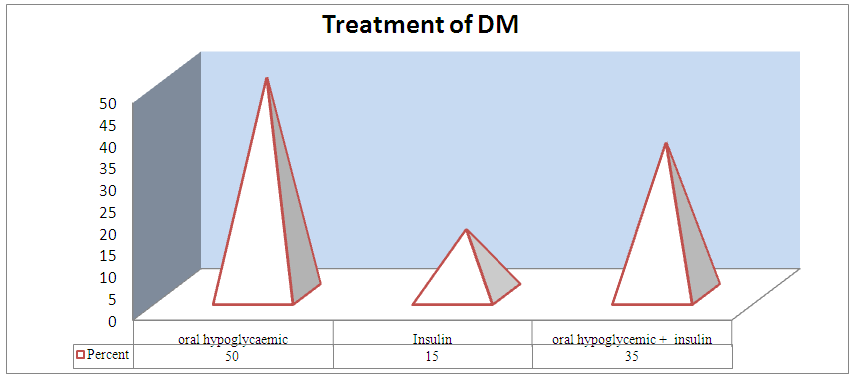 | Figure 5. Showed Treatment of DM Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
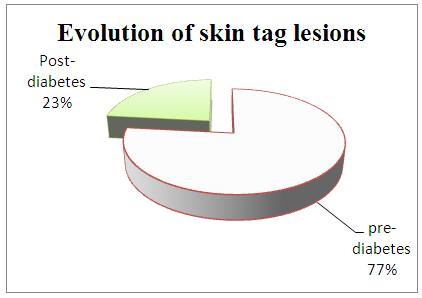 | Figure 6. Showed Evolution of skin tag lesions Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
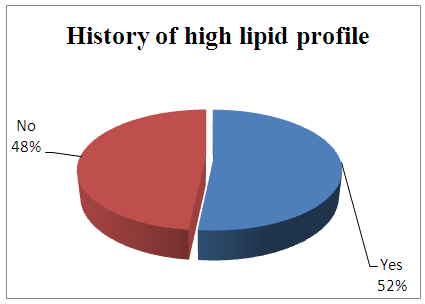 | Figure 7. Showed History of High Lipid Profile Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
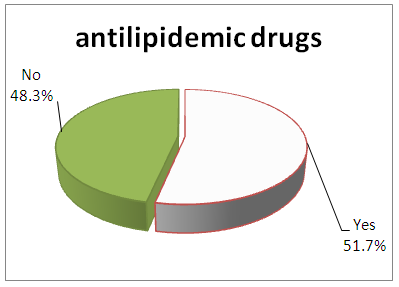 | Figure 8. Showed Antilipidemic Drugs Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015 |
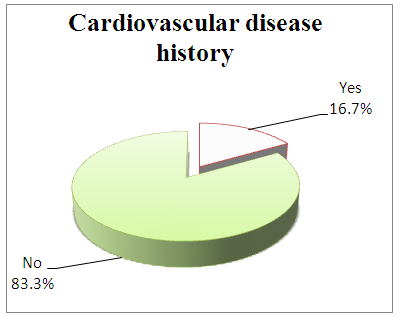 | Figure 9. Showed Cardiovascular Disease History Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
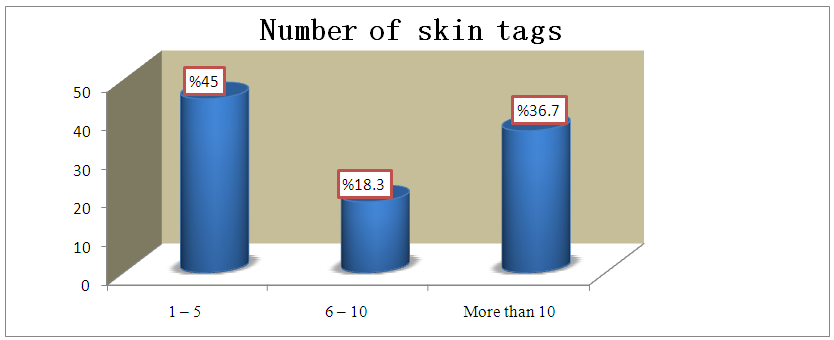 | Figure 10. Showed Number of Skin Tags Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
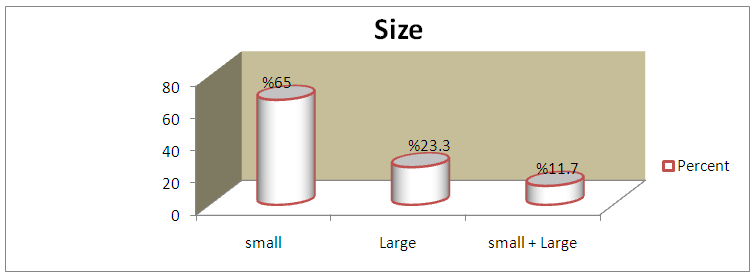 | Figure 11. Showed Size Of Skin Tags Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 (* small < 2mm, large > 2mm) |
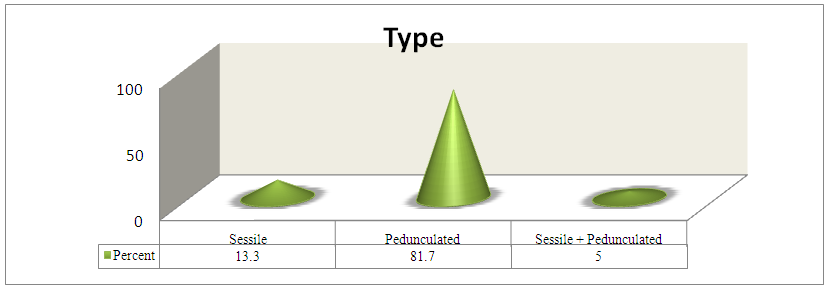 | Figure 12. Showed Type of Skin Tags Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
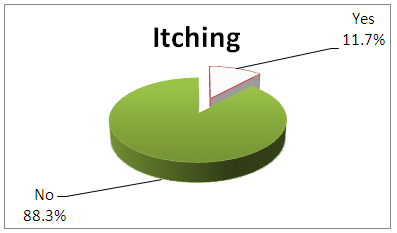 | Figure 13. Showed Presence of Itching Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
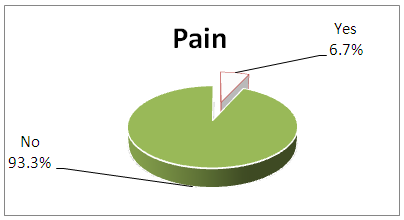 | Figure 14. Showed Presence of Pain Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015 |
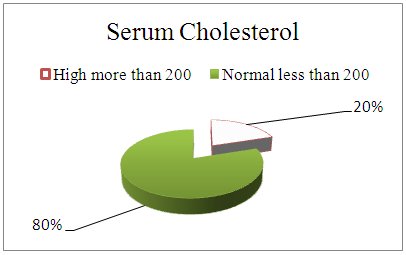 | Figure 15. Showed Serum Cholesterol Level Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 In Jabir Abu Eliz Diabetes Center between August – November 2015 |
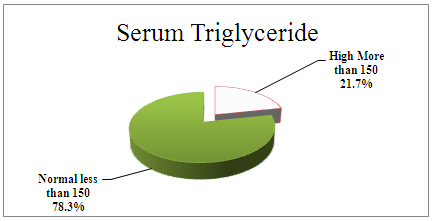 | Figure 16. Showed Serum Triglyceride Level Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 In Jabir Abu Eliz Diabetes Center between August – November 2015 |
Tables of control samples results:Age
 |
| |
|
History of DM
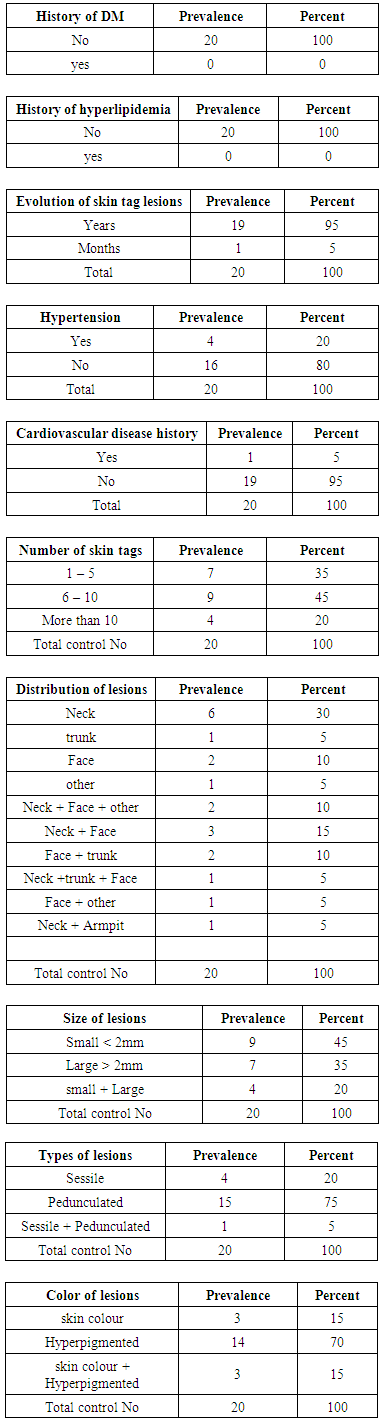 |
| |
|
Itching
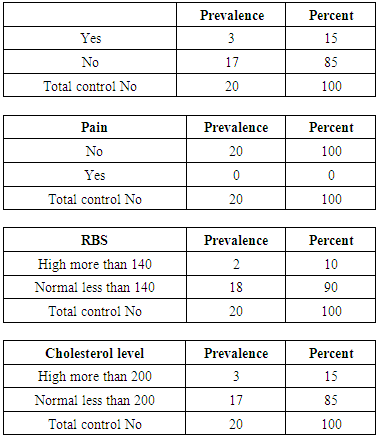 |
| |
|
Triglyceride
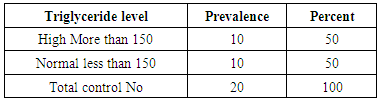 |
| |
|
Table 1. Showed Region Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir Abu Eliz Diabetes Center between August – November 2015
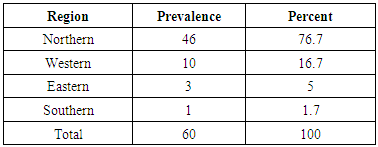 |
| |
|
Table 2. Showed Hypertension History Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015
 |
| |
|
Table 3. Showed Skin Tags Distribution - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015
 |
| |
|
Table 4. Showed Colour of Skin Tags - Skin Tags And Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015
 |
| |
|
Table 5. Showed Relationship between antilipidemic drugs and Serum Triglyceride Level - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015
 |
| |
|
Table 6. Showed Relationship between antilipidemic drugs and Serum Cholesterol Level - Skin Tags and Atherogenic Lipid Profile in Diabetes Mellitus Type 2 in Jabir AbuEliz Diabetes Center between August – November 2015
 |
| |
|
6. Discussion
In the literature, limited studies had been found to be done in the correlation between skin tags and atherogenic lipid profile and diabetes mellitus type 2.This study included 60 patients with ST; all were known to be DM type 2 and were tested for lipid profile including cholesterol and TG.The prevalence of ST among type 2 DM in Jabir Abu Eliz center was 60 patients out of 640, which represented 9.4%.Bashir et al. in Khartoum study of 1112 cases of diabetes mellitus examined for cutaneous manifestations, only 125 diabetic patients (11.24%) showed cutaneous lesions. The prevalence of Skin Tag (ST) was reported to be 2.4%. All participants were typed 2 DM. [28]In this study the lipid profile was significantly high in diabetic patients with ST (60%) a relatively similar study in Egypt, where 50 persons were included in this study, they were divided into 2 groups, the first group included 30 patients (each with 3 or more skin tags) and the second group which represented 20 individuals, age sex matched and apparently healthy volunteers with no skin tags as contro. The highly significant difference was found of the fasting blood glucose, HbAIc, serum cholesterol, LDL, and VLDL between patients and controls while serum TG and HDL were higher in patients than controls but did not reach the statistical significance. As regards the serum leptin level we found a highly significant difference between patients and control. [29]Also, a cross sectional studies in Brazil showed those patients with > 5 skin tags in the neck region and/or axillae. Results were adjusted for the other known co-varieties of risk for insulin resistance using a multiple logistic regression models. They had ninety-eight cases, and 103 controls were evaluated. There was no difference between the groups concerning age or gender. Skin tags were directly associated with HOMA-IR values (odds ratio = 1.4), hypertriglyceridemia and body mass index, irrespective of adjustment for diabetes mellitus, age, skin Phototype, gender, family history of diabetes mellitus or hip/waist ratio. Qualitatively elevated HOMA-IR levels (>3.8) were also significantly associated.An other dual study in India done for comparison Kahana et al., screened 216 patients with skin tags and found overt DM in 26.3% [57] of the patients and impaired glucose tolerance test was found in 7.9% and similarly Thappaetal. [22], found that 62.8% of the patients with skin tags had diabetes, and thus both the studies concluded that skin tags may serve as markers for diabete smellitus. [31]Another study in India, Bhargava et al. reported skin tags in 20% patients of overt DM, whereas impaired GTT was found in 8% of patients. Achrochordon is regarded as a sign of impaired glucose tolerance, DM, and increased cardiovascular (atherogenic lipid profile) risk. [3]
7. Conclusions
Skin tags associated with high lipid profile in DM type 2, In 31 patients represented (51.7%) there was a positive history of high lipid profile, while 29 patients (48.3%) has no history of high lipid profile, 59 patients (%) out of those with negative history found to be had high lipid profile, with a total of 36 patients, raising the percentage up to (60%). Skin tags were considered to be an indicator for high lipid profile in type 2 DM.
8. Recommendations
This study suggests that Skin Tags may be considered as a clinical marker for high lipid profile in diabetes type 2 and an indicator for cardiovascular risk.The study aimed to encourage further researchers for proving the correlation between ST and atherogenic lipid profile in a larger study sample scale.This study could help general practitioners and specialists to evaluate cardiovascular risk from atherogenicity for patients presented with skin tags in referral clinics.Screening lipid profile may be necessary for diabetic type 2 patients, whom having skin tags attending to Dermatology Hospital even for other complaint and refer them to Internal Medicine department to evaluate cardiovascular risks.
References
| [1] | National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes, 1979; 28: 1039-57. |
| [2] | Perez M I, Kohn SR. Cutaneous manifestations of diabetes mellitus. Journal of American Academy of Dermatology; 1994, 30:519-31. |
| [3] | Oyer DS. Diabetes mellitus: new developments. Arch. Dermatol. 1982:118:132-4. |
| [4] | Diabetes Statistics-MSN Home/Hotmail-For the latest MSNBC Health. Internet. |
| [5] | Sonck CE, Somersalo O: The yeast flora of the anogenital region in diabetic girls. Arch. Dermatology.196388:846-852. |
| [6] | Rook text book of dermatology, 8th edition 2010, p 52.40. |
| [7] | Fitzpatrick’s dermatology in general medicine, 7th edition 2008, p 554. |
| [8] | Crook MA, Skin tags and the atherogenic lipid profile, JClinPathol. 2000 Nov; 53(11): 873-4. |
| [9] | Rook's text book of dermatology, eighth edition 2010, p 52.40-1. |
| [10] | Jean L Bolognia MD, Joseph L Jorizzo MD. Third edition Dermatology. Vol. 1. 2012, p 1961. |
| [11] | Rook's text book of dermatology, eighth edition 2010, 62.58. |
| [12] | Rook's text book of dermatology, eighth edition 2010, 8.13. |
| [13] | Fitzpatrick’s dermatology in general medicine, 7th edition 2008, p 1327. |
| [14] | Adams BB, Mutasim DF. Elastic tissue in fibroepithelial polyps. American Journal of Dermatopathology. 1999 Oct. 21(5):446-8. |
| [15] | Kassinove A, Raam R. Acrochordon of the labia. J Emerg Med. 2013 May. 44(5):e361-2. |
| [16] | Gorpelioglu C, Erdal E, Ardicoglu Y, Adam B, Sarifakioglu E. Serum leptin, atherogenic lipids and glucose levels in patients with skin tags. Indian Journal of Dermatology. 2009. 54:20-22. |
| [17] | Boza JC, Trindade EN, Peruzzo J, Sachett L, Rech L, Cestari TF. Skin manifestations of obesity: a comparative study. Journal of European Academy of Dermatology and Venereology. 2011 Sep 20, 1220-3. |
| [18] | Akpnar F, Dervs E. Association between Acrochordons and the components of metabolic syndrome. European Journal of Dermatology. 2011 Nov 7. (1): 106-10. |
| [19] | Senel E, Salmanoglu M, Solmazgül E, BerçikInal B. Acrochordons as a cutaneous sign of impaired carbohydrate metabolism, hyperlipidemia, liver enzyme abnormalities and hypertension: a case-control study. Journal of European Academy of Dermatology and Venereology. 2011 Dec 21.10.1111. |
| [20] | Garg S, Baveja S. Giant Acrochordon of Labia Majora: An Uncommon Manifestation of a Common Disease. Journal of Cutaneous Aesthetic Surgery. 2015 Apr-Jun. 8 (2): 119-20. |
| [21] | Dianzani C, Calvieri S, Pierangeli A, Imperi M, Bucci M, Degener AM. The detection of human papillomavirus DNA in skin tags. Brazilian Journal of Dermatology. 1998 Apr. 138(4): 649-51. |
| [22] | Thappa DM. Skin tags as markers of diabetes mellitus: an epidemiological study in India. Indian Journal of Dermatology. 1995 Oct. 22(10):729-31. |
| [23] | Goyal A, Raina S, Kaushal SS, Mahajan V, Sharma NL. Pattern of cutaneous manifestations in diabetes mellitus. Indian Journal of Dermatology. 2010. 55(1):39-41. |
| [24] | Mathur SK, Bhargava P. Insulin resistance and skin tags. Dermatology. 1997. 195(2):184. |
| [25] | Görgülü T, Torun M, Güler R, Olgun A, Kargi E. Fast and Painless Skin Tag Excision with Ethyl Chloride. Aesthetic Plastic Surgery. 2015 Aug. 39 (4):644-5. |
| [26] | Monfrecola G, Riccio G, Viola L, Procaccini EM.A simple cryo-technique for the treatment of cutaneous soft fibromas. Journal of Dermatologic Surgery and Oncology. 1994 Feb. 20(2): 151-2. |
| [27] | Eley KA, Pleat JM, Wall SA. Reconstruction of a congenital nasal deformity using skin tags as a chondro-cutaneous composite graft. Journal of Craniofacial Surgery.2009 Mar. 20(2): 573-5. |
| [28] | Bashir, A.H.H. (2004). Clinico-epidemiological Study of Cutaneous Manifestations of Diabetes mellitus in Jabir Abu Eliz Diabetic Center in Khartoum, Sudan. Sudanese Journal of Dermatology. September 2004; 2(2):34-38. |
| [29] | Zeinab Tosson; Samia A. Ibrahim; Abdalla H. Kandil and Mohamed Husam, Relationship between skin tags, leptin hormone and metabolic disturbances. Egyptian Dermatology Online Journal; 9 (2): 4, December 2013. |
| [30] | Andréia de Almeida TamegaI; Adriana Milanezi Pinheiro AranhaII; Marcelo Massaki GuiotokuIII; Luciane Donida BartoliMiotIV; HélioAmanteMiotV. Association between skin tags and insulin resistance. Anais Brasileiros de Dermatologia. vol.85 no.1 Rio de Janeiro Jan./Feb. 2010. |
| [31] | Dependra Kumar Timshina, Devinder Mohan Thappa, Aparna Agrawal, A clinical study of dermatoses in diabetes to establish its markers. Indian Journal of Dermatology 2012, Volume: 57: 1, 20-25. |
| [32] | Roshni Vahora, Sejal Thakkar, Yogesh Marfatia, Skin a mirror reflecting diabetes mellitus: A longitudinal study in a tertiary care hospital in Gujarat. Indian Journal of Dermatology Year: 2013, Volume: 17: 4, 659-664. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML