-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2013; 2(1): 1-4
doi:10.5923/j.ajdv.20130201.01
Pityriasis Amiantacea:Its Clinical Aspects, Causes and Associations; a Cross Sectional Study
Mohammed Y. Abbas 1, Maytham M. Al-Hilo 2, Ghalawish Ahmed 1, Dahlia M. AL-Katteb3,*
1MBChB, FICMS,Al-Kindy College of Medicine ,Baghdad University; Baghdad , Iraq
2MBChB, FICMS, DV, Consultant Dermatologist and Venereologist, Al-Kindy Teaching Hospital, Baghdad, Iraq
3MBChB, Al-Kindy Teaching Hospital, Baghdad, Iraq
Correspondence to: Dahlia M. AL-Katteb, MBChB, Al-Kindy Teaching Hospital, Baghdad, Iraq.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This cross sectional study was done in Al- Kindy Teaching Hospital in Iraq in the period between October 2010 and October 2012. Theaim of this study was to shade light on pityriasisamiantacea regarding its clinical aspects, causes and associations. Seventy six patients with pityriasisamiantacea were enrolled in this study including 26(34.21%) male and 50(65.78%) females. Their ages ranged between 3 months to 68 years and the median was 13 years. Full history and detailed clinical examination was done for each patient. Swab for culture and skin scrapping as well as hair plucking for mycological examination to detect any bacterial and fungal infections was done to all patients.Skin biopsy and histopathological examination were done for only ten cases . The most age group affected was between (10-19) years that represents (36.8%). Pityriasisamiantacea was more common in females patients (65.8%).The disease was generalized in 48(63.15%)patients, localized in 24(31.57%) patients while the diffuse involvement of the scalp was in 4(5.26%) patients. The results revealed that pityriasisamiantacea in 45(59.2%) patients was caused by psoriasis,seborrheicdermatitis , atopic dermatitis and tineacapitis respectively.Twenty three patients (30.26%) were found to have a secondary bacterial infection and the highest figure of secondary bacterial infection in patients with pityriasisamiantacea were found in atopic dermatitis patients (66.67%).
Keywords: Pityriasisamiantacea, Psoriasis ,Seborrheic Dermatitis , Atopic Dermatitis, Tineacapitis
Cite this paper: Mohammed Y. Abbas , Maytham M. Al-Hilo , Ghalawish Ahmed , Firas Al-Samarai , Pityriasis Amiantacea:Its Clinical Aspects, Causes and Associations; a Cross Sectional Study, American Journal of Dermatology and Venereology, Vol. 2 No. 1, 2013, pp. 1-4. doi: 10.5923/j.ajdv.20130201.01.
Article Outline
1. Introduction
- Pityriasisamiantaceais a characteristic eruption of unknown etiology.(1) It was first described by Alibert in 1832, and was called ‘la porrigineamiantacée’ because its scales resemble the grayish substance surrounding the feathers of juvenile and molting birds and have the appearance of asbestos (amiante).(2,3) Some authors believe that pityriasisamiantacea is a form of eczema or psoriasis.One patch or several patches of dense scale appear anywhere on the scalp and may persist for months before the parent notices temporary hair loss or the distinctive large, oval, yellow-white plates of scale firmly adhered to the scalp and hair.Characteristically, the scale binds to the hair and is drawn up with the growing hair. Patches of dense scale range from 2 to 10 cm. The scale suggests fungal scalp disease, which explains the designation tinea. Amiantacea, meaning asbestos, refers to the plate- like quality of the scale, which resembles genuine asbestos.Hair loss, sometimes cicatricial, is seen inpityriasisamiantacea.(1)Theaim of this study is to shade light onpityriasisamiantacea regarding its clinical aspects, causes and associations.
2. Patients and Method
- This cross sectional study was done in Al-Kindy Teaching Hospital in Iraqin the period between October 2010 to October 2012. This study was approved by the ethical committee in AL Kindy Teaching Hospital.All cases presented with a scaly scalp were clinicallyassessed and those who were diagnosed as pityriasisamiantacea were included in this study.Seventy six patients with pityriasisamiantacea were enrolled in this study including 26(34.21%) male and 50(65.78%) females. Theirages rangedbetween3 months to 68 years and the median was 13 years. Each patient or theirparentsreceived a completeexplanation of the nature and purpose of the study and an oral consent was taken before they were included in this study.Full history and detailed clinical examination was done for each patient emphasizing on the following: age, sex , age of onset , family history of the disease.and when there is pruritus, its severity was assessed subjectively by the patientinto mild, moderate or severe. In addition to the degree of extension of pityriasisamiantacea(localized, generalized or diffuse) and the presence or the absence and type of hair loss. Swab for culture and skin scrapping as well as hair plucking for mycological examination to detectany bacterial and fungal infections was done to all patients.Skin biopsy and histopathological examination were done for only ten cases.
3.Results
3.1. Age Distribution
- The age of the included patients ranged from 3 months to 68 years with median of 13 years. The most age group affected was between (10-19) years that represents 36.8% , while the least figure wasin the age range between (40-49 years) representing 1.3%. Fig 1
3.2. Gender Distribution
- Pityriasisamiantacea were more common in females patients 50(65.8%) than males 26(34.2%)patients .
3.3. Duration of the Disease
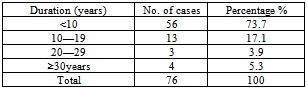
- The duration of the disease was extending from 2 months to 35 years with a median of 5 years as shown in table 1.
|
3.4. The Family History
- The family history of pityriasisamiantacea was positive in 31(40.8%) patients .
3.5. Pruritus
- The pruritus was reported in 66 amiantacea patients (86.84%).Thirty patients of them showed a mild pruritus(39.47%);In 26 (34.21%) patients, the pruritus was moderate while it was severe in 10 patients(13.15%).
3.6. Hair Loss
- Hair loss was seen in 18(23.68%) patients; seven teenth patients (22.7%) were with non scarring and only one patient(1.31%) was with scarring alopecia.
3.7. Degree of PityriasisAmiantacea
- The disease was generalized in 48(63.15%) patients, localized in 24(31.57%) patients while the diffuse involvement of the scalp was in 4(5.26%) patients.
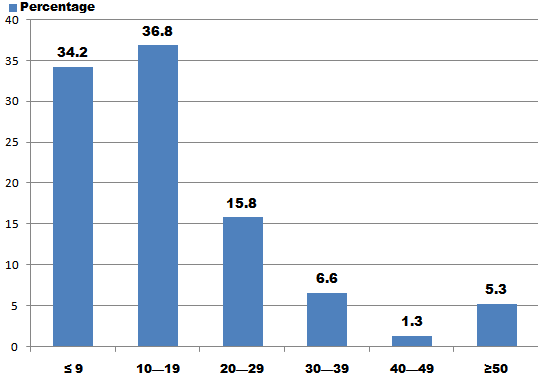 | Figure 1. Distribution of pityriasisamiantacea patients according to age |
3.8. Underlying Pathology
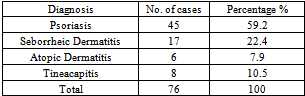
- These results revealed that the underlying pathology of pityriasisamiantacea in 45(59.2%) patients was caused by psoriasis, followed by other causes such as seborrheic dermatitis in 17(22.4%) patients , atopic dermatitis in 6(7.9%) patients and tineacapitis in 8(10.5%) patients, as shown in the table 2 below .The results of histopathological examination often patients goes with psoriasis in five patients which was comparable with the clinical diagnosis; in the other five patients the histopathological examination goes with dermatitis, depending on the patient’s profile, we cited these patients into either atopic orseborrheic.
|
3.9. Secondary Bacterial Infections
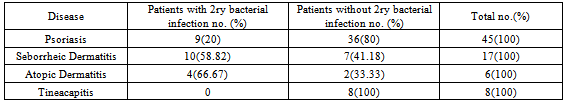
- Twenty three patients (30.26%) were found to have a secondary bacterial infection; the distribution of these patients according to etiology is shown in table 3.The highest figure of secondary bacterial infection in patients with pityriasisamiantacea were foundin atopic dermatitis patients 4 (66.67%) patients followed by seborrheic dermatitis in 10(58.82%)patients.None of pityriasisamiantacea patients caused by tineacapitis found to have secondary bacterial infection.
|
4. Discussion
- Pityriasisamiantacea is a reactive process of the scalp often without evident cause or it may be observed as complication or sequel of streptococcal infection, seborrheic dermatitis, atopic dermatitis or psoriasis.(2,4)Despite that pityriasisamiantacea is a well known distinct clinical entity, for the best of our knowledge, there were limited number of researches about its aetiology and associations.Abdel-Hamid etal and Knight G(5,6)had revealed that pityriasisamiantacea may occur at any age from 5 years up to 63 years. In our study, the age ranged from 3-68 years .This variation in the age ranges might be attributed to the wide range of age groups of the underlying pathology.As previously demonstrated, Pityriasisamiantacea appears primarily to affect the younger age groups.(5)The most commonly affected age group in this study was between 10-19 years while the least affected group ranged from 40-49years. This is similar to previous reports. However, the most commonly involved age group is dependent on the underlying pathology. Our study appointed female predilection in a ratio of 1.9:1.This is similar to previous published studies which had revealed that females were affected more than males.(5,6,7,8)Although female predilection can be explained by the fact that females in our society seek medical care for cosmetic reason more than males, the actual female: male ratio would eventually follows that of primary disease.All the patients in this study showed a duration of pityriasisamiantacea extending from 2months to 35 years. This is identical to what had previously published.(5) The wide variation in the duration could be closely attributed to the underlying pathology. The inflammatory diseases like psoriasis, atopic and seborrhoic dermatitis may takes a long course with exacerbation and remission.(9,10)while diseasesof infectious origin as tineacapitis takes a shorter course.(2,7,11,12)This study reported pruritus in 66 patients(86.84%);thirty patients of them revealed mild pruritus, twenty six(34.21%) patients show moderate pruritus while ten others(13.16%) had severe pruritus.Apparently, it seems that the existence and the severity of pruritus are chiefly related to the disease of origin; e.g. in patients with atopic dermatitis confined to the scalp that associated with adherent silvery scale suggesting pityriasisamiantacea , the pruritus is usually a major feature.(7)Hair loss has been variably reported inpityriasisamiantacea.In this study, eighteen(23.07%) patients had anon scaring hair loss and only one showed a scarring hair loss associated with tineacapitis.It has been reported that pityriasisamiantacea is associated with temporary hair loss.(6,8,13) Cicatricial alopecia is sometimes seen in psoriasis;(5,14)although it may occur , common scalp psoriasis is not a frequent cause of alopecia.(15)It has been suggested that scarring alopeciamay be related to secondary infection.(2)Previous studies have addressed the potential relationship between PA and psoriasis(3,4,5,6) as the most common cause(4,5,6)and might be the first clinical manifestation.(2)In this study, it become visible to us that most of the cases (59.21%) showed other clinical manifestations of psoriasis and 10 patients showed histopathological features of psoriasis.Previous reports have suggested that PA is a manifestation of a localized form of seborrheic or atopic(5,6,8,16,17,18) dermatitis. This was similar to the results of this study as 22.36% of the amiantacea patientswas caused by atopic and seborrheic dermatitis. An important consideration in the diagnosis of PA is to rule out the possibility of tineacapitis(5,19) which may have therapeutic implications. As previously demonstrated(5), tineacapitis was one aetiological factor of the eventual diagnosis in the last previous study;(5) the results of this work appeared that tineacapitis found in 10.5% of patients.Bacterial infections was also reported as an independent cause of pityriasisamiantacea.(5) However, bacterial infections in this study found as secondary to the underlying cause of pityriasisamiantacea (e.g. secondarily infected atopic dermatitisor seborrheic dermatitis).
5. Conclusions
- Our study revealed the underlying cause ofpityriasisamiantacea is either psoriasis, seborrheic dermatitis , atopic dermatitis or tineacapitis respectively. Superadded secondary bacterial infection was found mostly in atopic patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML