-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2014; 3(3): 51-56
doi:10.5923/j.ajdv.20140303.01
An Investigation into the Effectiveness of Light Emitting Diodes on Treating Melasma on Skin Type VI
Nomakhosi Mpofana1, Cindy Ramhurry2
1Department of Wellness, Cape Peninsula University of Technology, Cape Town, 8000, South Africa
2Department of Applied Communicative Skills, University of Johannesburg, Johannesburg, 2000, South Africa
Correspondence to: Nomakhosi Mpofana, Department of Wellness, Cape Peninsula University of Technology, Cape Town, 8000, South Africa.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
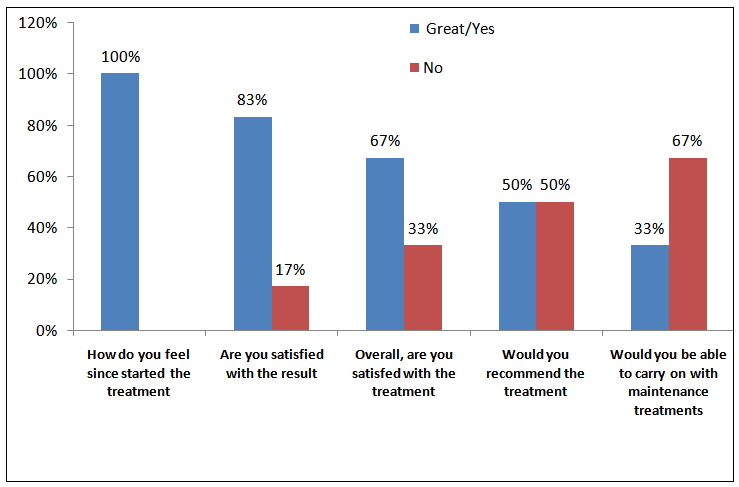
The literature highlights the higher prevalence of the condition of Melasma in women with Fitzpatrick skin type IV-VI and the risks and challenges involved in its treatment [1, 2, 3]. In this case study, we collected data from 6 confirmed cases of Melasma with Fitzpatrick skin type VI via record cards and visia analyses to investigate the effectiveness of Light Emitting Diodes (LED 633nm and 830nm) as a relatively risk free form of treatment. We specifically found that the LED (633nm and 830nm) generally improved skin texture, evened out skin tone, reduced the appearance of fine lines and wrinkles, refined enlarged pores and reduced porphyrins in the skin. In conclusion, we found evidence that LED (633nm and 830nm) may be effective in treating melasma in skin type VI.
Keywords: Melasma, Skin type VI, LED, Treatment, Prevalence
Cite this paper: Nomakhosi Mpofana, Cindy Ramhurry, An Investigation into the Effectiveness of Light Emitting Diodes on Treating Melasma on Skin Type VI, American Journal of Dermatology and Venereology, Vol. 3 No. 3, 2014, pp. 51-56. doi: 10.5923/j.ajdv.20140303.01.
Article Outline
1. Introduction
- Recent literature has shown an alarming increase in the occurrence of Melasma- an acquired, chronic, recurrent darkening of the skin on the face [4, 5]. The literature highlights the higher prevalence of this condition in women with Fitzpatrick skin type IV-VI and the risks involved in its treatment [1, 2, 3]. Writers contend that the wide spectrum of melanin absorption (250-1200nm) in darker skin types causes conditions such as post inflammatory hyperpigmentation, blistering, scabbing and in some cases, skin atrophy [6, 7]. Due to its disfiguring nature, melasma has been documented as a condition resulting in significant negative psychological and emotional impact [8]. Recent studies indicate a decrease in social functioning, decreased productivity at work and the lowering of self-esteem [9].The literature highlights the challenge in treating melasma in skin type VI. Most documented attempts have primarily relied on the use of invasive therapy, drugs and creams: these include ablative and non-ablative lasers, micro- dermabrasion, mesotherapy and topical de-pigmenting agents such as Hydroquinone, Kojic acid, Arbutin, Retinoids, Niacinamide, Mequinol, Kligman’s formula, Alpha Hydroxy, Beta Hydroxy and Fruit Acids [10]. These treatment modalities have been found to produce suboptimal results and undesirable side effects when treating dark skins phototypes [11, 12]. In the face of the challenges involved in treating melasma via invasive means, therapists have recently directed their energies towards exploring non-invasive channels of treatment in Fitzpatrick skin type IV-VI [13, 1]. Goldman [14] has gained the attention of skin therapists by offering a treatment that is arguably safe, user-friendly and available without a doctor’s prescription. Goldman [14] encourages the use of light emitting diodes in patients with skin type IV-VI. The literature shows evidence of LED as a more recent development which delivers narrow band, spectrally pure light of a specific intensity wavelength and dose to achieve clinically proven results [7]. LED is indicated to be a non-thermal, non-coherent and quasi-monochromatic light that has no down time on account of being a non-laser device [15, 16]. LED was initially used to treat actinic keratosis and superficial basal cell carcinomas, and has more recently been used to treat visible photo ageing induced by excessive sun exposure [3]. LED is seen as favourable for skin rejuvenation because it minimises the risk of the side-effects that ablative lasers present: LED systems are non–lasers, emitting no heat which avoids any thermal effect on the skin [17].In vitro studies evaluating the effect of LED on melasma have shown success: results have indicated that LED (830nm, 850nm, 940nm) inhibits the production of Tyrosinase in primary cultured melanocytes [18]. Other studies have found LED to be effective in the improvement of sun damage, (photorejuvenation) and pre-mature aging [14, 19, 17]. Although LED has shown much promise in theory, there is still a degree of vagueness and uncertainty regarding its use as a treatment option for melasma in skin type VI [6, 20, 21, 22]. On an empirical level, much research energy has been channelled into the use of LED as treatment option. However minimal research has been done to explore its response to melasma on skin type VI [2]. There is compelling evidence of the theoretical and/or practical need for more research into LED as a treatment option for skin type VI. In response to this need, our study was dedicated to investigating the effectiveness of LED as an alternative treatment modality for the problem of melasma in skin type VI. The study was guided by the following research question: What is the effectiveness of LED (633nm and 830nm) in the treatment of melasma on Fitzpatrick skin type VI?
2. Materials and Methods
- This study primarily adopted a qualitative research design because it centralises exploration, discovery and descriptive method analogy [23, 24]. A few quantitative techniques were additionally integrated into the design: data was analysed using a combination of both quantitative and qualitative techniques. Participants included six skin type VI women between the ages of 35 and 54with either dermal or epidermal melasma of the face. Participants were pre-assessed for melasma using two instruments: Visia Skin Analysis and Wood’s Lamp examination.
2.1. Time Schedule and Treatment Protocol
- The study followed a photo rejuvenation protocol of LED [25]. The total time scheduled to carry out the study was a period of fourteen weeks. The initial stage involved the following assessment activities: participants’ filling in of record cards, signing of consent forms and posing for a set of base-line photographs. In the subsequent stage, each participant was exposed to an LED 633nm treatment of 20 minutes. This was followed two days later by another exposure to LED 830nm light treatment. The Omnilux Medical, which was pre-set at 20 minutes, helped us to guard against any possibility of over- or under- exposure to the LED. As advised in the literature, the light panels of 633nm and 830nm wavelengths were positioned about three fingers from the participants’ face [25]. Once the treatment was done, a moisturiser suitable for the skin condition was applied. This was followed by the application of a broad spectrum sun protection factor of SPF 50.
2.2. Data Collection
- Data was collected using a structured standardised questionnaire which was also adapted to serve as a record card [23, 26]. This method provided us with an opportunity to recorda variety of participants’ characteristics as well as behaviour patterns [27, 26, 28]. Digital imaging was used to identify surface findings that could not be easily articulated [29]. Visia Complexion Analysis was then conducted on each participant to capture their respective complexion images. Visia Analysis as a method facilitated an objective evaluation of the skin allowing us to record standard, cross polarized and UV photography as well as to measure surface and subsurface skin conditions. With this quantitative assessment of the participants’ skin, we compared the skin’s features to other individuals of the same sex, age and skin type. As the treatments progressed, the Visia was used to track the changes in participants’ skin. The Visia analysis facilitated the conversion of test-taker’s original scores (raw scores) to a percentile score (which indicated how many people had scored below that score).
2.3. Data Analysis
- Data was analysed by comparing the digital images captured at base line with the images taken fourteen weeks after the completion of treatment. We looked for the following possible changes on the skin: the appearance of melasma, enlarged pores, skin texture, porphyrins, fine lines and wrinkles. Participants’ perspectives about the treatment, which were recorded throughout the process, were organised and are presented in this paper as themes [23]. We viewed participants’ descriptions of their emotional states at various stages as a significant form of feedback about the treatment. We particularly recorded any changes in self-confidence, self-esteem and general feelings about the self. We used graphs, percentiles, ratios and scores to indicate the holistic responses undergone by participants.
2.4. Reliability and Validity Issues
- To ensure high levels of reliability and validity, a position of reflexivity was adopted: every attempt was made to ensure that the same equipment was used throughout the study and that a standardised procedure was used for measurement. Standard methods were used to capture images, and to deliver the LED light treatment. We used triangulation to enhance the validity of our findings [23, 24].
2.5. Ethical Issues
- The following ethical procedures were observed: The study was cleared by the Ethical and Higher Degrees committee of University of Johannesburg. We explained the study in detail to the participants. This included its duration, equipment used, precautions and post care. We indicated that the study was voluntary and there were no costs involved. Participants were informed that they were at liberty to withdraw at any given time [23]. We made it known to participants that the Omnilux posed no known risks or health hazards. The right to privacy was enhanced by keeping all information declared to us as confidential. Participant’s names and their identities remained anonymous [24]. A letter of informed consent was signed by each participant [27].
3. Results
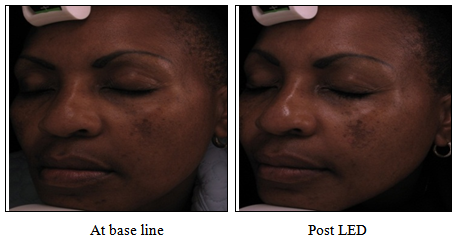
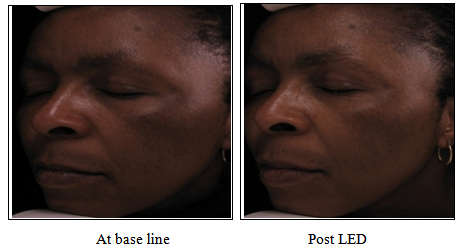
3.1. Photographs
- The analysis of photographs taken at the base line and after the completion of the LED treatment presented both positive and negative findings. In 5 out of the 6 participants we noted a significant improvement in skin tone, refined skin texture, less porphyrins, less fine lines and wrinkles, improvement of the naso-labial folds and a noticeable evening out of the skin (figure 1). On the other hand, 1 of the 6 participants displayed much darker melasma than before, suggesting that the pigmentation had worsened. Although the Visia complexion analysis confirmed the darkening of the melasma at completion of the treatments as compared to the base line images, it showed that the overall skin i.e. skin texture, enlarged pores, porphyrins, fine lines and wrinkles, had improved.
 | Figure 1. Improvement of melasma as well as the nasolabial folds was noted |
 | Figure 2. Darkening of melasma were noted at post LED treatments |
3.2. Complexion Analysis
- Visia printouts revealed that the participants’ complexions had improved significantly. All 6 participants indicated less fine lines and wrinkles. The porphyrins appearance showed general improvement and the cases of enlarged pores showed refinement.
 | Figure 3. Improved complexion and melasma was noted |
3.3. Record Cards
- In examining the participants perceptions of their experiences with the LED we found that 5 out of the 6 responded positively indicating that they had experienced some form of improvement in their skin after the fourteen week period. These respondents used descriptions such as “my skin feels softer”, “it seems to glow” “it looks healthier” and “it feels renewed’. Participant’s responses to the satisfaction questionnaire (figure 4) indicated more optimism at the post-treatment stage. For example, participant B stated that she had “gained more self-confidence” and participant C stated that she was “not as embarrassed” about her image as she was prior to the treatment. 1 of the 6 participants responded with negativity towards the end of the treatment period expressing “disappointment” that her pigmentation looked darker and much more pronounced than prior to the treatment.
4. Discussion and Conclusions
- Our study of LED (633nm and 830nm) on melasma in skin type VI provides some evidence of its ability to improve skin texture, even out skin tone, reduce the appearance of fine lines and wrinkles, refine enlarged pores as well as reduce porphyrins in the skin. In this study LED 633nm and 830nm light treatment has been found to have the added benefits of reducing visible signs of pre-mature ageing. While the literature is sparse, as in our study, an Invitro study conducted by Kim et al. [18] who used cultured human melanocytes to evaluate the effect of LED on melasma, likewise found success. In their study, results indicated that LED inhibits the production of tyrosinase in primary cultured melanocytes. The findings in this study indicate that the LED (633nm and 830nm), which is suggested to have photorejuvenation properties, helped reverse the signs of sun induced damaged. These findings support those of Goldberg [19] who also found the LED to be effective in the improvement of pre- mature ageing. In the use of LED, the results indicated minimal side effects experienced by the participants. This is also in accordance with the findings of Goldman [14]. The literature indicates that most studies conducted on the treatment of melasma have used a combination therapy approach [30, 2, 4]. This study, on the contrary, used LED as a form of monotherapy. The advantage in using such an approach is that it allowed us to isolate the LED and evaluate its unique potential to relieve the condition of melasma. If we had done a study which combined LED with a natural skin lightening cream i.e. Vitamin C or licorice root extract, we may have had to deal with a host of complex variables. It is well documented that relapse is common in chronic melasma [31]. During the study we observed that all the participants had adapted with ease to the new protocol of skin care regimen. We were curious to know whether they would continue with the new learned routine or if they would revert to their old habits once the given skin care range was completed. A major limitation in this study was the use of the specified tools to analyse the skin for possible changes. Melasma was not clearly indicative. We found it limiting that the Woods lamp did not indicate the contrast of melasma in the participant’s skins due to the fact that skin types VI are deeply pigmented. The Visia complexion analysis was also not entirely successful in providing a reading of UV damage and brown spots on all 6 participants. On fair skins (I-III), this feature usefully displays to patients the status of photo damage on their skins. We highlight the point that the diagnostic equipment in the skin care industry needs to be reviewed in terms of its suitability for use on all skin types, and particularly skin type VI. In our attempts to deal with this limitation we came across other techniques suggested by the literature to describe and evaluate the degree of improvement of melasma. One of these includes the Melasma Area and Severity Index (MASI) which is a subjective assessment scale used in grading melasma treatment outcomes. We recommend that future studies on skin type VI take such techniques into serious consideration.It was concerning to note that all 6 participants did not use sun protection nor were they aware of the irreversible possibility of photo damage. This finding raises an important socio-political issue. Trends in South Africa show that people of darker skins displayed particularly resistant attitudes towards skin care in the past [32, 33]. Going to a skin care clinic or a health spa was traditionally regarded as taboo and a waste of scarce financial resources among black people in South Africa. Understandably, this sector of the population in South Africa who have been historically disadvantaged by racial segregation prioritised their survival, giving little focus to other facets of their existence. This study has brought to the fore an important realisation: misperceptions still exist in South Africa about dark skin being free from the risk of sun damage or free radicals. This study has raised awareness of the dire need for particularly educating skin types VI in South Africa about the importance of using sun protection factor.In conclusion, we found evidence that LED (633nm and 830nm) may be effective in treating melasma in skin type VI. We found evidence of LED 633nm and 830nm light treatment providing the added benefit of reducing visible signs of pre-mature ageing and photo damage.
ACKNOWLEDGEMENTS
- We are indebted to Dr Chris Ladas for his technical support and the Laser Touch Aesthetic Clinic for the use of its facilities to conduct the study.
Conflicts of Interest
- The authors state no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML