-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2013; 2(4): 39-41
doi:10.5923/j.ajdv.20130204.01
Eosinophilic Folliculitis (Ofuji's Disease) and Mucosal Involvement, in Association with Helicobacter pylori in Sudanese Patient
Adil H. H. Bashir1, Lamyaa A. M. Elhassan2, Abdel Khalig Muddathir1, Khalid O. Alfarouk1, Ahmed M. El Hassan1
1University of Khartoum, Khartoum, Sudan
2Ahfad University for Women, Omdurman, Sudan
Correspondence to: Adil H. H. Bashir, University of Khartoum, Khartoum, Sudan.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Eosinophilic Folliculitis (EF) is a rare dermatosis and the treatment is difficult because the underlying pathogenic mechanism is unknown. We reported rare case, 4 years duration of Eosinophilic Folliculitis (EF), of married female patient, fifty years old, presented with insidious onset of skin colored and slightly pigmented, discrete widespread, clustered and diffuse non itchy, papulo-pustular lesions with central erosions and crustation, mainly at axillae, sub mammary, and right nasal fold. Vermilion shows to be dry, fissure and crusted, with chronic dyspeptic symptoms. The cases were diagnosed and confirmed histopathologically as Eosinophilic Folliculitis with Helicobacter pylori test positive, considered to be the first case of EF been reported in Sudan and as a mucosal one in particular.
Keywords: Eosinophilic Folliculitis, H. pylori,Immunology
Cite this paper: Adil H. H. Bashir, Lamyaa A. M. Elhassan, Abdel Khalig Muddathir, Khalid O. Alfarouk, Ahmed M. El Hassan, Eosinophilic Folliculitis (Ofuji's Disease) and Mucosal Involvement, in Association with Helicobacter pylori in Sudanese Patient, American Journal of Dermatology and Venereology, Vol. 2 No. 4, 2013, pp. 39-41. doi: 10.5923/j.ajdv.20130204.01.
Article Outline
1. Background
- Eosinophilic folliculitis (EF), also known as Eosinophilic pustular folliculitis or sterile eosinophilic pustulosis, is a rare follicular pruritic papular eruption observed in association with human immunodeficiency virus (HIV), though it can occur in HIV-negative individuals where it is known by the eponym Ofuji disease (OD)[1].Eosinophilic pustular folliculitis is a rare but important disease entity presenting with recurrent indurated erythematous papulopustular and plaques on the face. Increased awareness of this condition is important as it can mimic many other conditions presenting as red plaques on the face[2].The diagnosis of EF is based on the histologic findings consisting of a sterile inflammatory infiltrate rich in eosinophils involving hair follicles. EF in HIV patients is believed to be an immuno inflammatory response directed either at follicular or skin flora antigens in the late-stage of HIV infection. In this stage, immune response is characterized by a shift from a Th1- to a Th2-dominant cytokine profile and an increased secretion of interleukin-4 and interleukin-5, both known to promote eosinophilia[3].OD is an uncommon generalized pustular dermatosis of infancy with associated eosinophilia[4]. Eosinophilic pustular folliculitis in children is a rare follicular inflammatory dermatosis, usually occurring early in life. The disease progresses in flares of prurigenous plaques studded with papules and sterile pustules of the scalp and other areas of the skin. The mucosal involvement seen in patients in one study has never been reported in the literature neither in the infancy nor in the adult form[5].OD or eosinophilic pustular folliculitis and human immunodeficiency virus-associated eosinophilic folliculitis (HIV-EF) both show eosinophil -rich folliculocentric infiltrates, and it is not clear whether they are distinguishable pathologically. So it is suggested that OD and HIV-EF are indistinguishable pathologically and the diagnosis requires clinical correlation. Follicular Mucinosis (FM) was not uncommonly seen in lesions of OD. OD with FM may be difficult to differentiate from FM, especially in cases presenting with non-annular or non-pustular lesions, but the diagnosis might be facilitated by finding eosinophil-rich pustule, microabscess, or infiltrate in pilosebaceous units microscopically[6].EF has been to occur in a patient affected by Hodgkin lymphoma[7]. Eosinophilic pustular folliculitis can be induced by allopurinol and timepidium bromide[8]. Eosinophilic pustular folliculitis associated with parasitic infestations in some cases[9]. The histopathology of folliculitis in HIV-infected patients is protean. No single factor could be identified as the cause, making targeted antibacterial or antifungal therapy unlikely to be successful across a wide range of patients[10].Helicobacter pylori infection leads to gastritis, duodenal or gastric ulcer and even in rare cases to gastric carcinoma or Mucosa Associated Lymphoid Tissue (MALT) lymphoma. Based on a number of reports, a possible relationship of H. pylori infection to a variety of different dermatosis has been suggested, including urticaria, rosacea, acne rosacea, atopic dermatitis, alopecia areata, Sjögren’s syndrome, Schönlein - Henoch purpura, and Sweet’s syndrome[11].
2. Case Report
- A female patient, married, 50 years old, house wife, descent from second degree relative parents, resident in Dar Alsalam, belongs to Noba tribe (Darker Skin).The condition started 4 years ago with insidious onset and progressive course, with skin colored widespread diffuse and discrete non itchy, papulo-pustular lesions, with central erosions and crustation, mainly at axillae, sub mammary, and right nasal fold. Vermilion show to be dry, fissure and crusted. The condition is not associated fever or any constitutional manifestations rather than chronic dyspeptic symptoms.
3. General Examination
- The general condition is good, not pale, not icteric, as well no palpable spleen, and liver. No palpable lymph nodes.
4. Dermatological Examination
- On dermatologic examination of the patient, widespread, clustered symmetrically distributed erythematous centrally eroded and crusted papulo-pustular lesions; firm and tender. Skin overlying fixed, and hyperpigmented. Lesions size varies from 0.5-1cm, involving mainly axillae, sub mammary, and right nasal fold. Lower lip vermilion found to be dry, eroded, fissured and crusted with swollen, erythematous and slightly eroded lower lip mucosal surface. Similar lesions were seen on both soles and palms. No dystrophy was noticed on nails, also no abnormality was detected in ears nor hair. On oral cavity examination, the lower lip mucosa was swollen and slightly eroded with fissured tongue.Palms and soles: Similar lesions at both soles and palms.Nails: No nails dystrophy has been noticed.Ears: No Abnormality Detected.Hair: No Abnormality Detected. Oral cavity: lower lip mucosa swollen and slightly eroded with fissured tongue.
5. Investigations Done
- In skin biopsy taken from upper chest, the lesion showed show hyperkeratosis, Acanthosis, spongiosis and follicular plugging (Figure 1). The hair follicles are dilated and contain a dense collection of eosinophils with few neutrophils in some follicles (Figure 2). The surrounding dermis shows lymphocytic and plasma cell infiltration. The diagnosis was Eosinophilic Folliculitis.
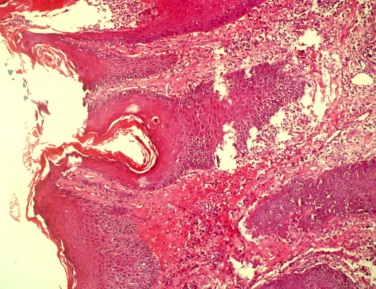 | Figure 1. Shows follicular plugging (H&Ex40) |
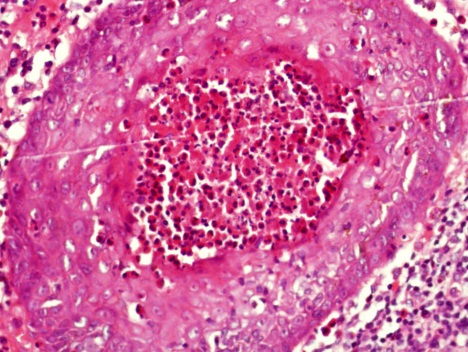 | Figure 2. Shows eosinophils in the lumen of a follicle. The epithelium lining the follicle shows spnogiosis (H&Ex40) |
6. Treatment
- Good response has been noticed where patient received first line triple therapy, as Doxycyclin 100 mg bid for 10 days, Cefixime 400 mg for 5 days and Rabeprazol as proton pump inhibitor (PPI) 20 mg for 28 days. After that, H. Pylori – stool Ag test has been done to show antigen was not detected.
7. Discussion
- Eosinophilic Folliculitis is a quite rare presentation especially in Africans and underlying pathogenic mechanism is unknown[12]. The mucosal involvement seen in patients in one study has never been reported in the literature neither in the infancy nor in the adult form[5] as seen in this case.Our case had an adult onset of presentation. Clinical features and histopathology were typical; it was associated with H. Pylori, patient showed good response to triple therapy. where focus as possible antigen is of paramount concern as possible causative antigen as in this case all serological specific tests for EF were negative while H. Pylori ICT test was the only positive test and turn negative after taken specific treatment (triple therapy), with no remission.
8. Conclusions
- Response of Eosinophilic Folliculitis to triple therapy as H. pylori considered to be a possible causative underlying cause and as it had been known that a definite cause was not clear and no specific treatment was known to be effective, so in this case it might focus new era to diagnose and treat EF as difficult one to be treated.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML