-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2017; 6(2): 17-24
doi:10.5923/j.ajdv.20170602.01

The Efficacy of Topical Hyaluronic Acid Serum in Acne Scar Patients Treated with Fractional CO2 Laser
Shakir J. Alsaedy, Khansaa A. Mosa, Salah H. Alshami
Department of Dermatology, Alkindy Teaching Hospital, Baghdad, Iraq
Correspondence to: Khansaa A. Mosa, Salah H. Alshami, Department of Dermatology, Alkindy Teaching Hospital, Baghdad, Iraq.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Acne is a common disorder experienced by up to 80% of peoplebetween 11 and 30 years of age and by up to 5% of older adults. It is caused by several factors including increased sebum production, follicular hypercornification, colonization with Propionibacterium acnes, and a lymphocytic and neutrophilic inflammatory response. Acne scarring can be divided into 2 main categories: Atrophic and Hypertrophic scars, the atrophic scars are subdivided into 3 basic types: icepick scars, rolling scars, and boxcar scars. Fractionated carbon dioxide (CO2) laser resurfacing combines the concept of fractional photothermolysis with an ablative 10600-nm wavelength. This technology allows for the effective treatment of acne scars, reduced recovery periods and a significantly minimal side effect profile as compared to traditional CO2 laser resurfacing. Hyaluronic acid is a carbohydrate occurring naturally in all living organisms. The biological functions include maintenance of the visco-elastisity of liquid connective tissues such as joint synovial and eye vitreous fluid, control of tissue hydration and water transport. This study is designed to evaluate the efficacy of using topical hyaluronic acid serum in patients with atrophic acne scars after treatment with fractional CO2 laser. Patients and Method: Thirty six patients (26 females and 10 males) withmoderate to severe atrophic acne scarring were included in this. The patients were divided randomly into two equal groups; one group was treated with CO2 fractional ablative laser alone and the other group was treated with laser in addition to topical hyaluronic acid serum to compare the final results between the two groups and assess the effect of hyaluronic acid on wound healing and post-operative complications. Therapeutic outcomes were assessed by standardized digital photography. Results: The final results after 3 months according to dermatologists' assessmentof level of improvement in response to treatment by CO2 laser combined with topical hyaluronic acid were as follows: three patients (16.6%) reported excellent improvement, nine patients (50%) significant improvement, five patients (27.7%) moderate improvement and one patient (5.5%) showed mild improvement in the appearance of the acne scars. The results were significant as indicated by the P value which was 0.002. All participants reported mild side effects like pain, erythema and peeling and few patients suffered from edema and severe peeling but they were all tolerable and transient and last for approximately five days. Conclusion: The addition of hyaluronic acid to CO2 laser resurfacing does notonly enhance the effect of laser but also provides faster recovery time and fewer side effects when compared to the CO2 laser resurfacing alone.
Keywords: Hyaluronic acid, Acne scars, Fractional CO2 laser
Cite this paper: Shakir J. Alsaedy, Khansaa A. Mosa, Salah H. Alshami, The Efficacy of Topical Hyaluronic Acid Serum in Acne Scar Patients Treated with Fractional CO2 Laser, American Journal of Dermatology and Venereology, Vol. 6 No. 2, 2017, pp. 17-24. doi: 10.5923/j.ajdv.20170602.01.
1. Introduction
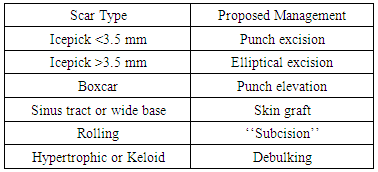
- Acne is a chronic inflammatory disease of pilosebaceous follicles, characterized by comedones, papules, pustules, nodules & often scars. It is caused by several factors including increased sebum production, follicular hypercornification, colonization with Propionibacterium acnes, and a lymphocytic and neutrophilic inflammatory response [1, 2]. Collagen and other tissue damage from the inflammation of acne leads to permanent skin texture changes and fibrosis. Dermal damage is more long lasting and results in an increase or decrease of tissue and often worsens in appearance with age as a result of normal skin changes. The two main causes of acne scar formation can be broadly categorized as either a result of increased fibrous tissue formation or, the more common cause, loss or damage of tissue [3]. Treatment of the true scars resulting from acne must reflect several considerations by the physician. Cost of treatment, severity of lesions, physician goals, patient expectations, side-effect profiles, psychological or emotional effect to the patient, and prevention measures should all play a role [4]. There are numerous surgical options available for treatment of acne scars (Table 1).
|
2. Patients and Methods
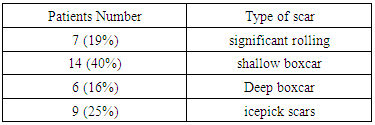
- This is an open therapeutic trial study performed at Beirut Private Center for Laser Treatments in Baghdad, Iraq during the period from April, 1st 2015 to April, 1st 2016. Thirty six patients (26 females and 10 males) with moderate to severe atrophic acne scarring according to Goodman's qualitative global acne scarring grading system (table 8) were included in this study. Their ages ranged from 20 to 43 years (mean age: 29.69 years old SD±7.21) and their Fitzpatrick skin types were III-IV. This study approved by the ethical committee in Al-Kindy teaching hospital. Written informed consent was obtained from each patient.Exclusion criteria include known photosensitivity, pregnancy or lactation, inflammatory skin disorders or active herpes infection, history of hypertrophic or keloidal scarring, and the use of isotretinoin or other physical acne treatments over the past 6 months. The use of anti-coagulants, isotretinoin, patients who had any medical illness (e.g. diabetes, chronic infections, blood dyscrasias) that could influence the wound healing process were also excluded. Patients were allowed to continue previous acne medications during the study except isotretinoin.All patients had mixed types of atrophic acne scars, including ice pick, boxcar, and rolling scars, although, some particular type predominates and therefore is used to classify the patients accordingly (Table 2).
|
3. Results
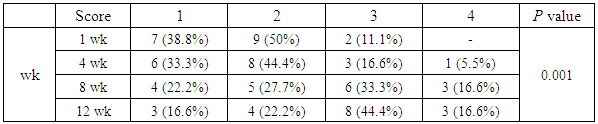
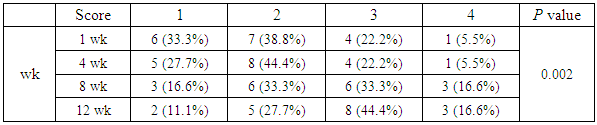
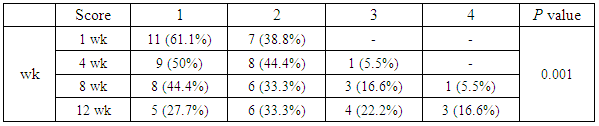
- Thirty six patients (26 females and 10 males) were included in the study. All patients completed the study, including the 3- month follow-up period. Most patients had mixed types of atrophic acne scars, including ice pick, boxcar, and rolling scars.The patients were divided equally into two groups (18 patients in each group). First group was treated with CO2 fractional ablative laser alone and the second group was treated with laser in addition to topical hyaluronic acid serum.In the second group, according to the patients' self-assessment of improvement, the results were remarkable and showed a great amount of satisfaction (Table 3). The results after 3 months follow-up were as the following: three patients (16.6%) reported excellent improvement, eight patients (44.4%) significant improvement, four patients (22.2%) moderate improvement and three patients (16.6%) mild improvement in the appearance of the acne scars. The results considered significant as indicated by the P value which was 0.001.
|
|
|
|
|
|
 | Figure 1. Patient 1: Pre- and 3 months post operatively |
 | Figure 2. Patient 2: Pre- and 3 months post operatively |
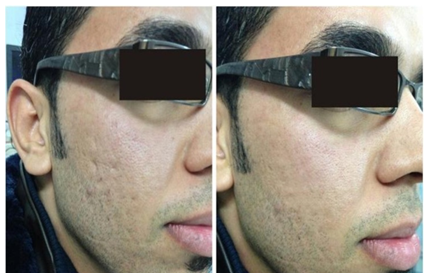 | Figure 3. Patient 3: Pre- and 3 months post operatively |
 | Figure 4. Patient 4: Pre- and 3 months post operatively |
4. Discussion
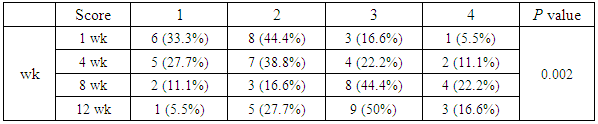
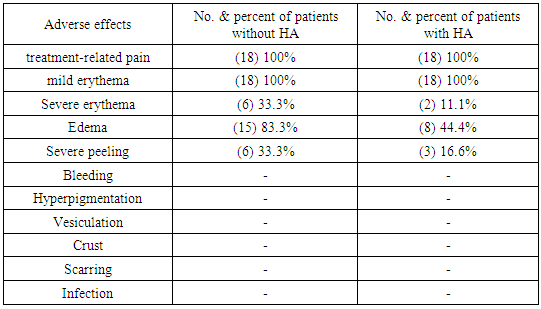
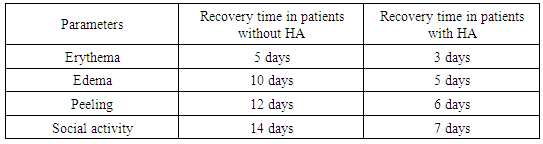
- Hyaluronan is a synthesized polysaccharide polymer composed of chains of the monosaccharide glucuronic acid and N-acetylglucosamine-1. A large variety of cells are able to produce hyaluronan; however, the most important, in terms of the wound healing response, appears to be keratinocytes, fibroblasts and platelets [21]. The skin normally contains the highest concentration of hyaluronan within the body [22]; however, the levels of free hyaluronan within the blood are low due to its rapid clearance by the liver [23].During tissue trauma or following infection, hyaluronan accumulates and stimulates immune cells at the injury site to express inflammatory mediators [24-26]; higher levels were also found in newly formed granulation tissue [27]. Hyaluronan is a highly hygroscopic (moisture retaining) compound [28]; By maintaining a moist wound environment, hyaluronan protects cells from the effects of desiccation, also assisting in cell movement by helping the dividing cell to disassociate itself from its substratum and providing a hydrated matrix, which facilitates easier cell movement [29]. In addition, it also affects the migration of fibroblasts to the wound site [30] by interaction with hyaluronan receptors (CD44 and RHAMM) through which it activates intracellular signaling pathways [31].Atrophic acne scars occur as a consequence of impaired resolution or wound healing after the damage of sebaceous follicles during active inflammation [32], and are usually classified into ice pick, rolling, and boxcar scars according to shape and depth [33]. Their treatment options include laser skin resurfacing, chemical peeling, dermabrasion/ microdermabrasion, tissue augmentation, and various other modalities.Fractional photothermolysis (FP) is a relatively new technology for skin resurfacing introduced and discussed in 2004 [34]. It depends on generating multiple non-contiguous zones of thermal damage (MTZ) in the epidermis and dermis, sparing the viable tissue surrounding each MTZ. The untreated healthy skin remains intact and actually aids the repair process, promoting rapid healing with only a day or two of downtime [35]. FP stimulates epidermal turnover and dermal collagen remodelling, which leads to significant improvements in a variety of scars [36, 37]. This technology has been used in a wide variety of skin conditions including (but not limited to) photo-aging, periorbital wrinkling, acne scarring, melasma and other pigmented lesions [38].The results of first group was very satisfactory as nearly as 72% of patients showed moderate to significant response according to dermatologists' assessment. These results were comparable to the results of another study investigating the effect of CO2 laser in treating acne scars conducted in Iraq few years earlier [39]. The results are significant as indicated by the P values which was 0.002.The results of the second group were very good as more than 77% of patients showed moderate to significant improvement. However, the patients' self-assessment is lower than that of the dermatologists (66%); this might be attributed to the fact that the patients usually use more subjective than objective scales, and they show a higher level of expectations of end results than the actual outcome. The results of both assessment groups (the patients and the dermatologists) are significant as indicated by the P values which were 0.001 and 0.002 respectively.All patients show different level of improvement ranging from mild to excellent results after only one session of laser treatment. In fact, surprisingly, mild improvement was observed in only one patient according to the dermatologists' assessment, although; according to patients' self-assessment the results were less remarkable (as mentioned above). This gives us a strong indicator of the overall results and the level of improvement noticed by the patients in general.The final outcome of laser treatment is best read after 3-6 months post-operatively. This time is usually needed for new collagen remodelling [40] and it was the same time interval we use to follow up our patients and read their end-results which were significantly different from the results after one week post-operatively.The effect of the addition of topical hyaluronic acid to the patients in combination with laser treatment is very obvious. According to previous studies investigating the effect of fractional ablative CO2 laser on acne scars, 70% of the CO2 laser sites were graded as having moderate to significant improvement of scars [39, 41]. Their end-results, although; were not significantly different from our results after 3 months follow-up (77% showed moderate to significant improvement) but taking in consideration the post-operative pain, edema, erythema and duration of peeling which were less and more tolerable and acceptable than that were associated with CO2 laser treatment alone.In contrast to CO2 laser resurfacing alone, the physiologic changes in wound healing treated with hyaluronan serum will allow the skin to recover faster [42]. Pigment alteration, which is a common side effect of CO2 laser, was not reported with hyaluronan addition in any of our patients even with those who don't commit to strict sunscreen.It was clearly demonstrate that hyaluronic acid offers not only beneficial effects to the skin but also influence the expression of many genes including those contributing to keratinocyte differentiation and formation of intercellular tight junction complexes which are reported to be reduced in aged and photodamaged skin [43]. HA has been shown to promote the migration and maturation of keratinocytes in process of re-epithelialization and it has even been proposed as a possible marker for effective healing in soft tissues [44]. Its activity is manifested in granulation tissue where it is abundantly produced and counters the damage induced by reactive oxygen intermediates [45]. Hyaluronan has an active role in the modification of the inflammatory response. It is thought to moderate the inflammatory response through its specific interactions with constituents of the inflammatory response, stabilizing cytokine activity and reducing protease-induced damage [46].In procedures aiming at aesthetic improvement, patient perception of the treatment outcome appears to be most important because it has a direct impact on patients’ body image and self-esteem [47], which can be obtained superbly by the CO2 laser but when hyaluronic acid topical serum is added, the results are noteworthy, recovery time is considerably shortened and traditional post-resurfacing sequelae are absent. Consequently this allows the patients a rapid return to their social or work environment.In general, the addition of hyaluronic acid to CO2 laser resurfacing does not only enhance the effect of laser but also provides faster recovery time and fewer side effects when compared to the CO2 laser resurfacing alone.
5. Conclusions
- 1. Fractional CO2 photothermolysis can be a safe and effective option for the treatment of acne scars in Iraqi skin. 2. Combination treatment with topical hyaluronic acid serum can constitute a synergistic approach for optimal outcomes. 3. Fractional CO2 photothermolysis plus topical hyaluronic acid serum were associated with substantial improvement in the appearance of all types of acne scars with lesser side effects. 4. Most patients began to show a visible improvement following only one session and according to visual assessments of patients and dermatologists, patients improvement continue to occur even after 3 months of operation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML