-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
2012; 1(2): 30-34
doi: 10.5923/j.ajdv.20120102.03
Treatment of Vitiligo with Narrow Band UVB vs.UVB with 0.1% Psoralin; A Case Controlled, Comparative, Therapeutic Trial
Shakir J. Al-Saedy 1, Maytham M. Al-Hilo 1, Dahlia M. AL-Katteb 2
1MBChB, FICMS, DV, Consultant Dermatologist and Venereologist, Al-Kindy Teaching Hospital, Baghdad, Iraq
2MBChB, Al-Kindy Teaching Hospital, Baghdad, Iraq
Correspondence to: Shakir J. Al-Saedy , MBChB, FICMS, DV, Consultant Dermatologist and Venereologist, Al-Kindy Teaching Hospital, Baghdad, Iraq.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This is a case controlled comparative therapeutic trial that conducted in the Beirut Center of dermatology/Baghdad from December 2011 to May 2012 to assess the clinical efficacy of NB-UVB plus topical 0.1% 8-methoxypsoralin in treatment of vitiligo. Sixty-one patients with generalized vitiligo were included in the study with age ranged from 19 to 40 years. The percent of body surface area of vitiligo (BSA-V) ranges from (5-60%) (18 ± 11.6). The response to treatment was evaluated according to a grading system (0, 1, 2, 3, 4).The patients were divided into two groups: group I was exposed to NB-UVB twice weekly till reach 48 sessions with assessment each 16 sessions intervals. Group II was treated with NB-UVB twice weekly with application of 0.1% methoxypsoralin twice weekly before NB-UVB exposure. The duration of treatment was 48 sessions with assessment each 16 sessions interval. In group I, the number of patients who achieved more than 50% reduction in BSA-V was 16 patients (53%): 10 patients reached grade3 and 6(20%) patients reached grade 4, whereas the number of patients who achieved more than 50% reduction in BSA-V was 17(55%) patients: 12(39%) patients reached grade 3 and 5(16%) patients reached grade 4. Group II showed more rapid and effective response than group I. The topical 0.1% methoxypsoralin potentiate the efficacy of NB-UVB in treatment of vitiligo. This combination therapy provided earlier repigmentation and reduced the duration of the treatment.
Keywords: Vitiligo, Photo(Chemo)Therapy, Methoxypsoralin
Cite this paper: Shakir J. Al-Saedy , Maytham M. Al-Hilo , Dahlia M. AL-Katteb , "Treatment of Vitiligo with Narrow Band UVB vs.UVB with 0.1% Psoralin; A Case Controlled, Comparative, Therapeutic Trial", American Journal of Dermatology and Venereology, Vol. 1 No. 2, 2012, pp. 30-34. doi: 10.5923/j.ajdv.20120102.03.
Article Outline
1. Introduction
- Vitiligo is an acquired idiopathic disorder characterized by circumscribed depigmented macules and patches.(1) Vitiligo is the most common depigmentory disorder of the skin and hair resulting from selective destruction of functional melanocytes. It affects all age groups with no predilection for either sex.(2)Though worldwide in the distribution, it is more common in India, Egypt, and other tropical countries. It affects approximately 1–4% of the world population. Patterns of distribution include generalized, acral or acrofacial, localized, and segmental.(3) Several theories include autoimmune, cytotoxic, biochemical, oxidant-antioxidant, neural, and viral mechanisms for destruction of epidermal melanocytes. Several studies also point to a significant role of genetic susceptibility to vitiligo.(4)The treatment of vitiligo is unsatisfactory and in most cases the patient advised to seek effective cosmetic camouflage for the lesions on exposed skin. In sunny climates, the prescription of sunscreens is often necessary.(5)Topical steroid and local immunomodulator therapy are also effective therapy.(6) Skin-bleaching creams 20% monobenzylether of hydroquinone are also of use.(7) Treatment with systemic psoralens,4,5`,8-trimethylpsoralen, 8-methoxypsoralen or 5-methoxypsoralen, combined with exposure to sunlight or to light sources providing high-intensity long-wave UV light, is effective in a proportion of the cases(8,9,10).The patient is instructed to take the psoralens with a dose of 0.6 mg/kg 2 hours before light exposure. Therapy is continued for at least 6 months and in some for several years. In the majority of patients, the areas retain the pigment long after psoralen therapy has been discontinued. Psoralin also been used with UVA.(11)Narrow-band UVB phototherapy has been found to be effective and safe for vitiligo.(12) Narrow-bandUVB is now considered as the gold standard of treatment for vitiligo covering more than 20% of the body. Vitiligo is the most common dermatological diseases treated with photo (chemo) therapy. Phototherapy is the exposure to nonionizing radiation for therapeutic benefits. It involves exposure to ultraviolet A (UVA) or ultraviolet B (UVB).(13) UVB lamps emit either broad band UVB (BB-UVB) or narrow band UVB (NB-UVB). The efficacy of NB-UVB may be enhanced by the addition of psoralen (P-NBUVB). (14)The present work was designed to assess the clinical efficacy of NB-UVB alone in comparison to the combination of NBUVB plus topical 1% 8-Methoxypsoralen in the treatment of vitiligo.
2. Materials and Method
2.1. Patients
- This is a case controlled comparative therapeutic trial done in the Beirut centre of dermatology – Baghdad extending from 1st of December 2011 to end of May 2012. Sixty-one patients with vitiligo were included in the study; 19(32%) males and 42(68%) females. Their ages ranged between 19-40 years with a mean age of 24.54±10.05 years, while the mean disease duration is 8.032±7.092 years. The percentage of body surface area of vitiligo (BSA-V%) ranged from 5-60%with a mean of 18±11.06. All patients had generalized vitiligo. All patients were fully interviewed regarding different medical aspects and examined under clear light. Woods light was used on need to confirm the diagnosis.The inclusion criteria were generalized vitiligo affecting 5% to 60% of the body surface area. Patients had taken treatment for vitiligo within the last 2 months before starting treatment, pregnancy, lactation, renal or hepatic disease, history of photosensitivity and any dermatoses affected by UV light were excluded from the study.Formal consent was taken from each patient before trial after a full explanation about the nature of disease, course and its complications in addition to the method of treatment course, duration, complication of therapy and duration of follow up.The ethical approval was obtained from the ethical committee in Al-kindy teaching hospital.Patients were divided randomly into 2 groups of treatment in which each patient had the chance to be in any group.l. Group I: those patients treated with NB-UVB twice weekly; 30 patients: 9 (30%) males and 21 (70%) females with a mean age of 23.6 ± 5.07 with body surface of vitiligo ranged from 5-60% of a mean 18± 13.75.All patients completed more than 48 sessions and included in the statistical analysis.2. Group II : those patients treated with NB-UVB and topical 8- methoxypsoralin 0.1% twice weekly; 31 patients: 10 (32%) males and 21 (68%) females with a mean age 22. 8± 4 .57 years and body surface area of vitiligo ranged from 5-60%witha mean of 18. 06± 9.8.All 31 patients completed more than 48 sessions and included in the statistical analysis.
2.2. Therapy
- The data of NB:UVB radiation treatment system used were:Kernel (kn-4004 AB) Mainland and lamp pipe Configuration (Philips) is 4×tl 100w/01.Group I: patients were treated twice weekly initially with an irradiation dose of 0.2 J/cm followed by 20% increments at each visit, if tolerated. Doses were adjusted according to the maximum erythema occurring since the previous sessions determined by patient report and by physical examination.Group II: patients were treated twice weekly NB-UVB plus topical 0.1% 8-methoxy psoralen applied 2 hours before exposure to UVB twice weekly in a similar manner to groupI.
2.3. Follow up and Termination of Therapy
- Treatment was terminated if any of the following occurs:1. Complete or almost complete resolution of vitiligo.2. Absence of improvement after 32 sessions or extremely slow progression or deterioration.3. Intolerance of therapy due to local or systemic side effect
2.4. Assessment of Response to Treatment
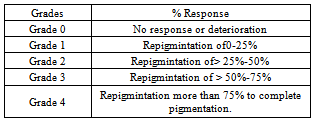
- All patients were assessed before the commencement of treatment and subsequently after every 16 sessions and photographs were taken on each occasion by Cyber-shot Sony digital Camera dsc-T99 (14.1 Mega Pixels) in a good illumination and same place.The surface area of the lesion was calculated using graphic paper for small lesions or use rule of nine and the grading of repigmentation was done as shown in table (1).
|
2.5. Statistical Analysis
- All data arranged and tabulated in number, percentage, mean and standard deviation. All data were coded and entered to the computer by using Microsoft Excel 2010 and Epi-info version 6. Comparison between all groups was done by using analysis of variance.Response to treatment was measured by using paired and unpaired t-test, chi- square test and analysis of variance (ANOVA). Test (p<0.05) was considered as level of significance.
3. Results
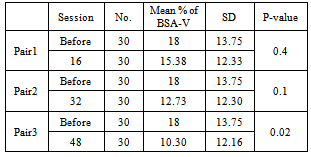
3.1. Group I: (Treatment with Exposure to NB-UVB)
- The results of 30 treated patients were shown in table(2); the mean percent of BSA-V before treatment was l8 ± 13.74. After 16 sessions, it became 15.38 ± 12.33( p-value =0.4); This reduction is statistically insignificant reaching 12.73 ± 12.30 after 32 sessions(p-value =0.1).The mean BSA-V% reached 10.3 ± 12.16 after 48 sessions (p-value=0.02)which is significant. According to the grading system of response after 48 sessions, the following grades were observed: grade I in five patients (17 %), grade II in nine patients (30%), grade III in ten patients (33%) and grade IV in six patients (20%).
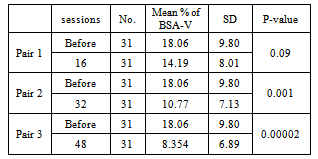
3.2. Group II: (Treatment with Exposure to the NB-UVB Plus Topical Methoxy-Psoralin Solution)
|
|
3.3. Adverse Effects
- Twenty patients (63%) in NB-UVB group and 2l patients (67%) in NB -UVB + 1% 8- methoxypsoralin developed erythema at some stage during their treatment ( p-value=0.08) that is statistically not significant ; no patients treated with 0.1% methoxypsoralin developed erythema. No patients terminate the treatment course because of side effects. No systemic side effects were reported.
4. Discussion
- Vitiligo is an incriminated considerable health problem all over the world. It had a deleterious disfiguring role in the behaviour of the patient.Different modes of treatment have been used to treat the vitiligo like phototherapy, photochemotherapy, immune -modulators, steroid, cosmetics, surgical procedures, and many others. Each has its advantages and limitations. Methoxy psoralin has been used to treat patients with vitiligo as a daily practice; all published studies over the last twenty years proved its effectiveness especially when it is combined with other therapies like UVA. Also methoxy psoralin combined with UV light exposure was recorded to be more effective than methoxypsoralin alone.(15)NB-UVB has been advocated as more applicable than PUVA as it does not need psoralen and it is as effective as PUVA.(16)Narrowband UVB (NB) uses the portion of the UVB spectrum from 311-312 nm. This region has been determined to help stimulate pigment cells to produce melanin in less time than it takes to burn the skin. Any kind of light therapy has a suppressive effect on the immune system, so it can possibly stop new areas from forming as well. NB can be done in the doctor's office with a full-body cabinet or with a doctor's prescription from home using a full-length panel or a handheld device. The handhelds are highly convenient for small areas of vitiligo but are too tedious and cumbersome to use for larger percentages as they cover a very small area at a time. NB is sometimes used in combination with other topical treatments, but is effective for many on its own. NB can be used in children old enough to stand still and keep goggles on.Results are often seen beginning between 30 and 60 treatments, and the treatment is usually given 3 times a week. Potential side effects of NB include burning if used too long. If using a full-body panel or box, the normal skin may tan, increasing the contrast. Only full sized body units provide the immune suppression needed for stabilization that may halt further pigment loss, as the handheld units only treat isolated areas. Eye protection is worn during treatment to protect the eyes, but is not necessary once the treatment is over. (17, 18)Regarding the presented study, the two modalities of treatment were effective in clearance the vitiligo patches, but in group II (the combination therapy) the response was slightly more rapid and more effective than NB-UVB alone. However, the differences in response between the two groups did not reached the level of significance. It has been shown that after 32 sessions, the reduction in BSA-V was statistically significant in both groups (p-value = 0.001). Accordingly, methoxy psoralin may be recommended to potentiate the efficacy of NB-UVB in treatment of vitiligo as it accelerate the resolution of vitiligo patches.To the best of our knowledge, there are few reports about the effect of the combination therapy with psoralin in treatment of vitiligo;similar studies about the use of NB-UVB in vitiligo had shown a satisfactory response.Westerhof and Nieuweboer- Krobotoval 1997 (19)study had shown a repigmentation in 32(63 %) patients with an over 75% of the affected BSA-V who continued with treatment with NB:UVB for 6-12 months. Another study has been done was a retrospective studies; Natta R., Somsak T., Wisuttida T. 2003 (20) mentioned that 33 % of the patients treated with the same modality had repigmentation over 75% of the affected BSA-V.An open trial therapy by Kanwar and Dogra 2005(21), revealed a repigmentation over 75% of the affected BSA-V after one year of treatment in 15 of 20 children treated with this same modality; other trial about UVB effect on vitiligo lesions like El-Mofty 2006, a Left – right comparison study: NB-UVB vs. oral PUVA suggested a repigmentation over 75 % of the affected BSA-V in57 % of the total patients with vitiligo after 60 sessions.(14) Lastly, ParsadD. 2006(22)( aretrospective study), clarified a marked to complete repigmentation in 41.9 % of NB-UVB treated patients of total group of 69 patients with vitiligo.(19,20,16,21) While in generalized vitiligo, PUVA and P-NBUVB had significantly a better results than NB-UVB alone as realized by M. El-Mofty et al,2010.(23) Our study suggests a lower success rate than these previous studies; this may be explained by the difference in study design, patient selection, duration of treatment and no. of sessions done. In addition to the difference in the device used and variations in calibration.(16)
5. Conclusions and Recommendation
- In conclusion, NB-UVB therapy for vitiligo is an effective modality for treatment but it is a need a long course of treatment, while a combination of NB-UVB and 0.1% 8- methoxypsoralenis is more rapid and more efficacious than NBUVB alone .
References
| [1] | Ortonne J-PAUL. Vitiligo and Other Disorders of Hypopigmentation. BologniaJl,Jorrizzo Jl, Rapini; pr. (eds).Dermatology. 2nd Ed.london. Mosby, 2008. |
| [2] | Mosher DB. Fitzpatrick, TB Ortonne, JP Hori; Hypomelanoses and Hypermelanoses. Filzpatrick's Dermatology in General Medicing 5th ed, t999;945-961. McGraw hill medical |
| [3] | Bleehen. SS and Ebling FJG. Disorders of skin color. In Rook A. Wilkinson DS, Ebling FJG, Champion R H, and Burton. Textbook of Dermatology. 6th ed Oxford. Blackwell Scientific Publication. 1998; 18025. |
| [4] | Halder R.M & Taliaferro S. J;vitiligo. In: Wolff K,Goldsith L A, Katz S I, Gichrest B A, Paller A S& Leffell D J. Eds. Fitzpatrick's Dermafology in General Medicine 7th ed.NewYork,McGraw-Hill-Company,2008;616. |
| [5] | Ansty. A. v;disorders of skin colour. In: B. Tony, Breathnach.S,Cox.N. Rook’s Textbookin Dermatology 8th ed. A John Wiley & Sons, Ltd.,publication. 2010;58.46. |
| [6] | Kandil E. Treatment of vitiligo with 0.1% betamethasone 17-valerate in isopropyl alcohol: a double-blind trial. Br J Dermatol 1974; 91: 457–460. |
| [7] | Mosher DB, Parrish JA, Fitzpatrick TB. Monobenzylether of hydroquinone. Br J Dermatol 1977; 97: 669 – 679. |
| [8] | Gawkrodger DJ, Ormerod AD, Shaw L et al. Guideline for the diagnosis and management of vitiligo. Br J Dermatol 2008; 159: 1051–1076. |
| [9] | Parrish JA, Fitzpatrick TB, Shea C et al. Photochemotherapy of vitiligo. ArchDermatol 1976; 112: 1531–1544. |
| [10] | Bleehen SS. Treatment of vitiligo with oral 4,5′,8-trimethylpsoralen (tripsoralen).Br J Dermatol 1972; 86: 54–60. |
| [11] | Ortel B, Tanew A, Hönigsmann H. Treatment of vitiligo with khellin and ultraviolet A. J Am Acad Dermatol 1988; 18: 693–701. |
| [12] | Scherschum L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and welltolerated treatment for vitiligo. J Am Acad Dermatol 2001; 44: 999–1003. |
| [13] | Drake L, Ceilly R, Dorner W, et al. Guidelines of care for phototherapy and photochemotherapy. J Am Acad Dermatol1994: 31 (4): 643–648. |
| [14] | El Mofty M, Mostafa W, Esmat S, et al. Narrow band Ultraviolet B 311 nm in the treatment of vitiligo: two right-left comparison studies. Photodermatol Photoimmunol Photomed2006: 22 (1): 6–11. |
| [15] | Crimes P. Vitiligo an overview of therapeutic approaches .Dermatol clin 1993; ll:325-338 |
| [16] | Younis S.S. Efficacy of PUV therapy vs. NBUVB therapy. ARC Dermatol , 143, May 2007. |
| [17] | Halder RM, Taliaferro SJ, . Vitiligo. In: Wo1ff K, Goldsmith LA, Katz SI, et al. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York. McGraw-Hill Company 2008:72:617-622. |
| [18] | National vitiligo foundation, Inc. newsletter 1990; 2:5. |
| [19] | Westerhof W, Nieuweboer-krobotoval L. Treatment of Vitiligo with UVB radiation vs topical PLIVA. Arch Dermatol1997; 133: 1525-1528. |
| [20] | Natta R, Somask T, Wisuttida L.Narrow-Band ultraviolet B radiation therapy for recalcitrant vitiligo in Asians.J Am Acad Dermatol.2003 sep;49(3):473-476. |
| [21] | Kanwa AJ., Dogra S., Parsad D.,Kumar B. Narrow-band UVB for the treatment of vitiligo: an emerging effective and well-tolerated therapy. Inte J Dermatol 2005; 44; 1:57–60 |
| [22] | Parsad D. Kanwar AJ. Kumar B. PUVA vs NB-UVB for the treatment of vitiligo J Eur Acad Dermatolvenereol 2006;20: 175- 177. |
| [23] | M. El-Mofty,W. Z. Mostafa, M. Bosseila et al. A large scale analytical study on efficacy of different photo(chemo)therapeutic modalities in the treatment of psoriasis, vitiligo and mycosis fungoides .Dermatologic Therapy 2010; 23:428–434. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML