Kaushik Padmanabhan, Sooraj Shetty, Chaiyaporn Mutsalklisana
College of Engineering, Northeastern University, Boston, USA
Correspondence to: Kaushik Padmanabhan, College of Engineering, Northeastern University, Boston, USA.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Atherosclerosis is characterized by the deposition of fat and other residues on their inner walls. This formation is called plaque formation. Over time, plaque hardens and narrows your arterial walls, thus, constricting the blood flow. This limits the flow of oxygen-rich blood to your organs and other parts of your body, which is essential for day to day functioning. One of the possible solutions to avoid the problems caused by Atherosclerosis is the pre-diagnosis of the plaque formation in the inner walls of the arteries. Our solution for it is to detect this plaque formation at a very early stage by placing Micro-SONAR in the suspected area. Application of MEMS technology in healthcare has progressed over years which lead us to use the Micro sized SONAR within the plaque formed artery. This Micro-SONAR would be used for the recurring diagnosis along with blood pressure sensing Nano-sensors which would help to keep track of the plaque formation along with Nano-surgery. Thus, it will help to get a viable solution to overcome the extreme adverse consequences of Atherosclerosis which mainly causes damage to heart with heart attacks by blocking the arteries with plaque.
Keywords:
Ultrasonic Sensor, Micro Electro Mechanical Systems, Nano-robot Actuator System, Nano-surgery, Wireless Monitoring
Cite this paper: Kaushik Padmanabhan, Sooraj Shetty, Chaiyaporn Mutsalklisana, An IoT Aware MEMS Cardio Care, American Journal of Biomedical Engineering, Vol. 6 No. 3, 2016, pp. 86-93. doi: 10.5923/j.ajbe.20160603.03.
1. Introduction
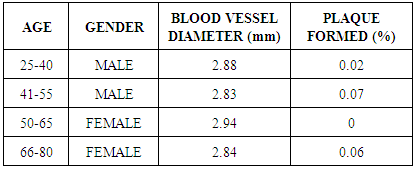
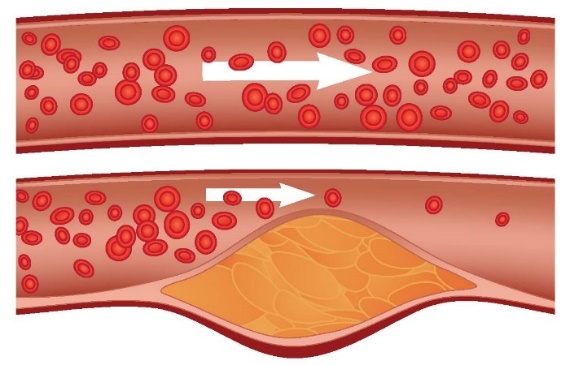
Among the serious diseases faced by human beings Cardio Vascular disease is the prominent one. A Recent survey by American Heart Association depicts that about 17% of the world’s population is suffering from Heart Diseases. Problems involving heart stroke, high blood pressure, angina and rheumatic heart disease comes under the list of these diseases. Coronary heart disease is the main form of heart disease. In common terms, it is known as Heart Disease. Coronary disease is the disorder in the blood vessels of the heart that can lead to heart attack. Heart Attack is characterized by the blockage of the arteries which subsequently prevents oxygen and other healthy nutrients from getting into the heart. Among the various heart diseases, Atherosclerosis is the predominant disease which is particularly characterized by the deposition of the fatty materials on the inner walls of the arteries. This fatty material is often referred as plaque. Atherosclerosis is characterized by the deposition of plaque in the inner walls of the arteries. Arteries are blood vessels which carry the blood to all the parts of our body. The blood carried by arteries is rich in oxygen and other healthy nutrients.Fat, cholesterol, calcium, and other substances found in the blood forms the fatty material, plaque, which restricts the flow of oxygen and other healthy nutrients from getting to the brain and other parts of the body. The problem associated with Atherosclerosis can lead to severe health damages even leading to death. No symptoms have been seen for Atherosclerosis symptoms until middle or older age. But with age the narrowing of arteries become severe and they choke off the flow of nutrient and oxygen rich blood. This choke leads to severe pain. The blockages cause blood clots inside the arteries which may even lead to rupture the arteries at the site of blood clots.  | Figure 1. Atherosclerosis |
The problem of Atherosclerosis progresses with time but the good thing is that there are measures to prevent this serious problem. It can be effectively prevented by avoiding the nine risk factors which are responsible for most of the cardiac arrests and issues. The factors causing these issues involve excessive smoking, very high cholesterol, uncontrolled blood pressure, diabetes, obesity, stress, unhealthy eating habits and inconsistent exercise. Another possible solution to have a control over this problem is the pre-diagnosis of the plaque formation in the inner walls of the arteries. There are many existing practices to perform the pre-diagnosis of plaque formation. These include Doppler tests which make the use of ultrasound or sound waves, Magnetic Resonance Arteriography (MRA), Special CT scans and many other tests like Angiography that uses X-rays to see inside the arteries. Key organs of the body like the heart, brain, kidney, liver, etc. can be viewed with this test. With the existing practices to perform the pre-diagnosis, there are many risk factors associated. These risks include the allergic reaction, bleeding, infection, pain, embolism, impairment of blood vessels, and renal failure. These risks are particular very dangerous for the patients who have weaker kidney functionality and also to the patients suffering from jaundice. To avoid the risks caused by these procedures Nanorobots and micro-sonar can be used for the pre-diagnosis of the plaque formation.Micro-sonar and Nanorobots, which acts as a Sensor- Actuator system, will be placed in the arteries and they will continuously sense for the plaque formation in the inner walls of the arteries. Once the plaque is detected by the micro-sonar, the Nanorobots will head towards the affected area of the artery. These Nanorobots will perform the operations to remove the plaque from the inner walls of the arteries. The position of the Nanorobots can be controlled which will give more precise results. Thus with the use of Nanorobots and micro-sensors, pre-diagnosis of the plaque formation from the arteries can save the individuals from these acute problems and it also reduces the risk factors which are much more susceptible with operations like existing techniques and procedures.
2. Review of Literature
Atherosclerosis, the major cause for the malfunctioning of the heart, referred to as the Myocardial Infarction, is characterized by the formation of plaque within the arterial walls as explained in [1]. Ref [2] deals with one of the existing methods of surface recording of heart muscles, wherein a tiny sensor is used to acquire the acceleration data which is processed by numerical integration to attain the velocity and displacement of the ventricle, which finally tells about the condition of heart. In the meanwhile, plaque formation can occur on the arterial walls which affect the normal functioning of the heart. With reference to the concept in [3], Intra Vascular Ultrasound Image (IVUS) is used to give the cross-sectional images of the arteries with plaque deposition and provides the size of the plaque by extracting the vessel wall and lumen boundaries using contour energy minimization method. The above methods are used only after the cardiac arrest occurs due to atherosclerosis and to remove the plaque that is formed in the arterial walls, an invasive bypass surgery along with the stent insertion is done. A better alternative to the invasive surgical technique is by introducing a minimally invasive surgery provided in [4] which consists of Nanorobots, known as Respirocytes, performing the same surgery with lower risks on the molecular level. This method is commonly known to be a Robotic Surgery. In general, the tiny mechanical systems, known as Nanorobots can be used as a drug delivery system in cancer treatment as explained in [5]. This device generally consists of propellers, cilia, processor and a power source, which is introduced into the body through the femoral artery which is in the thigh region. These Nanorobots can be powered by a radioactive substance, chemical batteries, thermoelectric generators, chemical generators, etc. as given in [6]. In ref [7], a QCA based navigation of Nanorobot is carried out, in which the Nanorobot navigates to the blood clot area by measuring the conductance change in the ZnO Nanowire, which is exerted by means of the high blood pressure within the constricted arteries. This navigation of the tiny device to the coronary artery, in the opposite direction of the blood stream, must know the velocity of blood as addressed in [8]. This includes a blood velocity sensing portion in the Nanorobots as it moves against the blood stream. At present, the Nanorobot surgery is considered to be a one-time surgery where the system is removed from the human body once the operation is done. Hence, it is not used for removing the plaque that can be formed in the near future, by staying within the arteries. In order to constantly detect the plaques and their sizes, that are formed on the arterial walls, an ultrasound device can be used, that is designed as per [12] by applying the piezoelectric body’s field directly on the gate of a field-effect transistor (FET). As explained in [9], the change in the bound surface charge density of the piezoelectric body and the electric field change affects the channel current of a FET, which produces the ultrasound waves. The current system given in [10] deals with the concept of Sensor-Actuator system, wherein an electrode made of MEMS technology is used as a sensor that records the change in Electro Cardio Gram signals from the surface of the heart which in turn sends the signal to the actuator device to release the Aspirin into the blood stream. This helps in preventing the cardiac arrest only after the heart pain occurs.
3. Our Method
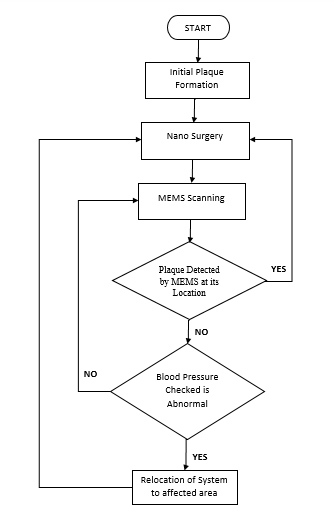
Our method revolves around the concept of using the micro-sized and Nano-sized devices into the human heart for controlling the occurrence of Myocardial Infarction.Fig-2 describes the design flow of our system. The initial plaque formation is the initial phase of the surgery where the first plaque is detected. Nano-surgery is the phase where the Nanorobots start their function of removing the plaque. MEMS scanning is the part where the MEMS unit is scanning the artery for more plaques. Based on the decisions made the system decides whether to relocate or not. 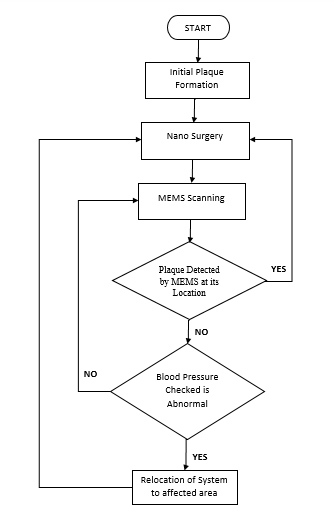 | Figure 2. Flowchart of our method |
A. Navigation of NanorobotsThe process consists of initial navigation of Nanorobots from the femoral artery to the coronary heart. This navigation happens through 7 arteries in between the thigh and the heart region of a human being. The algorithm involves,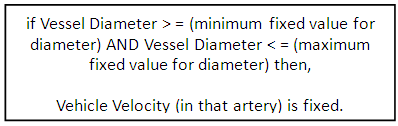 B. Initial SurgeryAfter the Nanorobots reach the coronary artery, the doctor who is technically handling the Nanorobots from outside initially must navigate it to the plaque location in the coronary artery. The navigation to plaque location is done by checking the vessel diameter and Cardiac Output value, so that if there is any reduction in diameter and also an increment in Cardiac Output is found, the existence of plaque in that area is determined easily. The algorithm for this process involves,a. The Blood Pressure is found out from systolic and diastolic values of the pressure recorded.
B. Initial SurgeryAfter the Nanorobots reach the coronary artery, the doctor who is technically handling the Nanorobots from outside initially must navigate it to the plaque location in the coronary artery. The navigation to plaque location is done by checking the vessel diameter and Cardiac Output value, so that if there is any reduction in diameter and also an increment in Cardiac Output is found, the existence of plaque in that area is determined easily. The algorithm for this process involves,a. The Blood Pressure is found out from systolic and diastolic values of the pressure recorded.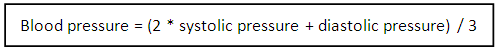 b. The Cardiac Output referred to as the amount of blood that is pumped for every minute of heart beat, is calculated from the blood pressure and the vascular resistance value.
b. The Cardiac Output referred to as the amount of blood that is pumped for every minute of heart beat, is calculated from the blood pressure and the vascular resistance value.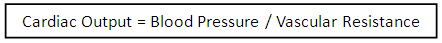 Now the Nanorobots check for the Cardiac Output value and the reduction in diameter of the vessel. If the reduction in diameter is found, the Nano-surgery takes place.
Now the Nanorobots check for the Cardiac Output value and the reduction in diameter of the vessel. If the reduction in diameter is found, the Nano-surgery takes place.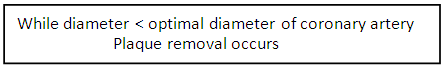 Again the NEMS system will check for cardiac output value so that it confirms whether the block has been removed or not.Fig-3 displays how the Nano surgery start and how it functions. The Nanorobots check all the parameters to verify the existence of plaque in the artery. Once verified, the Nanorobots start performing the surgery.
Again the NEMS system will check for cardiac output value so that it confirms whether the block has been removed or not.Fig-3 displays how the Nano surgery start and how it functions. The Nanorobots check all the parameters to verify the existence of plaque in the artery. Once verified, the Nanorobots start performing the surgery.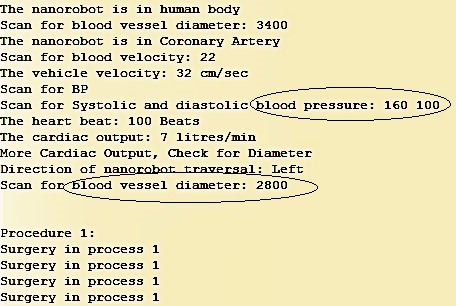 | Figure 3. Nano-surgery process |
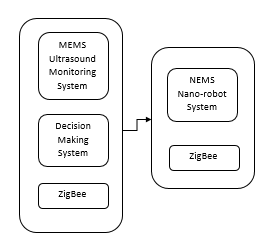
Fig-4 shows the MEMS and the NEMS unit of our system. The MEMS unit is made of the ultrasound monitoring system, which is responsible for the measurement of ultrasound waves. The decision-making system is the evaluation part of our MEMS device which evaluates the Round Trip Times calculated from the MEMS device. The ZigBee is the wireless communicator in the device system which communicates from MEMS to NEMS and vice versa. The NEMS system is made of Nanorobot that possesses the grinding part which is used to grind the plaque and an attaching needle that is used to attach to the walls of the artery. 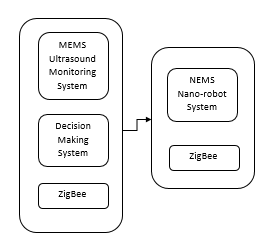 | Figure 4. Block Diagram of MEMS and NEMS unit |
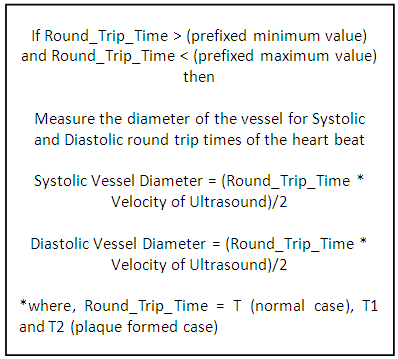
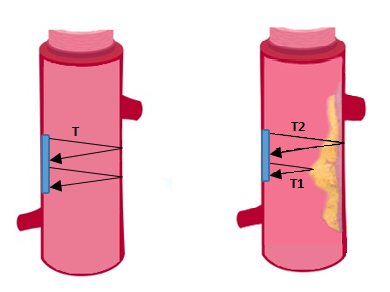
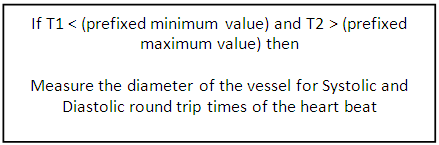
C. Detecting Plaque with Micro-sonarOnce after the Nanorobots removed the plaque, the Nanorobots attach to the walls of the coronary artery where the plaque has been removed and invokes the MEMS device to start its operation. The MEMS device involves a Micro-SONAR, which produces ultrasound waves of prefixed healthcare frequencies inside the coronary artery for measuring the diameter of the blood vessel continuously. The algorithm involves the following steps,Fig-5 shows two cases that clearly explain the concept of atherosclerosis and how our system detects plaque detection. For our system, we have considered time T, which is the Round Trip Time required by the ultrasound waves to get back to the MEMS device. If no delay is observed, (i.e.) when all the waves, that are sent, are received back at the same prefixed Round Trip Time of Micro-SONAR, we can conclude that no plaque has formed. In the second case, as the picture shows, plaque formation has taken place. Here we split T in two part as T1 and T2. T1 is the Round Trip Time required to receive the waves, which reflected without reaching the arterial wall. T2 is the Round Trip Time required to receive the waves, which penetrated the plaque, reached the arterial wall and came back to the MEMS device. The formulae required are as follows.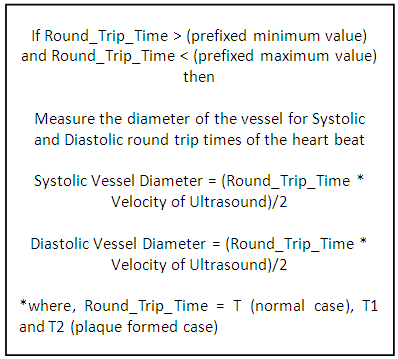
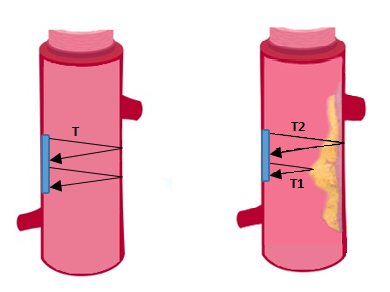 | Figure 5. Pictorial representation of round trip time T, T1 and T2 |
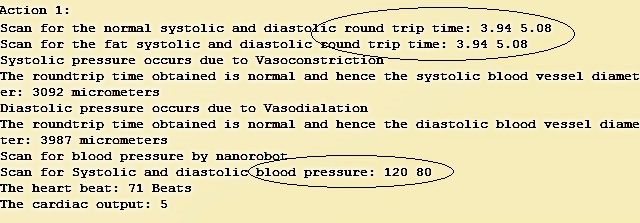
Fig-6 shows both round trip times are same (i.e.) time T, which allows us to deduce that no plaque formation has yet taken place.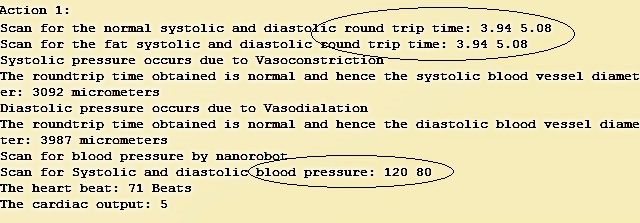 | Figure 6. Diameter calculation by Micro-SONAR |
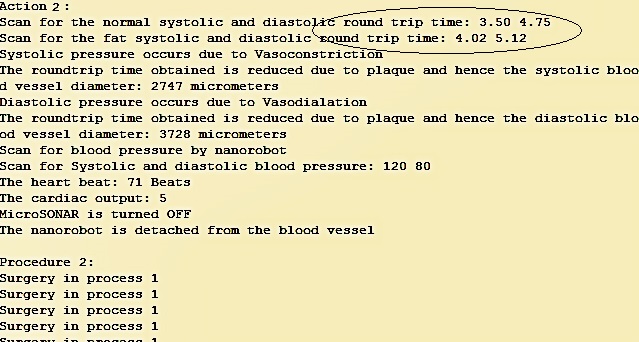
Fig-7 shows both the round trip times are different. The round trip time T1 has reduced and round trip time T2 has increased. This allows us to deduce that plaque formation has taken place.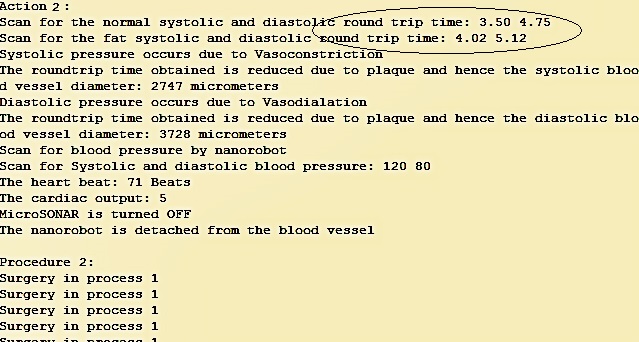 | Figure 7. Detecting the plaque by Micro-SONAR and its removal |
From the diameter and the blood pressure values, the plaque occurrence can fall into two cases.A] CASE STUDY – 1 (PLAQUE FORMED AT THE EXACT LOCATION OF MICRO-SONAR)The plaque can occur at the position where the Micro-SONAR is fixed and this can be found out from the value of the Round Trip Times (T1 and T2).For the plaque formed at the exact location of Micro-SONAR,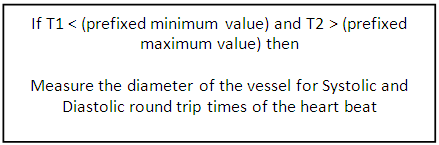 The Nanorobots detach to scrub the plaque formed in that area, after measuring the diameter of the vessel. From the increment in the value of Round Trip Time T2, the existence of plaque is perfectly determined.B] CASE STUDY – 2 (PLAQUE CAN BE FORMED SOMEWHERE ABOVE OR BELOW THE LOCATION OF MICRO-SONAR)Here, if the plaque is formed at a location above or below the micro-sonar position, then the value of the Round Trip Times, will be equal to prefixed Round Trip Time T but the value of the blood pressure recorded will either increase if the plaque is formed at a location above the Micro-SONAR or will decrease if it is formed below.Now the Nanorobot again detaches and navigate left or right depending on the blood pressure values.
The Nanorobots detach to scrub the plaque formed in that area, after measuring the diameter of the vessel. From the increment in the value of Round Trip Time T2, the existence of plaque is perfectly determined.B] CASE STUDY – 2 (PLAQUE CAN BE FORMED SOMEWHERE ABOVE OR BELOW THE LOCATION OF MICRO-SONAR)Here, if the plaque is formed at a location above or below the micro-sonar position, then the value of the Round Trip Times, will be equal to prefixed Round Trip Time T but the value of the blood pressure recorded will either increase if the plaque is formed at a location above the Micro-SONAR or will decrease if it is formed below.Now the Nanorobot again detaches and navigate left or right depending on the blood pressure values.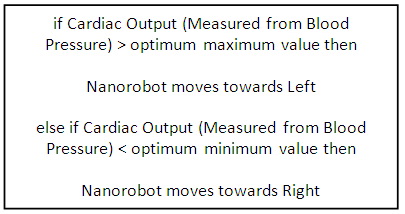 After the direction is chosen, the Nanorobot checks for the reduction in diameter and if the reduction in diameter is found, the Nanorobot undergoes the Nano-surgery which is mentioned in part 1.2 and finally it again attaches to the walls of the coronary artery.Fig-8 shows Nanorobot traversal in the artery based on the location of the new plaque formed, whether on right or left of the current position of Nanorobot.
After the direction is chosen, the Nanorobot checks for the reduction in diameter and if the reduction in diameter is found, the Nanorobot undergoes the Nano-surgery which is mentioned in part 1.2 and finally it again attaches to the walls of the coronary artery.Fig-8 shows Nanorobot traversal in the artery based on the location of the new plaque formed, whether on right or left of the current position of Nanorobot.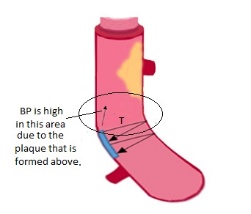 | Figure 8. Traversal of nanorobot to a location above or below the present position of Micro-SONAR |
4. Analysis
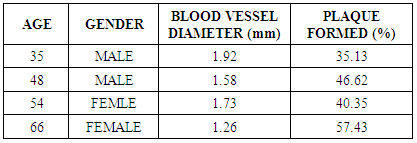
Our proposed solution concentrates mainly on the Coronary Artery, which subdivides into right and left coronary arteries. As per [14], the diameter of the right coronary artery during vasoconstriction is 2.9 +/- 0.5 mm and during vasodilation is 3.8 +/- 0.6 mm. The normal values of blood vessel diameter for different age groups and genders are given below.Table 1. Normal values of Blood Vessel diameter and plaque formed
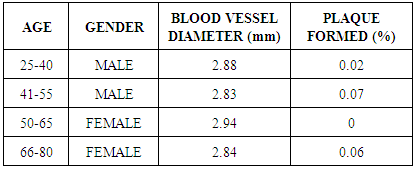 |
| |
|
For our project, we have considered 5 subjects, out of which 4 suffers from cardiac arrest due to atherosclerosis and 1 due to other factor. Table-2 shows the variation in plaque formation in all our patients. It shows that older the patient grows more he or she is prone to plaque formation, as the body is unable to process the fats efficiently.Table 2. Formation of plaque observed in four of our subjects with vessel diameters
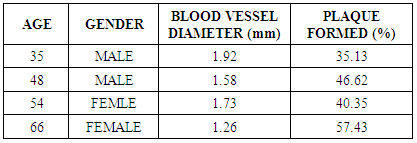 |
| |
|
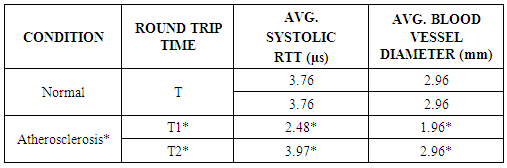
The roundtrip times for the ultrasound with respect to the MEMS unit are presented in the Table-3. In case, no plaque formation has taken place, roundtrip times match. However, that is not the case in case of plaque formation.Table 3. Round trip times T, T1 and T2 are clearly explained in above table
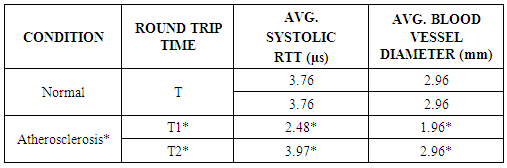 |
| |
|
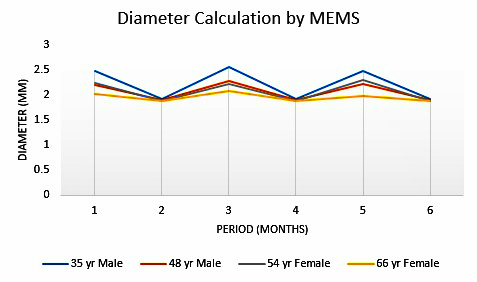
Both the roundtrip times are different for subjects affected by atherosclerosis. Fig-9 shows the calculations performed by the MEMS system which is an essential part of our system. The X-axis is the duration of months. The Y-axis shows the diameter of the blood vessel in mm. We have considered 4 cases, which are highlighted by distinct colors. 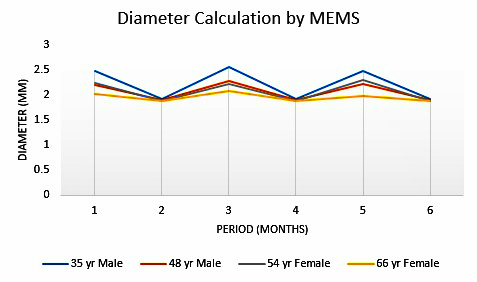 | Figure 9. Graphical representation diameter calculation performed by our system |
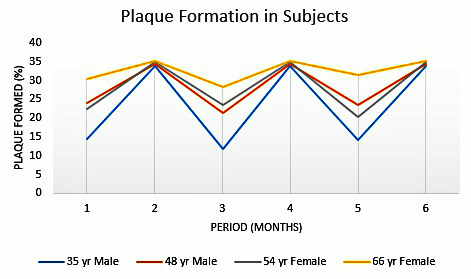
The MEMS system performs the calculation with regards to determining how much plaque is formed in the blood vessel. The MEMS sends out ultrasound waves directed at the artery wall. In an artery free of plaque, transmitted ultrasound wave is reflected back in the correct amount of time. However, in the case of plaque formation, the ultrasound takes a longer time, as the velocity of ultrasound in plaque is reduced. Above graph clearly shows the formation of plaque over a period of time resulting in variation in the values of the available diameter of the free artery. The system kicks into action when the diameter reaches a pre-fixed value depending on age and gender. Then the available diameter comes back to the normal value.Fig-10 shows the plaque formation over a period of time. The X-axis is the duration of months. The Y-axis shows the percentage of the plaque formed in the artery. We have considered 4 cases, which are highlighted by distinct colors.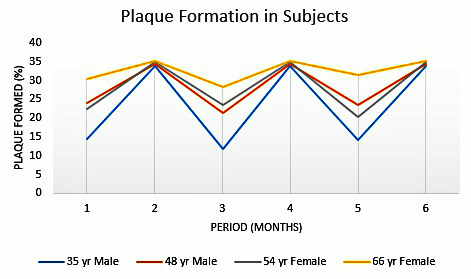 | Figure 10. Graphical representation of plaque formation that takes place in our patients |
The above graph is inferred from the MEMS calculations. We can infer that over the period, plaque formation takes place and our system starts its operation when the vessel diameter is reduced to the pre-fixed value depending on age and gender. After this, the inserted actuator system removes the plaque formed and reduces the plaque percentage in blood vessels. However, this is a cyclic process, as plaque formation is a recurring case, the system starts its process again when the pre-fixed value is reached.
5. Advantages
Our system is one of a kind system where detection and removal of plaque are done by the same system. The various advantages of our system are as follows:Ÿ Continuous removal of plaque – Our system constantly checks for plaque in the coronary artery, with the help of its MEMS unit and removal with its NEMS unit. Thus, plaque removal is done constantly. This avoids built up of stronger plaques, which are harder to remove.Ÿ Fast detection of plaque – The MEMS unit detects plaque at a phenomenal rate, given the fact formation if plaque is an extremely gradual process. Faster detection enables the system to stay two steps ahead and allow in maintaining cleaner arteries.Ÿ No side-effects – The system is intact, hence issues arising from chemical discharge is not possible. Also, the system performs in such a way, that no harm is caused to the human body.Ÿ Site-specific operation – The system is programmed to operate in a fixed area, in this case, the coronary artery. This enables us to constantly monitor the system successfully. Also, side tracking of the system does not occur.Ÿ Minimally invasive surgery – The surgery to insert the system is a minimally invasive surgery, where the system is inserted into the femoral artery, to navigate all the way to the coronary artery. The surgery while being minimally invasive also saves a lot of time.Ÿ Fast and accurate results – Results from our system are extremely accurate, as our system takes into consideration lot of factors which enables us to get these results. Also, the system is very fast in producing results.These advantages enable our system to be the top of the line system designed for to solve this problem.
6. Future Scope
Resembling any current modern technology, our system also allows plenty of new modernizations and developments to be done. The system we have designed is a stepping stone to venture in this field. Some of the future scopes of the project are as follows:Ÿ System biocompatibility – The human body releases antibodies to fight foreign agents inside the body. The system which we introduce inside the body is recognized as a foreign body. The human body will react as it is designed to do and attack the system. This hampers the progress of the system and thus affecting its work. If the system is made biocompatible, it will surely overcome this problem.Ÿ Electrical Impedance Spectroscopy – Detection of plaque can also be done by Electrical Impedance Spectroscopy. Here, the intensity of the plaque is also detected, allowing us to know beforehand how to go about the removal of plaque.These factors must be considered in the scenario our system needs betterment. Consideration of these factors will enable us to design more advanced systems.
7. Conclusions
Our system, which is a one of a kind, treats atherosclerosis taking into consideration the innumerable variations that come up in treating one person to another. As atherosclerosis is one of the leading factors affecting our up and coming generation, the need for such a system is extremely essential. By far, this is the most advanced technique implemented in this field.
ACKNOWLEDGEMENTS
We wish to acknowledge each and everyone who played a major or minor part which resulted in the creation of this paper. Among all the helpful people, we would especially like to thank our Teaching Assistants, Mushtaq Rizvi, Atul Nipane and Shreya Jain. We would like to thank our Research Assistant, Kishore Mohan. And last but not the least we would like to thank our professor, Chaiyaporn Mutsalklisana, who guided us throughout the entire project, in each and every way possible.
References
| [1] | E. Falk, “The Formation, Fate and Clinical Consequences of Atherosclerotic plaque”, Dept. of Cardiology, Aarhus University Hospital, Denmark, May 1999. |
| [2] | Fjodors Tjulkins, Anh Tuan Thai Nguyen, Nils Hoivik, Knut E. Aasmundtveit, Erik Andreassen, Lars Hoff, Kristin Imenes, “3-Axis MEMS Accelerometer-based Implantable Heart Monitoring System with Novel Fixation Method”, IEEE Electronic Components & Technology Conference, 2013, pp.510 -516. |
| [3] | Sridevi S, Sundaresan M, “A new approach for coronary plaque layer analysis based on IVUS”, International Conference on Computing for Sustainable Global Development, 2014, pp.490-494. |
| [4] | Lukeman Hakkim S, Ranjitha A, “Replacement of heart bypass surgery using Nanorobots: a review”, International Journal of Novel Research in Engineering and Science, Vol. 2, Issue 2, September 2015, pp. 7-12. |
| [5] | Leslie Rubinstein, “A Practical Nanorobot for Treatment of Various Medical Problems”, Eighth Foresight Conference on Molecular Nanotechnology, pp. 1-12. |
| [6] | Kailash Chandra Mishra, “A review on supply of power to Nanorobots used in nanomedicine”, International Journal of Advances in Engineering & Technology, Vol. 4, Issue 2, September 2012, pp. 564-571. |
| [7] | Suraj H, Vivekavardhana Reddy B, “QCA Based Navigation for Nano Robot for the Treatment of Coronary Artery Disease”, IEEE. |
| [8] | Matthieu Fruchard, Laurent Arcese, and Estelle Courtial, “Estimation of the Blood Velocity for Nanorobotics”, VOL. 30, NO. 1, FEBRUARY 2014, pp.93-102. |
| [9] | Min Sung, Kumjae Shin, and Wonkyu Moon, “A micro-machined hydrophone using piezoelectricity on gate of a field-effect transistor”, IEEE Transducers 2015, June 2015, pp.379-382. |
| [10] | Prittopaul P, Sathya S, Jayasree K, “Cyber Physical System Approach for Heart Attack Detection and Control Using Wireless Monitoring and Actuation System”, IEEE Sponsored 9th International Conference on Intelligent Systems and Control (ISCO), 2015. |
| [11] | Xiaoxiao Zhang, Lei Xu, Juhyun Lee, Rongsong Li, Yang Liu, Aubrey Shapero, Tzung Hsiai, Yu-Chong Tai, “Flexible Micro Sensor for Intravascular Vulnerable Plaque Diagnostic with Electrical Impedance Spectroscopy”, 10th IEEE International Conference on Nano/Micro Engineered and Molecular Systems (IEEE-NEMS 2015), April 2015, pp. 243-247. |
| [12] | Anh-Tuan T. Nguyen, Fjodors Tjulkins, Knut E. Aasmundtveit, Nils Hoivik, Lars Hoff, Kristin Imenes, “Miniaturization of Package for an Implantable Heart Monitoring Device”, DTIP 2013, April 2013. |
| [13] | Yuan Luo, Xiaoxiao Zhang, Rene Packard, Rongsong Li, Tzung Hsiai, Yang Liu, “In-vivo intravascular intervention with parylene microelectrode to diagnose rupture-prone atherosclerotic plaque using electrical impedance spectroscopy”, IEEE MEMS 2016, January 2016, pp. 307-310. |
| [14] | J. Theodore Dodge Jr., MD; B. Greg Brown, MD, PhD; Edward L. Bolson, MS; and Harold T. Dodge, MD, “Lumen Diameter of Normal Human Coronary Arteries Influence of Age, Sex, Anatomic Variation, and Left Ventricular Hypertrophy or Dilation”, American Heart Association , July 1, 1992, Volume 86, Issue 1. |



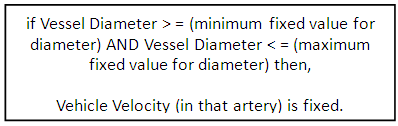 B. Initial SurgeryAfter the Nanorobots reach the coronary artery, the doctor who is technically handling the Nanorobots from outside initially must navigate it to the plaque location in the coronary artery. The navigation to plaque location is done by checking the vessel diameter and Cardiac Output value, so that if there is any reduction in diameter and also an increment in Cardiac Output is found, the existence of plaque in that area is determined easily. The algorithm for this process involves,a. The Blood Pressure is found out from systolic and diastolic values of the pressure recorded.
B. Initial SurgeryAfter the Nanorobots reach the coronary artery, the doctor who is technically handling the Nanorobots from outside initially must navigate it to the plaque location in the coronary artery. The navigation to plaque location is done by checking the vessel diameter and Cardiac Output value, so that if there is any reduction in diameter and also an increment in Cardiac Output is found, the existence of plaque in that area is determined easily. The algorithm for this process involves,a. The Blood Pressure is found out from systolic and diastolic values of the pressure recorded.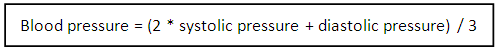 b. The Cardiac Output referred to as the amount of blood that is pumped for every minute of heart beat, is calculated from the blood pressure and the vascular resistance value.
b. The Cardiac Output referred to as the amount of blood that is pumped for every minute of heart beat, is calculated from the blood pressure and the vascular resistance value.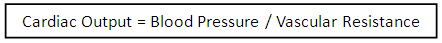 Now the Nanorobots check for the Cardiac Output value and the reduction in diameter of the vessel. If the reduction in diameter is found, the Nano-surgery takes place.
Now the Nanorobots check for the Cardiac Output value and the reduction in diameter of the vessel. If the reduction in diameter is found, the Nano-surgery takes place.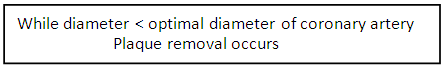 Again the NEMS system will check for cardiac output value so that it confirms whether the block has been removed or not.Fig-3 displays how the Nano surgery start and how it functions. The Nanorobots check all the parameters to verify the existence of plaque in the artery. Once verified, the Nanorobots start performing the surgery.
Again the NEMS system will check for cardiac output value so that it confirms whether the block has been removed or not.Fig-3 displays how the Nano surgery start and how it functions. The Nanorobots check all the parameters to verify the existence of plaque in the artery. Once verified, the Nanorobots start performing the surgery.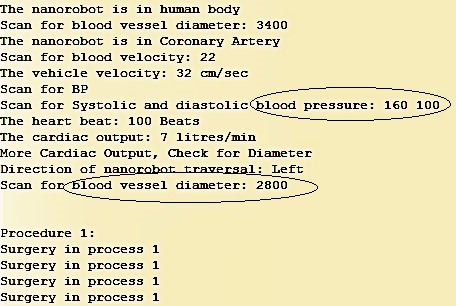
 The Nanorobots detach to scrub the plaque formed in that area, after measuring the diameter of the vessel. From the increment in the value of Round Trip Time T2, the existence of plaque is perfectly determined.B] CASE STUDY – 2 (PLAQUE CAN BE FORMED SOMEWHERE ABOVE OR BELOW THE LOCATION OF MICRO-SONAR)Here, if the plaque is formed at a location above or below the micro-sonar position, then the value of the Round Trip Times, will be equal to prefixed Round Trip Time T but the value of the blood pressure recorded will either increase if the plaque is formed at a location above the Micro-SONAR or will decrease if it is formed below.Now the Nanorobot again detaches and navigate left or right depending on the blood pressure values.
The Nanorobots detach to scrub the plaque formed in that area, after measuring the diameter of the vessel. From the increment in the value of Round Trip Time T2, the existence of plaque is perfectly determined.B] CASE STUDY – 2 (PLAQUE CAN BE FORMED SOMEWHERE ABOVE OR BELOW THE LOCATION OF MICRO-SONAR)Here, if the plaque is formed at a location above or below the micro-sonar position, then the value of the Round Trip Times, will be equal to prefixed Round Trip Time T but the value of the blood pressure recorded will either increase if the plaque is formed at a location above the Micro-SONAR or will decrease if it is formed below.Now the Nanorobot again detaches and navigate left or right depending on the blood pressure values.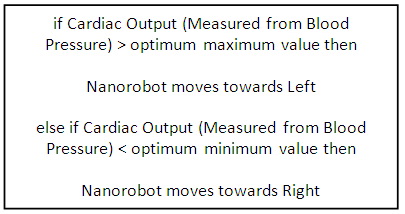 After the direction is chosen, the Nanorobot checks for the reduction in diameter and if the reduction in diameter is found, the Nanorobot undergoes the Nano-surgery which is mentioned in part 1.2 and finally it again attaches to the walls of the coronary artery.Fig-8 shows Nanorobot traversal in the artery based on the location of the new plaque formed, whether on right or left of the current position of Nanorobot.
After the direction is chosen, the Nanorobot checks for the reduction in diameter and if the reduction in diameter is found, the Nanorobot undergoes the Nano-surgery which is mentioned in part 1.2 and finally it again attaches to the walls of the coronary artery.Fig-8 shows Nanorobot traversal in the artery based on the location of the new plaque formed, whether on right or left of the current position of Nanorobot.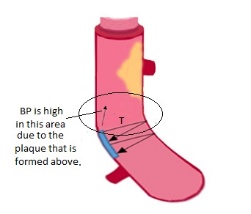
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML