-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2015; 4(1): 9-11
doi:10.5923/j.ajdv.20150401.03
Case Report: Testicular Seminoma in Sudanese Patient
Anilkumar Mitani1, Mohamed A. Hameed2, Gamal O. Elhassan3, 4, Khalid O. Alfarouk5, Abdel Khalig Muddathir6, Adil H. H. Bashir6
1University of Bahri, Bahri, Sudan
2Omdurman Islamic University, Omdurman, Sudan
3School of Pharmacy, Uneiazah University, AL-Qassim, KSA
4Faculty of Pharmacy, Omdurman Islamic University, Omdurman, Sudan
5Alfarouk Biomedical Research, LLC, Tampa, Florida, USA
6University of Khartoum, Khartoum, Sudan
Correspondence to: Adil H. H. Bashir, University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
A male, 22 years old young man presented with left testicular mass and pain along left leg and lower back for one year; the mass is totally excised and sends to histopathology to be confirmed as Seminoma.
Keywords: Testicular Seminoma, Sudan
Cite this paper: Anilkumar Mitani, Mohamed A. Hameed, Gamal O. Elhassan, Khalid O. Alfarouk, Abdel Khalig Muddathir, Adil H. H. Bashir, Case Report: Testicular Seminoma in Sudanese Patient, American Journal of Dermatology and Venereology, Vol. 4 No. 1, 2015, pp. 9-11. doi: 10.5923/j.ajdv.20150401.03.
1. Case Report
- A male patient, laborer, 22 years old, single, resident in Al-Gezira, South of Khartoum. The patient was complaining of painfully hard swelling at left testicle one year ago, no increase in testicle size at the first three months, then gradually increased to reach a grapefruit size in almost eight months. Patient’s general condition was good within two years before a sense of hotness in the left testicle on and off. No loss of weight or appetite, as no fever or night sweating. The condition started with sudden onset and progressive course, where received treatment in the form of tablets and capsules with no response. Patient has been admitted to hospital for enteric fever at childhood.Family history: Parents are first-degree relatives, as no similar condition in the family.On examination: Patient has normal facial features and good general condition. Lesions are skin colored and Firm on palpation.Palms &soles: not detected. Nails: No nail dystrophy. Hair: No Abnormality Detected. Eye: No abnormality is seen.Oral mucosa & Lips: No abnormality is seen.Genital Examination: Left testicle is large in size about 12X8 cm, freely mobile, slightly tender, smooth surface with palpable 2 nodules, testicle is hard in consistency, spermatic cord couldn’t be palpated, and noregional inguinal lymph nodes are palpable, as Para aortic lymph nodes.Scrotal skin shows an ulcer 3X4 cm punched out, indurated, with necrotic floor, penis and pubic hair look normal on examination. Right testicle shows no abnormality. No palpable regional or Para aortic lymph nodes.
2. Investigations Did
- Ultra sonography of both testicles:Gross multiple ectopic left testicular mass with left spermatocele.Right testicular size and pattern looks normal.Histopathology: Gross: Hard growth, 13X8 in size, regular, smooth, with ill-defined spermatic cord structure.
3. Discussion
 | Figure 1. Scrotal swelling and necrotic ulcer |
 | Figure 2. Spermatic cord of the swollen testes |
 | Figure 3. Excision of the scrotal ulcer prior to removal of the testicular tumor |
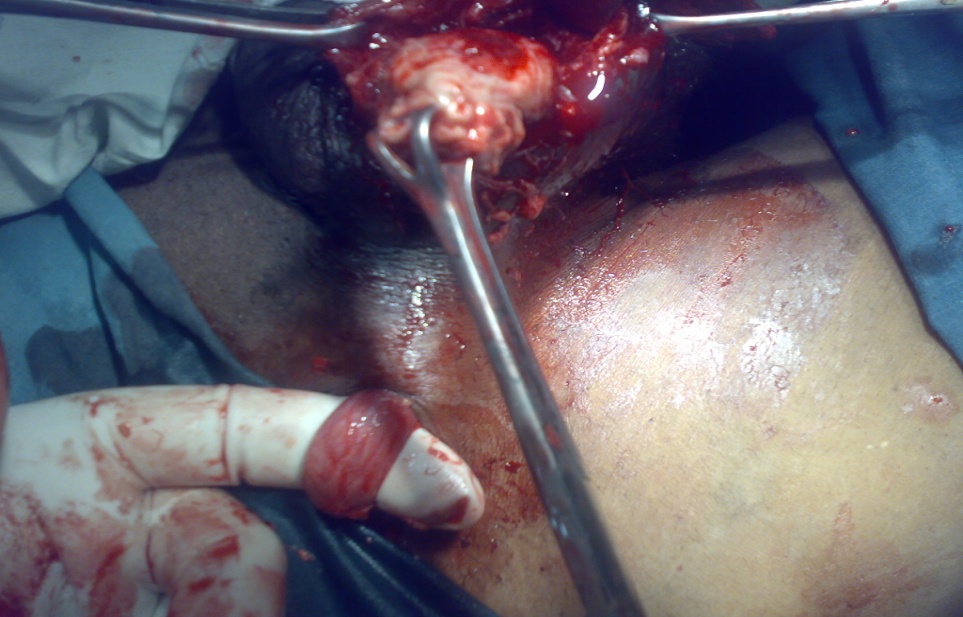 | Figure 4a. Removal of the testicular tumor |
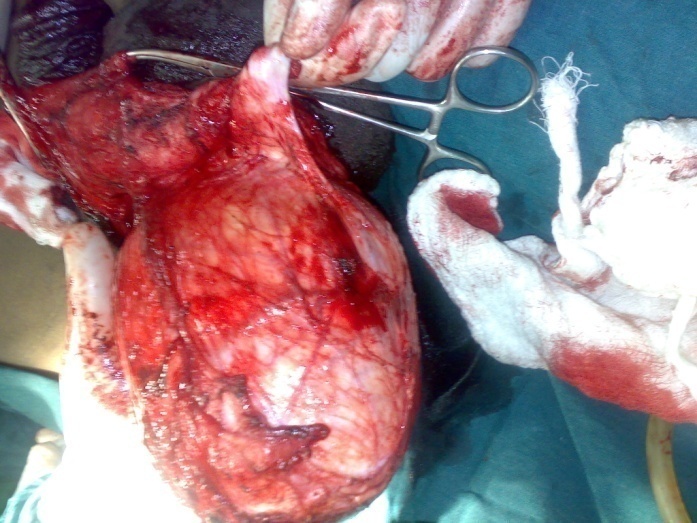 | Figure 4b. Removal of the testicular tumor |
 | Figure 5. the testicular tumor is totally removed |
 | Figure 6. The case after the operation |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML