-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2014; 3(1): 1-4
doi:10.5923/j.ajdv.20140301.01
Hidradenitis Suppurativa (HS), in Association with Helicobacter Pylori, in a Female Sudanese Patient: Case Report
Adil H. H. Bashir 1, 2, Waleed M Elamin 3, Lamyaa A El Hassan 4, Abdel Khalig Muddathir 2, 3, Khalid O. Alfarouk 1, 2, Ahmed M El Hassan 1
1University of Khartoum, Khartoum, Sudan
2H. Alfarouk Cancer Center, Khartoum, Sudan
3El Zaeem El Azhary University, Khartoum North, Sudan
4Faculty of Medicine, Ahfad University for Women, Omdurman, Sudan
Correspondence to: Adil H. H. Bashir , University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Hidradenitis suppurativa (H S) is an annoying chronic condition characterized by swollen, painful and inflamed lesions in the axillae, groin, and other parts of the body that contain apocrine glands. The disease was originally attributed to a chronic acneiform infection of the apocrine glands but more recently it was documented to be due to a folliculitis. The hallmark of the disease is sinus tracts and draining fistulas in the skin. We reported here a rare case of H S in a 26 years old Sudanese female, who, presented with insidious onset and progressive course of nodulo-pustular lesions that discharged foul pus of 2 month duration. The lesions involved the chin, cheeks and the forehead. The diagnosis was confirmed by histopathology. By immunostaining the lesions were positive for Helicobacter pylori antigen. A stool examination was positive for H. pylori infection. The patient responded well to ant- H. pylori therapy and the lesions regressed.
Keywords: Hidradenitis suppurativa, Apocrine acne, Acne inversa, Helicobacter pylori
Cite this paper: Adil H. H. Bashir , Waleed M Elamin , Lamyaa A El Hassan , Abdel Khalig Muddathir , Khalid O. Alfarouk , Ahmed M El Hassan , Hidradenitis Suppurativa (HS), in Association with Helicobacter Pylori, in a Female Sudanese Patient: Case Report, American Journal of Dermatology and Venereology, Vol. 3 No. 1, 2014, pp. 1-4. doi: 10.5923/j.ajdv.20140301.01.
Article Outline
1. Introduction
- Hidradenitis Suppurativa is a rare dermatitis of unknown etiology and is difficult to treat (1). Historically the disease was believed to be due to a chronic acneiform infection of the cutaneous apocrine glands. Recent evidence points to its being a follicular disease [1-4]. It may be associated with smoking [5], lithium [6], oral contraceptives [7] and HIV infection [8]. Herein we report an unusual case of HS in a Sudanese female. The lesions were mainly in the chin and forehead, sites that were not reported before to be involved in this condition.
2. Case Description and Methods
- A 26 years old Sudanese female patient, reported with a progressive course of a nodulo-pustular skin lesions discharging offensive pus of 2 months duration. She was examined clinically and the type of and distribution of the skin lesions was recorded. Hematological investigations included estimation of hemoglobin level, ESR, total and differential white cell count and platelet count. Other tests included liver function tests, stool examination for H pylori infection, HIV test, random blood sugar level and VDRL RPR. All tests were performed before and after treatment. A skin biopsy from the chin was performed. The biopsy was fixed in 10% neutral formalin. Sections were stained with hematoxlyn and eosin and immunohistochemically for H pylori using a specific monoclonal antibody (Dako, Denmark) according to the instructions of the manufacturer.
3. Results
- On examination the patient looked well and was afebrile. The spleen and liver were not enlarged and there was no lymphadenopathy. Dermatological examination showed localized individual crusted nodulo-pustular lesions discharging yellowish pus. The lesions were mainly in the chins with fewer but similar lesions in the cheeks and the forehead (Figure 1, 2). The palms, soles nails and the rest of the skin were normal.
 | Figure 1. shows papulo-pustular lesions at chin |
 | Figure 2. shows papulo-pustular with multiple sinuses lesions chin and low cheek |
4. Investigations Done
4.1. Skin Biopsy
- A skin biopsy showed several changes in the epidermis and dermis. In several foci there was follicular plugging (Figure 3), Invagination of the epidermis into the dermis formed keratin filled cysts containing neutrophils (Figure 4). The rest of the dermis showed periadnexal inflammation and an acute and chronic inflammatory infiltrate involving hair follicles. One of the latter shows almost complete destruction of its wall by inflammatory, mainly neutrophils. A hair follicle had been completely destroyed leaving a cross section of a hair surrounded by neutrophils (Figure 5). Using a monoclonal antibody against H pylori, H pylori antigen was detected in histiocytes in the lesions (Figure 6). Some foreign body giant cells were also seen. These were probably a reaction to keratin fibersDiagnosis: Hidradenitis Suppurativa.
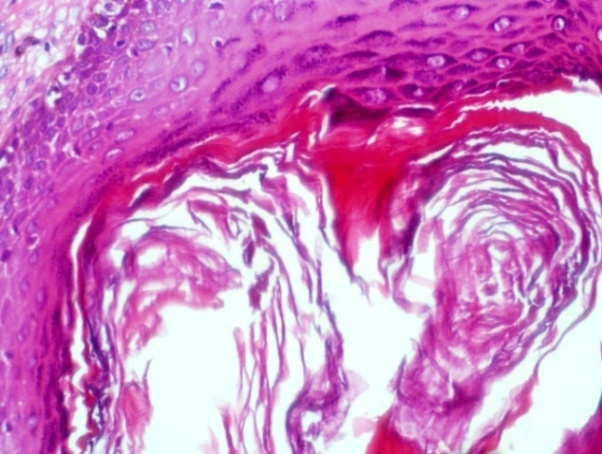 | Figure 3. Showing follicular plugging (H&Ex40) |
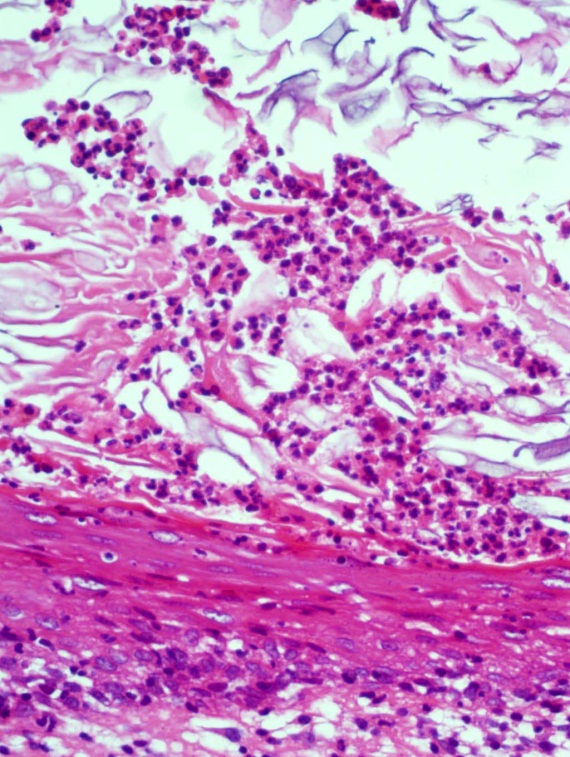 | Figure 4. A keratin cyst in the dermis containing neutrophils |
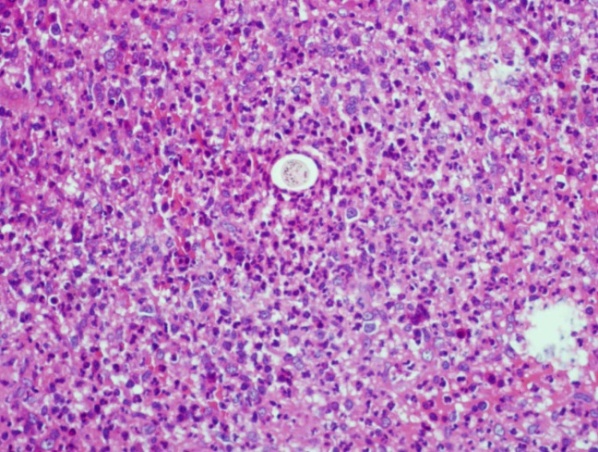 | Figure 5. In the center of the field is a cross section of a hair surrounded by dense neutrophil infiltration. (H%E x40) |
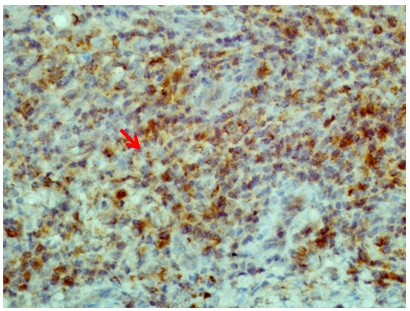 | Figure 6. H pylori antigen in the cytoplasm of mononuclear cells; the rod-like structure is probably a whole bacterium (Immunoperoxidase stain x40) |
4.2. Hematological Changes
- Before treatment the total white cell count was 14.500/DL with a neutrophil leucocytosis. Lymphocytes, basophils and eosinophils were within normal limits. After treatment, the total white cell count fell to 4500/DL and the differential was normal. The ESR was 69 mm in the first hour before treatment and returned to normal after therapy.
4.3. Biochemical Profile
- A random blood sugar was normal. Before treatment the total bilirubin was 20 (Normal 5-17). The direct bilirubin level was 4. Total protein was 69 T bilirubin mg/dl (normal (64-83). ALP-AMP 188uL (normal 20-115). After treatment all tests were normal.Culture from the discharging sinuses for bacteria was negative.
4.4. Treatment
- The patient was treated with Amoxicillin + Clavulinic acid1g BD intravenous for 10 days, Metronidazole 1g drip infusion OD for 3 days and Pantoprazole 40 mg OD for 5 days the followed by 40 mg with oral Pantoprazole OD for 4 weeks The lesion regressed markedly after therapy (Fig 7, 8). A serum ICT Ab was positive for H. pylori and became negative for stool Antigen done after anti H. pylori treatment.
 | Figure 7. The patient after anti H pylori treatment; lesions have markedly regressed |
 | Figure 8. Lesions on the cheek after treatment |
5. Discussion
- H S is a rare chronic disease of unknown cause that usually affects the genitofemoral, perianal and axillary areas [1-4]. Lesions are painful nodulo-pustules that discharge pus with a foul odor. The disease is more common in women [5]. The prevalence is about 1-2% in the population though a Danish study reported a prevalence of 4% among women [5]. There appears to be a genetic predisposition since it often affects members of the same family [6]. The disease may be triggered by smoking [7] and lithium [8]. Some other conditions associated with H S are: Crohn’s disease [9], Irritable bowel syndrome, Down syndrome , certain forms of arthritis [10], HIV infection [11] Graves disease or Hashimoto thyroiditis, Sjögren's syndrome and Herpes simplex. None of these were found in this patient. The pathology of the lesions in the present case is typical of H S. There was folliculitis associated with follicular plugging and an inflammatory infiltrate composed of neutrophil that destroyed the follicles. Historically the disease was believed to be due to a chronic acneiform infection of the cutaneous apocrine glands but recent evidence points to HS as being a follicular disease. This was confirmed in this patient since no affected apocrine glands were identified in the pathology of the lesions Furthermore the disease affected the face, a feature which as far as we are aware, was not described previously.This patient had a positive H. pylori infection which cleared after anti- H pylori triple therapy. H pylori antigen was demonstrated in the lesions by immunostaining. There was no evidence of other factors believed to cause or trigger the infection in the present patient. The anti-H. pylori treatment was associated with the apparent cure of the disease. The abnormal hematological changes and liver function returned to normal after drug treatment of H. pylori. The pathology in the liver might have been caused by H pylori although we do not have concrete evidence for this. We suggest that H S may be caused by H. pylori, at least in some cases. Based on a number of reports, possible relationships of H. pylori infection to a variety of different dermatoses have been suggested [11].
6. Conclusions
- Hidradenitis Suppurativa is a rare dermatitis and the treatment is difficult because the underlying pathogenic mechanism is unknown. Finding a method for HS treatment is of a paramount importance. In severe cases of H S as in this case, the patient may suffer a constant succession of new lesions forming as soon as old lesions heal. The patient presented with a chronic condition in which the multiple nodules had coalesced and were surrounded by a fibrous reaction. This resulted in scarred and unsightly appearance of the area. Hidradenitis may be observed as a primary condition without any obvious cause, but it may be observed in association with the following conditions: Crohn disease, Irritable bowel syndrome, Down syndrome, certain forms of arthritis, Graves's disease or Hashimoto thyroiditis, Sjögren's syndrome and Herpes simplex. In this patient it was associated with H. pylori infection and using a monoclonal antibody against H. pylori, H. pylori antigen was detected in histiocytes in the lesions. The patient responded well to eradication with triple therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML