-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2014; 3(5): 87-94
doi:10.5923/j.ajdv.20140305.03
Treatment of Periorbital Hyperpigmentation Using Platelet-Rich Plasma Injections
Salah Hashim Al-Shami
Dermatologist and Venereologist, Laser Care center, Amman, Jordan
Correspondence to: Salah Hashim Al-Shami, Dermatologist and Venereologist, Laser Care center, Amman, Jordan.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Background: The term Platelet-Rich Plasma (PRP) is a generic term used to describe a plasma suspension obtained from whole blood, prepared so as to contain platelet concentrations higher than those normally found in circulating blood. The mechanism of action of PRP is based on the fact that platelets contain many growth factors. These factors have a well-known role in the process of tissue repair. Periorbital hyperpigmentation refers to conditions that present with relative darkness of the periorbital eyelids. It has multifactorial causes like sun exposure, smoking, alcoholism and sleep deprivation. Various treatments have been proposed for periorbital hyperpigmentation but without clear-cut results. This study, was designed to evaluate the effectiveness of platelet-rich plasma in the treatment of periorbital hyperpigmentation in Jordanian patients. Patients and Methods:This is an open therapeutic trial study performed at Laser Care Clinic in Amman, Jordan during the period from July, 1st 2013 to July, 1st 2014. Fifty patients (46 females and 4 males) with periorbital hyperpigmentation were included in this study. The treatment course consisted of three sessions of autologous platelet-rich plasma injections into the periorbital area as well as the whole face with one month apart in between the injections. Therapeutic outcomes were assessed by standardized digital photography. Results: The final results after 6 months were as follows: two patients (4%) reported excellent improvement, six patients (12%) significant improvement, twenty three patients (46%) moderate improvement, and nineteen patients (38%) mild improvement in the appearance of the dark circles.Conclusions:PRP is a useful treatment for periorbital hyperpigmentation and further comparative studies of other treatment modalities are highly recommended.
Keywords: Platelet-rich plasma, Periorbital hyperpigmentation, Facial rejuvenation
Cite this paper: Salah Hashim Al-Shami, Treatment of Periorbital Hyperpigmentation Using Platelet-Rich Plasma Injections, American Journal of Dermatology and Venereology, Vol. 3 No. 5, 2014, pp. 87-94. doi: 10.5923/j.ajdv.20140305.03.
1. Introduction
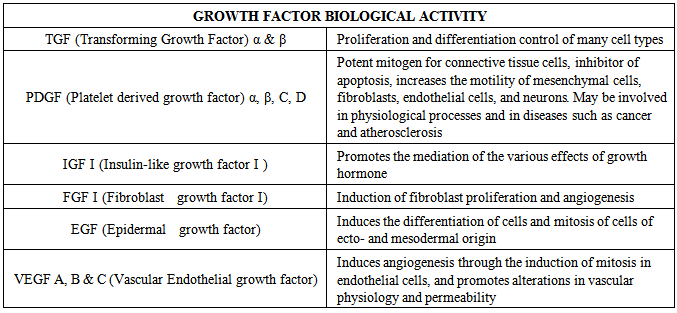
- The term Platelet-Rich Plasma (PRP) is a generic term used to describe a plasma suspension obtained from whole blood, prepared so as to contain platelet concentrations higher than those normally found in circulating blood [1]. Platelets are anucleated fragments of megakaryocytes, and are produced in the bone marrow. They contain granules consisting of various substances, which are released upon activation of the platelets [2]. Among the main substances that are released from these granules are growth factors (GF) (Table 1) [3], cytokines, adhesion molecules, integrins, and coagulation proteins [4].
|
2. Patients & Methods
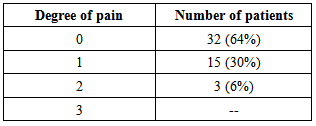
- This is an open therapeutic trial study performed at Laser Care Clinic in Amman, Jordan during the period from July, 1st 2013 to July, 1st 2014. Fifty patients (46 females and 4 males) with periorbital hyperpigmentationwere included in this study. Their age ranges from 19-60 years with a mean ± SD of 41.5 ± 9.63 years and median of 42 years. Their skin types were III – V (Fitzpatrick skin types). This study approved by the ethical committee in Al-Dholail hospital. Written informed consent was obtained from each patient.The treatment course consisted of three sessions of autologous platelet-rich plasma injections into the periorbital area as well as the whole face with one month apart in between the injections and followed up for additional three months to assess the level of improvement or recurrence of the dark circles.Exclusion criteria include patients with known platelet dysfunction syndrome, critical thrombocytopenia (<50,000/ul), any hemodynamic instability, or chronic medical illness (e.g. diabetes, chronic infections, and blood dyscrasias). Patients withlocal inflammatory skin disorders or active herpes infection at the site of the procedure were driven out of the study. Patients on consistent use of anti-coagulants or non-steroidal anti-inflammatory drugs (NSAID) within 48 hours of procedure, corticosteroid injection at treatment site within 1 month, systemic use of corticosteroids within 2 weeks, recent fever or illness, cancer- especially hematopoietic or of bone, and hemoglobin level< 10 g/dl were also excluded.The whole procedure was fully explained and thoroughly discussed with the patients about the mechanism of platelet-rich plasma treatment, the time required for the treatment, the behavior after the treatment, and the prospects of successful treatment, and any unrealistic expectations of the end results were strongly discouraged. The patients were informed about all risks that may be caused by the procedure and the pre- and post-operative care.Prior to each treatment, the face was cleansed with a mild non-abrasive detergent and gauzes soaked in 70% isopropyl alcohol. A topical anesthetic cream (EMLA, a eutectic mixture of local anesthesia of 2.5% lidocaine and 2.5% prilocaine, AstraZenica LP, Wilmington DE) was applied under an occlusive dressing for 1 hour and subsequently washed off to obtain completely dry skin surface. Topical antibiotics and a moisturizing cream were prescribed after each session and the patients were informed to apply a sunscreen all along the treatment course.Three photos were taken before treatment for each patient for both sides and the front of the face with a digital camera (Canon® EOS 500D Rebel T1i DigitalCamera, 15.1 megapixel HD) and another set of photos was taken in each visit post-treatment using identical camera settings, lighting, and patient positioning.Fifteen to twenty milliliter (ml) of blood was withdrawn from the patient using a butterfly cannula and a vacuum tube containing sodium citrate 3.2% as anticoagulant. The centrifugation process separates blood components owing to their different specific gravities, i.e., RBCs being the heaviest, followed by WBCs, whereas platelets are the lightest. The first centrifugation is slow to avoid spinning down platelets and to isolate plasma. The centrifugation was at 1600 rpm for 10 minutes. Platelets are mostly concentrated right on top of the buffy coat layer. The supernatant plasma was withdrawn and re-centrifuged. The subsequent centrifugation is faster at 4000 rpm for 10 minutes, so that platelets are spun down and separate as a pellet at the bottom of the tube from platelet-poor plasma (PPP) above. The final platelet concentration depends on the volume reduction of PPP. Approximately 3/4 of the supernatant is discarded and the platelet-rich pellet is re-suspended in remaining amount of plasma. The resultant plasma was aspirated and 0.1 ml of calcium chloride was added for each 1 ml of plasma to activate the platelets and then injected into the selected area using a 32-G needle for superficial microinjections via the mesotherapy technique, and the injections were administered in to the papillary dermis (1.5∼2.0 mm deep).Therapeutic outcomes were assessed by standardized digital photography by two blinded dermatologists using the following five-point scale: 0=no change; 1=slight improvement (0–25%); 2=moderate improvement (26–50%); 3=significant improvement (51–75%); 4=excellent improvement (>75%).The patients were asked to evaluate their own level of satisfaction by giving themselves a score from 0-4 points and the score was translated using the following scale:0=no change1=satisfied2=pleased3=very pleased4=excellentIn addition, the participants were asked to report any cutaneous or systemic side effects associated with treatment. In particular, a pain scale of 0–3 was used to determine the level of discomfort during the procedures as following:0=no pain1=mild pain2=moderate pain3=severe painStatistical data were analyzed by Chi test using Software Minitab V.16 and P value < 0.05 is considered statistically significant descriptive data by frequency, percent, figure and table.
3. Results
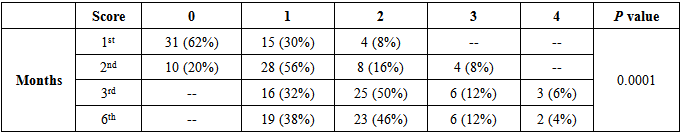
- Fifty patients (46 females and 4 males) were included in the study. All patients completed the study, including the 3-monthly sessions of PRP injections and the 3-month follow-up period. According to dermatologists' assessment (Table 2) the results after 1month were unpretentious (only 8% moderate improvement) but the number of patients that showed mild response is noteworthy (30%). Although weak at the start, the results were encouraging and showed dramatic changes thereafter through the subsequent months where the patients started to show more favorable response towards the end of treatment sessions. At the end of the 3rd session after 3 months all patients showed different levels of improvement, few patients showed significant (12%) and excellent (6%) responses while the majority expressed moderate (50%) improvement compared to the 1st month.
|
|
|
4. Discussion
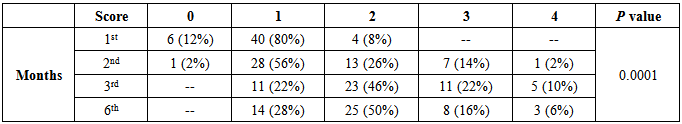
- The application of PRP has been documented in many fields. First promoted by M. Ferrari in 1987(31) as an autologous transfusion component after an open heart operation to avoid homologous blood product transfusion, there are now over 5200 entries in the National Center of Biotechnology Information (NCBI) for PRP ranging in fields from orthopedics, sports medicine, dentistry, otolaryngology, neurosurgery, ophthalmology, urology, wound healing, dermatology, cosmetic, cardiothoracic and maxillofacial surgery [32].The initial popularity of PRP grew from its promise as a safe and natural alternative to surgery. PRP advocates promoted the procedure as an organically based therapy that enabled healing through the use of one’s own natural growth factors. In recent years, scientific research and technology has provided a new perspective on platelets. Studies suggest that platelets contain an abundance of growth factors and cytokines that can affect inflammation, postoperative blood loss, infection [33], osteogenesis, wound, muscle tear and soft tissue healing. Research now shows that platelets also release many bioactive proteins responsible for attracting macrophages, mesenchymal stem cells and osteoblasts that not only promote removal of degenerated and necrotic tissue, but also enhance tissue regeneration and healing [34].Afresh PRP has been an emerging area of interest in aesthetic medicine. PRP has been reported to augment dermal elasticity by stimulating the removal of photodamaged extracellular matrix (ECM) components and inducing the synthesis of new collagen by dermal fibroblasts via various molecular mechanisms [35].Although periorbital hyperpigmentation is a mere color difference between the palpebral skin and the remaining facial skin, dark circles can be a significant cosmetic concern forpatients. Although it is a condition that doesnot cause morbidity, it can influence the quality of life from the medical point of view [36].The two most important factors in the pathogenesis of periorbital dark circles are the deposition of melanic pigment and hemosiderotic pigment in the affected sites. The melanic pigment deposition occurs as a consequence of excessive and cumulative exposure to the sun, which increases the production of melanin, while hemosiderotic deposition occurs due to intense vascularization in the palpebral region causing dermal blood extravasation. The liberation of ferric ions takes place locally, entailing the formation of free radicals that also stimulate the melanocytes, which generates melanic pigmentation [37].In this open therapeutic trial study, patients received one session of platelet-rich plasma injections per month for three months. The final outcome was evaluated after six months from the first session by two blinded dermatologists using standardized digital photography and by the patient's self-assessment. The results were very satisfactory, according to the dermatologists' evaluation, as almost as 60% of patients showed moderate to significant improvement. The patients' self-assessment of satisfaction was also high since more than 65% of patients said they were pleased or very pleased with end results; in fact the patients reported more favorable responses than those of the dermatologists'. This might be attributed to the fact that the patients were used to be very frustrated from their look and the long list of treatments used for so many months without really any acceptable results. The sensible change in their outlook and the improvement of the eyes' dark circle made the patients over estimate the results and give more hopeful and optimistic results than the dermatologists. This remarkable result which gives the patient a great feeling of being well treated is the most important target in any kind of treatment. These results give an overall indication of the effectiveness of PRP injections in the treatment of eye dark circles. The results of both assessment groups (the patients and the dermatologists) are significant as indicated by the P values which were 0.0001.The most important contents of platelets are contained in the α-granules. There are more than 30 bioactive substances in these granules [38]. Some of the bioactive substances present in the α-granules include platelet-derived growth factor(PDGF), transforming growth factor (TGF)-β1, 2, epidermalgrowth factor (EGF), and mitogenic growth factors such asplatelet-derived angiogenesis factor and fibrinogen. Toour knowledge, only TGF-β1 and EGF have been investigated about their relation with melanogenesis.Kim et al. investigated the effects of TGF-β1 on melanogenesis by using a spontaneously immortalized mousemelanocyte cell line, and asserted that TGF-β1 significantlyi nhibits melanin synthesis in a concentration dependent manner. They declared that TGF-β1 decreases melanogenesis via delayed extracellular signal-regulated kinase activation [39].While Yun et al. studied the effect of EGF on melanogenesis by using mouse-derived immortalized melanocytes from a laser-treated keratinocyte-conditioned culture media. They proposed that treatment with EGF lowers melanin production in melanocytes by inhibiting prostaglandin-E2 (PGE2) expression and tyrosinase enzyme activity. They offered that treatment with EGF can be used in cosmetics to whiten the skin and for the prevention of post inflammatory hyperpigmentation [40].Melasma was also reported to be successfully treated with PRP in a single Turkish study [41]. The researchers reported improvement of more than 80% of melasma after three sessions of PRP alone. This result was better than ours because periorbital hyperpigmentation is caused by a more complicated multifactorial mechanism than melasma and it is more treatment resistant. Despite the difference in results, both studies prove that PRP might be a good option for treatment of facial hyperpigmentation.The pigmentary improvement that occurs with PRP treatment may be also associated with the increase in skin volume. PDGF has a significant role in blood vessel formation and in the synthesis of collagen and components of the extracellular matrix, including hyaluronicacid. Hyaluronic acid has been shown to increase skin tone and volume, resulting in providing a more ‘glowing skin’ [42].Monthly intradermal injections of PRP in 3 sessions have shown satisfactory results in face and neck rejuvenation and scar attenuation [43]. In a split face blinded trial, Kang et al. proposed that PRP injections given monthly for 3 months, have shown very good results for infra-orbital rejuvenation as well, without any obvious side effects [44].Shin et al. showed that a combination of fractional non-ablative (erbium glass) laser therapy with topical application of PRP, resulted in objective improvement in skin elasticity, a lower erythema index and an increase in collagen density as well. Histological examination showed an increase in length of dermo-epidermal junction, amount of collagen and fibroblasts in the treated skin [45].Being an autologous preparation, PRP is devoid of any serious adverse effects, apart from local injection site reactions like pain or secondary infection, which can be avoided with proper precautions. PRP has no issues regarding transmission of infections such as hepatitis-B, C or HIV [46].The role of PRP injections in the treatment of periorbital hyperpigmentation is not fully considered. The studies that investigate their effect are lacking or very limited. Comparative studies are deficient to contrast PRP with other treatments like topical cosmeceutical preparations of growth factors. This might be attributed to the fact that PRP is relatively new technology introduced only recently in treatment of dermatological or cosmetic problems [47] and extensive further studies are highly recommended to confirm the results and endorse such maneuver as a successful way in alleviating the tragedy that some patients might suffer.In procedures aiming at aesthetic improvement, patient perception of the treatment outcome appears to be most important because it has a direct impact on patients’ body image and self-esteem [48]. Furthermore, many patients mentioned they experienced a remarkable improvement in ‘skin quality’ in addition to more stable and balanced skin color and subsequently can wear more natural makeup.In general, Platelet-Rich Plasma is a useful and relatively very safe treatment for periorbital hyperpigmentation and may provide an easy solution for a devastating problem.
 | Patient 1. Pre- and 3-months post-operative |
 | Patient 2. Pre- and 3-months post-operative |
 | Patient 3. Pre- and 3-months post-operative |
 | Patient 4. Pre- and 3-months post-operative |
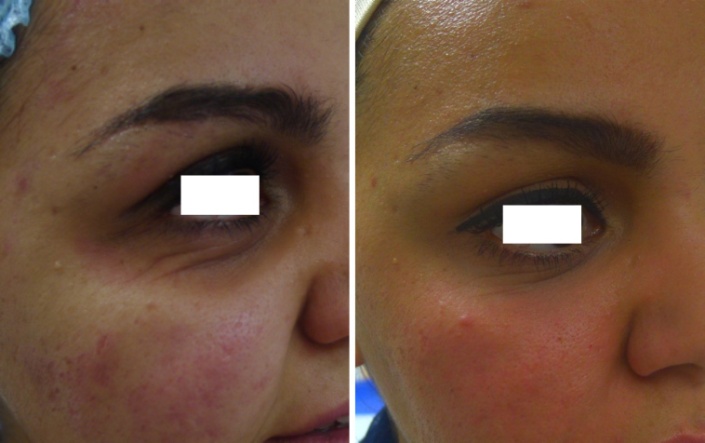 | Patient 5. Pre- and 3-months post-operative |
5. Conclusions
- PRP is a useful treatment for periorbital hyperpigmentation and further comparative studies of other treatment modalities are highly recommended.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML