-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biomedical Engineering
p-ISSN: 2163-1050 e-ISSN: 2163-1077
2014; 4(4): 73-78
doi:10.5923/j.ajbe.20140404.01
The Functions of Electrical Activity of the Heart
Bill Wenling Zheng1, Wenli Ma1, Wan-Ching Ho2
1Southern Medical University, Institute of Genetic Engineering, Guangzhou, China
2Retired Electronic Engineer, Hong Kong, China
Correspondence to: Wan-Ching Ho, Retired Electronic Engineer, Hong Kong, China.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Many reports in the literature have separately discussed the operation and analysis of cell membrane potential and of electrical activity of the heart. More studies have provided detailed, in-depth explanations on the former, while fewer have been written on the latter. There has even been no generally accepted name for “electrical activity of the heart,” so we refer to it here as Cardio-emf. As we all know, the liver is located beside the heart, and both organs are connected through blood that has high electrical conductivity. From the point of view of an electrical circuit, the membrane potential of the liver cells and the Cardio-emf are electrically connected, or it can be said that both are in the same circuit. Therefore, to say there is no mutual effect between them would completely overturn the theories on circuits and electronics. This manuscript demonstrated and proved that the Cardiac electrical activity (cardio-emf) could influence directly the movement of the liver cells in synchronized manner so absorption and secretion from the liver cells would be in phase. By extrapolation of such an analysis, novel functions of the cardio-emf has been discovered.
Keywords: Cardio-emf, Coulomb's Law, Membrane-emf, Capacitor, ECF&ICF
Cite this paper: Bill Wenling Zheng, Wenli Ma, Wan-Ching Ho, The Functions of Electrical Activity of the Heart, American Journal of Biomedical Engineering, Vol. 4 No. 4, 2014, pp. 73-78. doi: 10.5923/j.ajbe.20140404.01.
Article Outline
- Knowledge on the cardiac electrical activity could be dated back more than 160 years ago. Form the work of Dr. Augustus Waller, he proposed the ways to monitor the electricity of the heart and he was widely recognized as the father of electrocardiography(ECG),which is the milestone in advancing the diagnosis of the heart diseases.In 1995, Dr. Bill Zheng and Dr. W. Ma have suggested a hypothesis about the cardiac electrical activity may control the liver cells to absorb and secrete through their membrane voltage. In 2014, the hypothesis, which may lead to research development that save thousands of lives, have been proven by Dr. Zheng and Dr. Ma with assistance from an Experienced Electronic Engineer.Full text of the manuscript will be presented as follow.Coulomb’s law is the foundation for electricity, and therefore, we try to employ it to investigate the electrical mechanisms of the electrical activity of the heart [2].
1. The Cardio-emf or the Electrical Activity of the Heart
- The main function of Cardio-emf is to make the heart muscles contract so as to keep blood flowing. Aside from this, could there be other unidentified functions?To be concrete, we use the liver as a model organ to explain how Cardio-emf may impact liver function, and we assume that the liver cannot function without Cardio-emf, so the factors should be considered as follows.A) To reduce the power lost on transmission, the path of the current must be as short as possible, so the model organ will be close to the heart.B) Aside from having a short distance, a material with high electrical conductivity, or with low resistance, is also very important to decrease the power loss. As is generally known, blood is the substance in the human body with least resistance, so the model organ must be the organ with the highest amount of blood influx.C) Since the supposed model organ must rely on Cardio-emf, therefore the model organ will cease activity when heart failure occurs.D) Cardio-emf is available 24 hours a day, so the model organ must work 24 hours a day.To meet the above four conditions, it is necessary to use the liver as the model organ.Before exploring how Cardio-emf controls the operation of liver cells, it is necessary to study the electrical characteristic of the cell membranes.
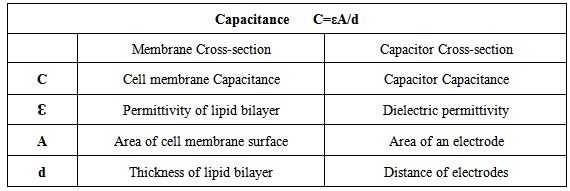
2. Cell Membrane and Capacitor Analysis
- First of all, we should discuss the structure of the cell membrane from the perspective of an electrical device. As shown in the sectional view in Figure 1, the cell membrane has a structure that is almost identical to that of a capacitor (on the right), and the only difference is that the two electrodes of the “cell membrane capacitor” are the liquid extracellular fluid (ECF) and the intracellular fluid (ICF). As for the dielectric, the lipid bilayer is made of an organic solid, which is always associated with ultra high electrical resistance (for lipid bilayer=100GΩ). Therefore, the capacitance can be expressed using the following formula.
|
3. Think Positive – Charge
- Theory, positive charge = proton.Every positive charge inside human body may be regarded to be an atom, a molecule, etc. that has lost a free electron. An electron has a negative charge, and its diameter is only 1/100,000 that of a hydrogen atom. Given their extremely small sizes, the impact of the mass of the electrons are entirely negligible since they will never lead to motion of the materials.Therefore, we can draw the conclusion that:• A positive charge = atom (-e) = molecule (-e) = substanceAs a result, positive charges are the main factor to consider that cause physical movement, deformations, and so on.
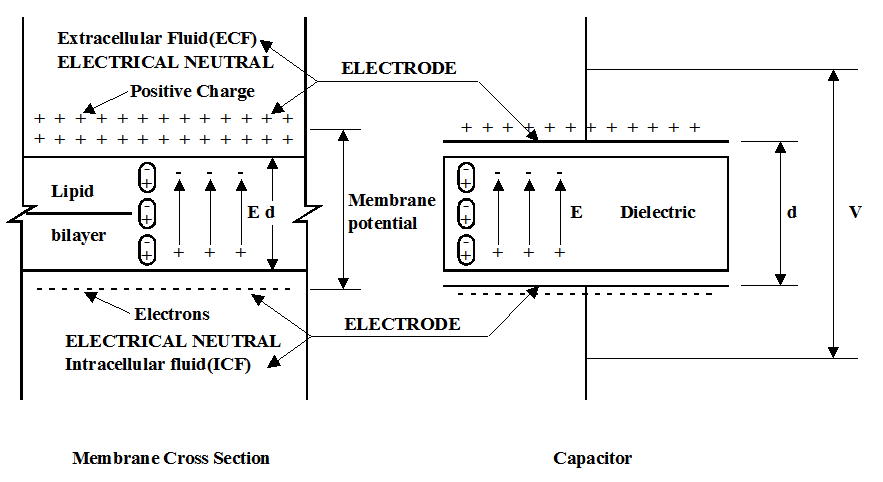
4. Analysis of Electric Current Flows through a Conductor
- Electric current = the flow of a positive charge.Electron flow = opposite to the electric current’s direction, which is the real flow of the electrons. Therefore, inside a normal circuit, only electrons actually move.Figure 2: Current I, flows through a conductor R from top to bottom, and the potential slowly decreases, which observed as Va>Vb>Vc>Vd. This is one of the main phenomena explained through Kirchhoff’s voltage law [1].
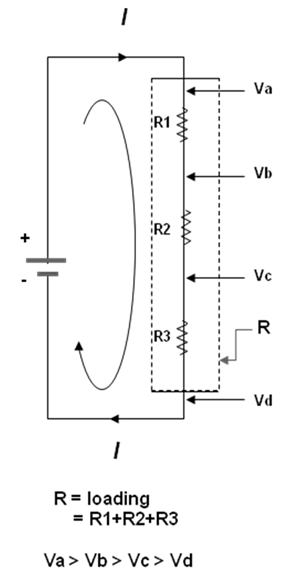 | Figure 2. Voltage drop inside the conductor R |
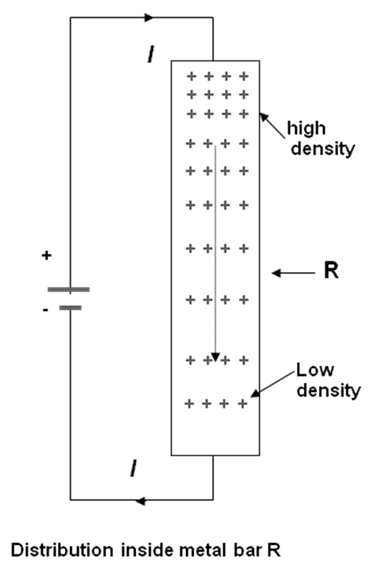 | Figure 3. Distribution of positive charges inside conductor R |
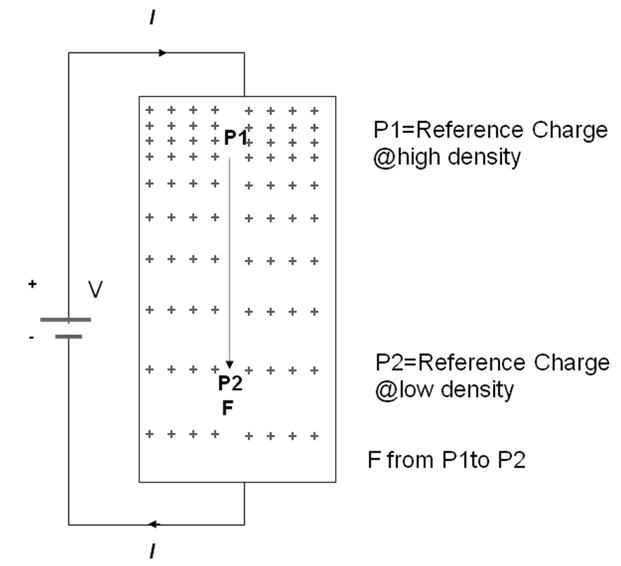 | Figure 4. Set a positive charge as a reference between the high low densities |
5. How does Cardio-emf Make Liver Cells Absorb and Secrete
- After having understood the electrical principles of the system, it is very easy for us to explain how hepatocytes operate. For ease of explanation, the present function can be simplified according to the following diagram.Figure 5: Since the outer positive charges on the cell membrane are free charges, they can generate an electric field due to the Coulomb force, as shown in the diagram. (The lines are drawn in such direction, and we call these the electric force or Coulomb force lines.) Where will the electric force lines, just like arrows, extend to? Of course the destination is the cathode of the Cardio-emf, which is created by the activity of the cardiomyocytes. At the moment of a pulse, the cathode is the place that contains the most free electrons, and it is nearest to the liver in human body and is connected with blood. So all of the electric force lines emitted from the free positive charges on the hepatocytes have no other choice but to be oriented toward the cathode as per Coulomb's Law. Per our roughly calculations (assume: ε of blood = ε of ECF & ICF), the Coulomb attractive force for the free positive charges on the outer membrane toward the cathode is 1.6×104 times that toward the negative charges of the inner membrane. If the estimate for cathode is of 1.8×1017e or 0.03 Coulomb, then r = 0.1m. If the estimate for membrane free charges is of 1×106e or1.6×10-13 Coulomb, then r = 30 μm. After the electric force lines connect (electrically turn on), electrons will rush to all hepatocytes with an electricity or electric field speed of 0.96 c. (For reference, this is the speed of electricity in a bare copper wire, and c = the speed of light). It makes no sense to discuss which electron arrives faster because the distance is too short and the speed is too fast. So we can suppose that all electrons have arrived at the same time, and we just present another drawing of the cell to explain the situation.
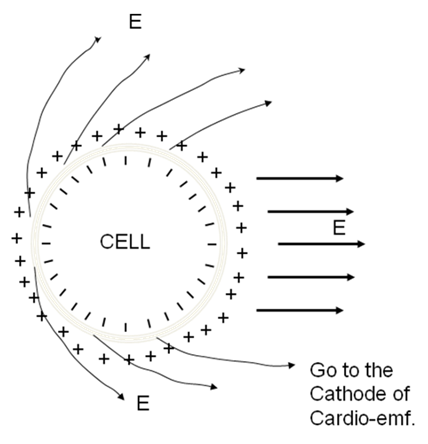 | Figure 5. Demonstrated a single liver cell generates a electric field due to the Coulomb force from the cathode of cardio-emf |
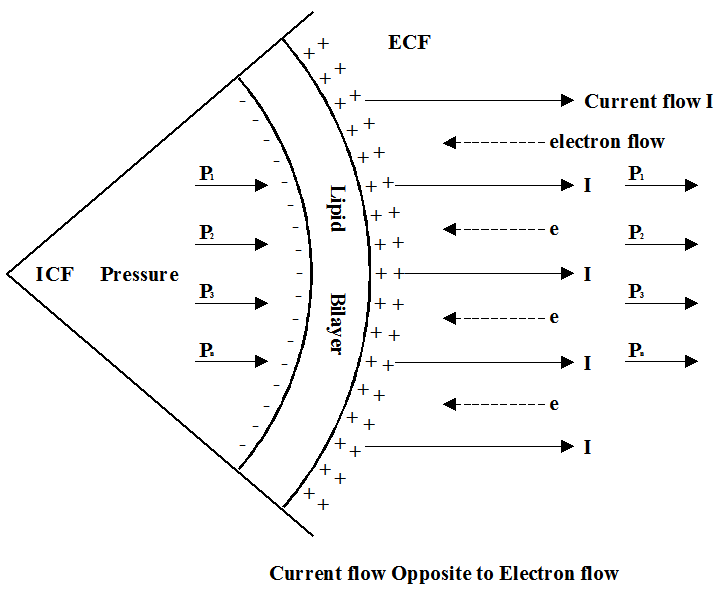 | Figure 6. Current Flow cause the cell expand |
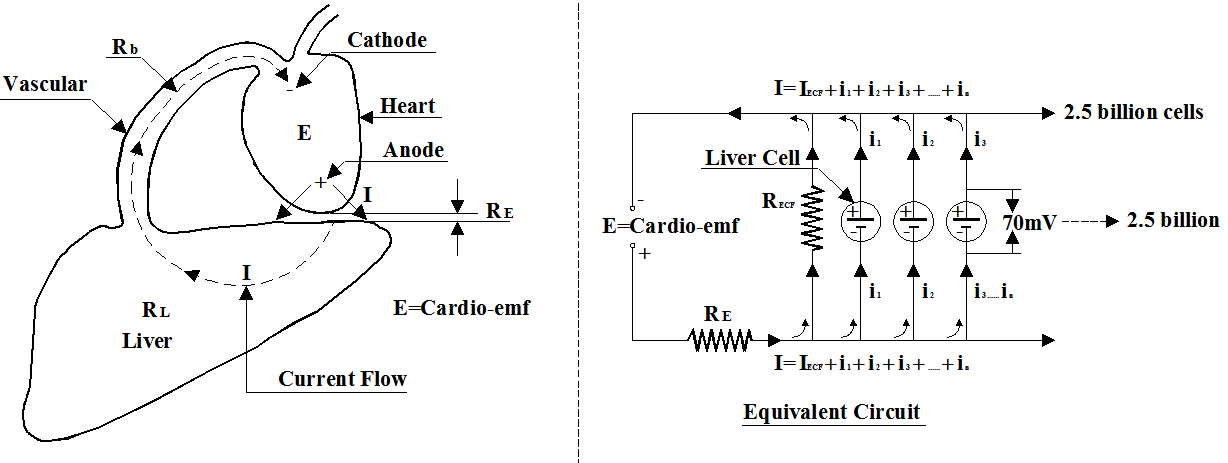 | Figure 7. Electrical equivalent circuit of the cardio-emf and the liver organ |
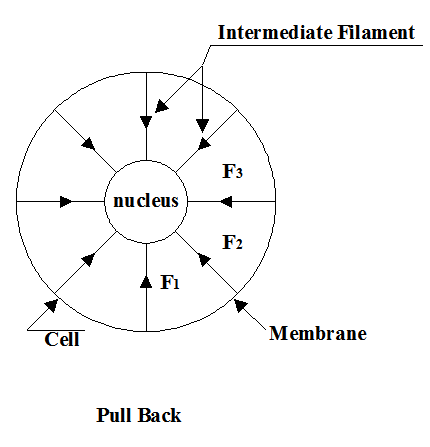 | Figure 8. The connection between the membrane and the nucleus is responsible to pull back the cellular volume back to normal, as in the process of secretion |
6. Conclusions
- 1) As is commonly known, the main function of Cardio-emf is to make the heart contract so as to keep blood flowing. Besides this, the second function is to drive the liver cells, working in phase, in order to increase the efficiency of the organ. Otherwise, many cells may only absorb secreted materials from their neighbors, if a pair of cells absorb and secrete in opposite phases (kiss effects).2) As far as we know, the main function of the cell membrane-emf is to make the cell expand, so as to absorb and to secrete substances.3) In the past thirty years, all clinical trials on artificial heart are not very successful, the cause of failure might be due to lack of the Cardio-emf pulsing system that should be built into the artificial heart. Therefore, the traditional artificial heart could not be fully functioned as a real heart. In contrast, the features of artificial joint design was designed to be very close to the real joint hence the successful rate of artificial joint transplant or replacement is substantially higher. It is estimated that at least 1500 people died in the United States every year because of the shortage of the suitable and transplantable heart. Redesign of the artificial heart which is associated with the built-in system of Cardio-emf could potentially result in saving thousands of lives every year.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML