-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biomedical Engineering
p-ISSN: 2163-1050 e-ISSN: 2163-1077
2012; 2(3): 105-114
doi: 10.5923/j.ajbe.20120203.03
Marginal Adaptation of Nanofilled, Packable and Hybrid Dental Composite Resins Stored in Artificial Saliva
Mohamed El-Nawawy1, Lubna Koraitim1, Ossama Abouelatta2, Hanan Hegazi1
1Conservative Dentistry Dept., Faculty of Dentistry, Mansoura University, 35516 Mansoura, Egypt
2Production Engineering and Mechanical Design Dept., Faculty of Engineering, Mansoura University, 35516 Mansoura, Egypt
Correspondence to: Ossama Abouelatta, Production Engineering and Mechanical Design Dept., Faculty of Engineering, Mansoura University, 35516 Mansoura, Egypt.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Resin based composites are possibly the most universal material available in dentistry as they are used in a huge variety of clinical applications, ranging from filling material, luting agent, indirect restorations and metal facing for endodontic posts and cores. The growth of bacteria on the composite resin surfaces, secondary caries and pulp damage or marginal imperfections may occur at the site of gap formation. In this study, marginal adaptation of three composites were measured and compared. A total of sixty human mandibular first molars were used. The teeth were divided into three main groups (20 teeth each) according to the composite resins that were used. In group I, Surefil (packable composite) was used as the restorative material. In group II, Esthet-X-improved (nanofilled composite) was used, while in group III Glacier (hybrid composite) was used. Each group was subdivided into four subgroups (five teeth each) according to the storage intervals (24 hours, one week, two weeks, and three weeks). In each group, occlusomesial cavities were prepared with diamond burs and restored with the composite, according to manufacturer's instructions. In all specimens, composite was applied to the cavity using incremental technique. All the restored teeth were subjected to in vitro thermal cycling and mechanical loading simulating a total of six months in vivo function. Marginal adaptation was evaluated using Measurescope-10 and the results were confirmed with scanning electron microscope. These specimens were dried, sputter coated with gold-palladium and then photographed with SEM at 1500x. A highly significant difference in marginal adaptation was found between the used composites. After specimen storage in artificial saliva, there was a gradual improvement in the marginal adaptability of the specimens. It can be concluded that the marginal adaptation of the nanofilled composite was the best when compared to the other composites.
Keywords: Marginal Adaptation,Nanofilled,Packable,Hybrid,Composite Resins
Article Outline
1. Introduction
- The evolutionary development of filling materials leads to an ever increasing need for better tooth colored restorative materials to replace missing tooth structure and to modify tooth color and contour, thus enhance facial esthetics. Polymeric restoratives have continued to evolve into the direct restorative materials of choice mainly because of their superior aesthetic characteristics. Currently, composites are the most widely used materials in restorative dentistry[1]. Polymerization shrinkage remains a challenge and still imposes limitation in the application of direct techniques. Dental composites exhibit inherent problem of 2-4% volumetric shrinkage during polymerization process[2]. Stress arising from polymerization shrinkage can result in bond failure and has been shown to have greater effect on marginal gap formation than bond strength. A gap free direct composite restoration is possible only if the adhesive forces to the tooth overcome the interfacial stress generated during curing and afterward[3].In fact, previous studies indicate that chemical toxic leachants from restorative materials are less significant in causing pulpal injury than bacteria leakage arising from polymerization shrinkage around the restoration margins in posterior teeth[2,4]. The supreme test of dental restorative filling is its ability to maintain unfailing margins; a microscopic space tends to exist between the restoration and the prepared cavity which results in passage of saliva. Incomplete marginal sealing at tooth/restoration interface is found to result in post placement sensitivity, marginal staining, recurrent caries and eventually the development of pulp pathology[5].A composite, as the name implies, consists of a mixture of two or more materials. Each of these materials contributes to the overall properties of the composite. Composites are classified by particle size as macrofill (10-100µm), midifill (1-10µm), minifill (0.1-1µm), microfill (0.01-0.1µm) and nanofill (0.005-0.01µm). Composites with mixed ranges of particle sizes are called hybrids, and the largest particle size range is used to define the hybrid type (e.g. minifill hybrid composite)[6,7].Nanocomposites are a very promising new class of polymer composites that exhibit an interesting combination of chemical, physical and mechanical properties. Only small amounts of nanofiller are sufficient to generate great variation of many properties. Therefore, many researchers studied the effect of nanofillers to compare the inorganic fraction and the mechanical properties[8], to assess and to correlate wear and surface roughness of minifilled and nanofilled composites finished and polished by different methods[9], to determine the changes in gloss of composite resins after generalized wear simulation[10], to investigate friction and wear properties[11], to characterize the surface properties of some modern resin composites employing a series of physicochemical methods[12], and to investigate the mechanical properties of experimental composites and an unfilled ones[13]. In addition, others concluded that the stress resulted from the placement of dental composite in a confined setting compromises the integrity of the marginal seal[14]. Others compared the enamel and dentin bond strengths of a new nanofilled one-coat adhesive system with its predecessor to analyze the dentin interfacial ultramorphology[15]. An in vitro study was done to determine the distribution of nanofillersfrom a simplified-step adhesive in acid-condi- tionedwithin the collagen network of the hybrid layer[16]. The effects of nanofiller surface treatment and resin viscosity on the early and long-term properties of experimental hybrid composites were also evaluated[17]. The clinical performance of a nanofill and a nanohybrid composite in restorations in occlusal cavities of posterior teeth in a randomized trial over 30 months was evaluated by Andrade et al.[18]. The materials investigated showed acceptable clinical performance and showed a significant differences in the marginal adaptation. Takahashi et al.[19] investigated the effects of polymerization contraction, shrinkage stress and Young’s modulus of nanofiller containing resin composites on early marginal adaptation of restorations in cavities.Marginal cavity adaptation of restorations in bonded dentin cavities reflects complex interactions between adhesive bonding on the one hand, and polymerization contraction strain, stress and elastic modulus, on the other.Marginal adaptation was defined as the interfacial distance between the eluted restoration and the tooth structure, excellent marginal adaptation depends on the quality of the composite restorations and adhesive systems. The growth of bacteria on the composite resin surfaces, secondary caries and pulp damage or marginal imperfections may occur at the site of gap formation[20]. The origin of marginal leakage is very complex because of the numerous factors contributing to it, polymerization of composite resins produces shrinkage and subsequent water sorption does produce expansions, other factors like coefficient of thermal expansion and marginal adaptation contribute as well[21]. The bond strength of most composite resins is less than the concentration forces, this causes a space that developed between the restoration and enamel wall. This undesirable space or gap can be expected and frequently detected on the proximal gingival margins of class II restorations[22]. Thonemann et al.[23] studied the effect of marginal expansion upon marginal adaptation at dentine-composite interface. It was concluded that water sorption causes gap reduction by hygroscopic expansion seen in the scanning electron microscope (SEM) as the volume increased. Krejci et al.[24] studied the marginal adaptation of conventional, hybrid and microfilled composite resins, after load cycling. They found that marginal adaptation of microfilled composites deteriorated during load cycling the margins while the other composites remained stable during load cycling. In addition, Makishi et al.[25] investigated the potential use of swept-source optical coherence tomography as a new tool to evaluate marginal adaptation of composite restorations in class I cavities. They stated that 3D imaging by swept-source optical coherence tomography can be considered as a non-invasive technique for fast detection of gaps at the restoration interface.Fróes-Salgado et al.[26] evaluated the effect of composite pre-polymerization temperature and energy density on the marginal adaptation, degree of conversion, flexural strength, and polymer cross-linking of a resin composite. Pre-heating the composite prior to light polymerization similar in a clinical situation did not alter the mechanical properties and monomer conversion of the composite, but provided enhanced composite adaptation to cavity walls.Opdam et at.[27] evaluated the quality of the marginal adaptation of composite restorations placed in vivo. Over extended margins observed by SEM were differ from those detected by radiographs. Mathew et al.[28] studied the marginal gap at the dentine/composite interface in class II composite restorations subjected to thermal cycling and has been effectively evaluated using the silver staining technique. Peutzfeldt et al.[29] evaluated the marginal gaps at enamel (occlusal) and dentin (gingival) margins of mesio-occlusodistal cavities, composite resin restorations made with different incremental insertion techniques. In addition, the effects of water storage on the marginal adaptation of two composite resins, two polyacid-modified composite resins and a pre-reacted glass-ionomer composite were investigated by Yap et al.[30]. They found that no significant difference in marginal gap formation was observed between materials under study and where bonding systems were not used, a decrease in gap width over time was observed with all materials. Marginal adaptation of high viscosity resin composite restoratives bonded to dentin in a cylindrical cavity modelwas evaluated by Rahiotis et al.[31]. No improvement was recorded on the quality of marginal adaptation following one week of water storage. Turkun et al.[32] evaluated a packable composite for posterior restorations for a period of three years. De Souza et al.[33] evaluated the clinical performance of two packable and one microhybrid composites placed in cavities of posterior teeth after one year. They-found that, the packable and microhybrid composites exhibited an excellent clinical performance after one year and may be considered possible materials for the restoration of posterior teeth. The marginal adaptation of a packable and hybrid composite restorations with self- etching adhesive systemwas evaluated by Poon et al.[34]. They concluded that, the clinical performances of both composites were similar and satisfactory for the restoration of class II cavities.Provisional resin crowns may be used for an extended period while complex treatments are completed. The crowns function intraorally; therefore, moisture absorption and thermal cycling may affect the physical properties of acrylic resin, causing a change in marginal gap size. One of the most important requirements for interim restorations is good marginal adaptation. Polymerization shrinkage of interim restorative materials can jeopardize the marginal integrity of interim restorations. Clinical performance and marginal adaptation of direct and semi-direct class II composite restorations in a split-mouth design over 3.5 years were studied by Reberto et al.[35]. The marginal accuracy of interim restorations made with 4 interim materials was compared by Nejatidanesh et al.[36]. The marginal integrity of dentine adhesives bonded to enamel and dentine, before and after thermo-mechanical loading (TML) was evaluated by Frankenberger[37].Martínez-Rus et al.[38] investigated the effect of different manufacturing techniques on the marginal adaptation of zirconia ceramic copings. The marginal accuracy achieved for the 4 zirconia-based ceramic crown systems analyzed was within the range of clinical acceptance.Dhillon et al.[39] investigated the effect of water temperature and duration of immersion on the marginal accuracy of provisional restoration fabricated in autopolymerizing resin. They concluded that polymerizing the polymethyl methacrylate resin provisional crowns by direct technique in the water maintained at 20–30°C temperature for 10 minutes resulted in better marginal fit and this method can be utilized in clinical conditions for better results.On the other hand, the effect of long-term water absorption and thermal cycling on marginal gap size of polymethyl methacrylate copolymer and bis-acrylic composite resin crowns was studied by Ehrenberg et al.[40]. Others aimed to evaluate whether the method of light curing could influence marginal sealing and resin composite adaptation to the cavity wall, polymerization contraction rate; and hardness at the top and bottom surfaces of a body of resin composite[41]. In addition, the effect of water sorption of composite and thermal stress on the marginal adaptation to the dentin cavity wall was evaluated by measurement of the gap width between composite fillings and the dentin cavity wall[42]. Although many studies have been done on composite restorations, it was thought that a study planned to evaluate and compare the marginal adaptation of different composite restorations might be of value.
2. Materials and Methods
2.1.Material
- Sixty sound human mandibular first molars were collected from a dental clinic from patients with ages ranged from 25-35 years. The collected teeth were cleaned from debris and blood by a tooth brush and soap under running water after storing them in 1% H2O2 for 24 hours. The collected teeth were examined using light microscope (PHMG, Olympus Optical Co. Ltd., Tokyo, Japan) to select molars that were free from cracks[3].The extracted teeth were stored in 0.2% Sodium Azide (has antibacterial activity) at room temperature before preparation and restoration[43]. The materials used in this study are listed in Table 1.
2.2.Specimen Preparation
- Intact teeth were mounted in auto-polymerizing acrylic resin blocks (Pekatray, Bayer Dental Leverkusen, Germany) that were confined by stainless steel holders. Each holder held three teeth positioned with crowns in proximal contacts and long axis parallel to the sides[44]. The tooth in between the axial teeth was used only to obtain firm contact areas as shown in Figure 1(a). Class II (occlusomesial) cavities were prepared with an occlusal box of dimensions 2.5 mm depth and 2 mm width. A proximal box of 3.5 mm depth and 3 mm width was made as shown in Figure1(b), using high speed hand piece (NSK, Tokyo, Japan) with continuous air-water cooling system[3].
2.3.Specimens Grouping
- Sixty molars were divided into three main groups according to the type of composite resins that were used. Each group consisted of 20 teeth. In group I Surefil was used as the restorative material, in group II Esthet–X–Improved was used, while in group III Glacier was used. Each group was subdivided into four subgroups (five teeth each) according to the storage intervals (24 hours, one week, two weeks and three weeks)[7].
2.4.Restorative Procedures
- After the preparation of each tooth, the cavity was dried using gentle air blast and a transparent matrix in a tofflemire matrix retainer (ProduitsDentaires SE, Switzerland) was used and held in place with light reflecting wedges (Dentalez Group, Malvern, USA) as shown in Figure 1(d). Phosphoric acid etchant gel 37% was applied to the enamel and dentin as shown in Figure1(e), and left for 15 seconds. After that it washed with water spray for ten seconds and air dried by oil free compressed air. Excess water was removed without over drying the dentin[3]. The Prime & Bond NT bonding agent was applied to the etched enamel and dentin using a disposable applicator tip as shown in Figure 1(f), for 20 seconds. The excess was gently air thinned for five seconds until a uniform glossy appearance was obtained, then bonding agent was light cured) (MEGA-PHYSIK Dental, D-76437-Rastatt, Germany) as shown in Figure 1(g), for ten seconds with a light curing unit (Chromalux light cure unit). In all specimens composite was applied to the cavity using the incremental technique, Figure 1(h). The thickness of each increment was about 2 mm and each increment was cured for 20 seconds according to manufacturer instructions.
2.5.Curing Procedures
- According to the manufacturer instructions, the first layer was applied with a suitable condenser (Compo-Sculp: DD 3, Sutr dental manufacturing, CHICO, CA). The composite resin was adapted to the cavity floor and walls, then light cured for 20 seconds. The second layer was applied similarly, then the anatomical occlusal surface was carved using shaping-sculpting instruments (Compo-Sculp: DD 1, 2, Sutr dental manufacturing, CHICO, CA) and light cured for 20 seconds as shown in Figure 1(i).
2.6.Finishing and Polishing
- The finishing was immediately done, gross excess was removed and a general outline form was established with diamond finishing instruments. Additional finishing was done by the use of "Enhance" finishing system (Dentsply Caulk, Mil ford , DE 19963-0359, USA) as shown in Figure 1(j). A high luster was established by using "Pogo" one step diamond micro-polisher system (Dentsply Caulk, Mil ford, DE 19963-0359, USA), according to the manufacturer's instructions. All the specimens were subjected to a total of six months in vitro simulated in vivo function[45] by exposing the restoration to thermal cycling and mechanical loading (Conservative Department Lab, faculty of Dentistry, Tanta University, Egypt).
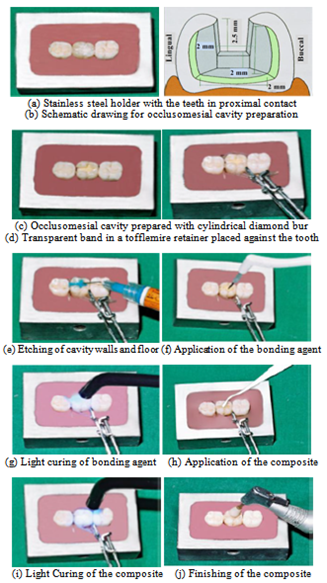 | Figure 1. Specimen preparation |
2.7.Thermal Cycling
- For thermal cycling, all the specimens were thermocycled between 5±2℃ and 55±2℃ for 300 cycles, with a dwell time 2 minutes and 10 seconds transfer time[45].
2.8.Load Cycling
- All specimens were fixed in mounting rings. The mounting ring was attached to the lower member of a custom – made loading machine which acted as the mandibular element, while an uniaxial load of 49 N was applied using a rounded end metal rod which was fascinated to the upper member of the machine, Figure 2.A 3mm diameter of the root was chosen to allow contacting restoration. A cam was attached between the two portions stabilizing the degree of opening (10cm) of the mandibular portion according to measurements taken from the natural tempro-mandibular joint movement. All specimens were subjected to 120,000 loading cycles corresponding to six months of clinical service thus simulating the clinical conditions as much as possible[45]. Each group was subdivided into four subgroups according to the storage period intervals. Subgroup specimens were stored in artificial saliva for one day, one week, two weeks and three weeks.
2.9.Evaluation of Marginal Adaptation
- Marginal adaptation was evaluated by using a Measurescope-10(Nikon Measurescope-10, Japan), as shown in Figure 3.At each time interval, specimens were blotted dry and inspected under the Measurescope-10 for marginal adaptation at magnification lens of 10x. The measurements were taken at three predetermined locations; midgingival, midbuccal and midlingual. The average of the three readings was recorded[3].
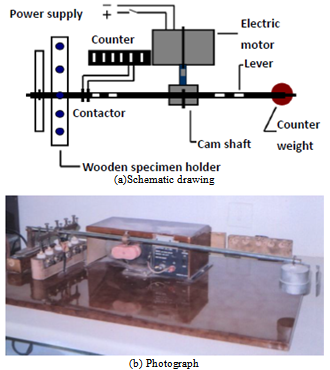 | Figure 2. Schematic drawing of load cycling machine |
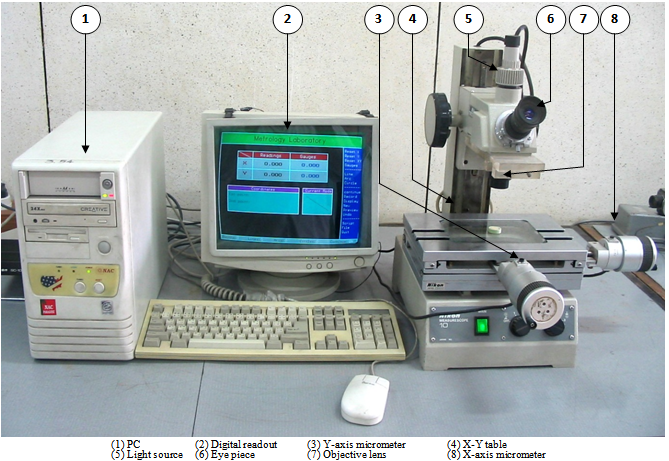 | Figure 3. Measurescope-10 used for marginal adaptation measurements |
|
|
3. Results and Discussion
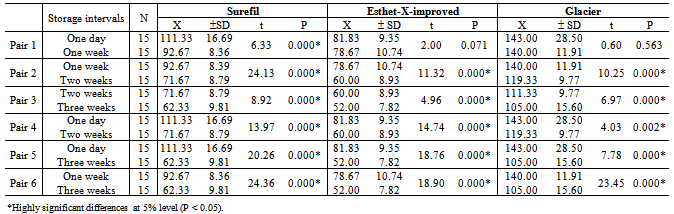
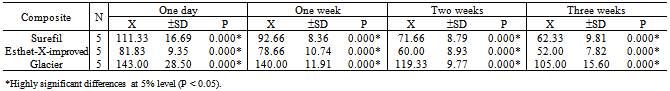
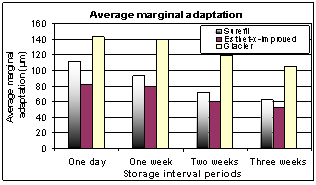
- Pair-wise comparisons between the mean values of marginal gap width as an indication of marginal adaptation at different storage intervals for each of the three composite restorative materials were applied using the student's t-test. The storage intervals, mean values of marginal gap width (X) for the used composite restorative materials, the standard deviations (SD) and the results of students' t-test at significant level (P) were listed in Table 2 and Figure 4. The students' t-test of pair-wise comparisons between mean values of marginal gap width as an indication of marginal adaptation at different storage intervals for each of the three composite restorative materials showed a highly significant difference at P<0.05. The students' t-test of pair-wise comparisons between mean values of marginal gap width as an indication of marginal adaptation at different storage intervals for each of the three composite restorative materials showed a highly significant difference at P<0.05 except for Esthet-X-improved and Glacier composite restorations in case of one day-one week storage intervals pair-wise comparison.On the other hand, analysis of variance test ANOVA was used to compare mean values of marginal adaptation width as an indication of marginal adaptation of each of the three composite restorative materials at one day, one week, two weeks and three weeks storage intervals, respectively. The mean values of the marginal gap width, the standard deviations and results of ANOVA test for the three composites at one day, one week, two weeks and three weeks storage interval were listed in Table 3 and Figure5.
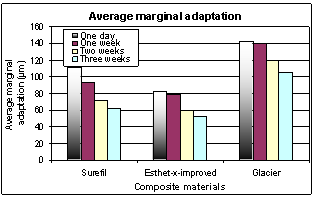 | Figure 5. Comparison between the mean values of the marginal gap width of the three composites at one day, one week, two weeks and three weeks storage interval |
4. Discussion
- Despite the improved characteristics of composite restorations, polymerization shrinkage remains a challenge and still imposes limitation in the application of direct techniques. This volumetric shrinkage ranges from 2-4%[2]. This study aimed to compare polymerization shrinkage of nanofilled, packable and hybrid composites, which are different in filler particle size, at different storage intervals (one day, one week, two weeks and three weeks), using artificial saliva[24]. Nanofilled composite was used because of the new technology used in its fabrication where its filler particle size ranges from (0.005-0.01µm). These very small particles don't react with the visible light and don't produce scattering resulting in significant absorption of light which leads to improvement in modulus of elasticity, depth of cure and esthetics[46-47].
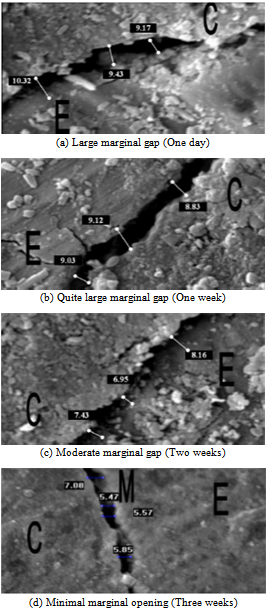
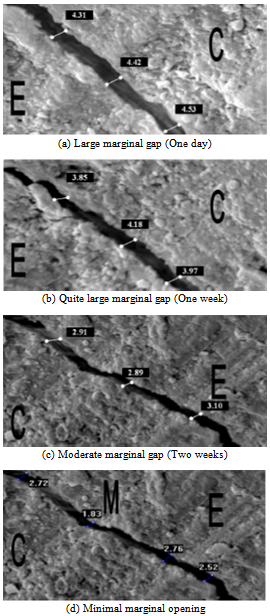 | Figure 6. Scanning electron microscope showing marginal gap between Surefil and enamel |
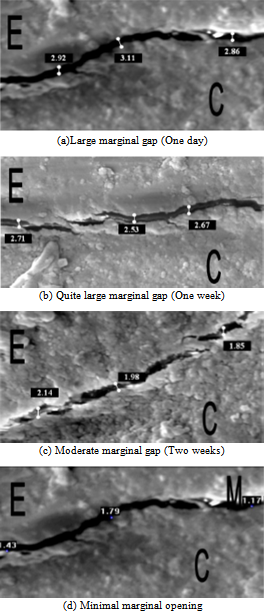 | Figure 7. Scanning electron microscope showing marginal gap between Esthet–X–improved and enamel |
 | Figure 8. Scanning electron microscope showing marginal gap between Esthet–X–improved and enamel |
5. Conclusions
- In this study the marginal adaptation of a three composites was measured and compared. Marginal adaptation was evaluated using Measurescope-10 and the results were confirmed with scanning electron microscope. For confirmation, a selected specimens from each subgroup were investigated by scanning electron microscope. These specimens were dried, sputter coated with gold-palladium and then photographed with scanning electron microscope at 1500x, It can be concluded that:1. Highly significant difference in marginal adaptation was found between the used three composites.2. Marginal adaptation of the nanofilled composite was better than the other composites used.3. After specimens storage in artificial saliva, there was a gradual improvement in the marginal adaptability of the specimens.4. From the present study it was concluded that, the marginal adaptation of the nanofilled composite was the best when compared to the other composites.Further studies are recommended to compare the other physical and mechanical properties and clinical uses of nanofilled and packable composites and to evaluate the uses of packable composites in anterior teeth. Packable composites need further development to improve its adaptability in posterior teeth.
References
| [1] | Wendt, S.L., Mcinnes, P.M. and Diekinson G.I., The effect of thermocycling in microleakgeanalysis. Dent. Mat.,vol. 8, pp. 181-84,1992 |
| [2] | Dietschi, D. and Dietschi, J., Current developments in composite materials and techniques. Practical periodontics and Aesthetic Dent,vol. 8, pp. 603-609, 1996 |
| [3] | Mathew, M.E.K., Nair, P. and Krishnan, K., Bonding agent is a decisive factor in determining the marginal leakage of dental composite. J. Oral Rehabil.,vol. 28, pp. 68-77, 2001 |
| [4] | Brannstrom, M., The cause of post-restorative sensitivity and its prevention. J. Endo., vol.12, pp. 520-25, 1986 |
| [5] | Phillips, R.W., New concepts in materials used for restorative dentistry. JADA,vol. 70, pp. 652-58, 1965 |
| [6] | Harrington, H. and Wilson, H.J., Depth of cure of radiation-activated materials-effect of the mould material and cavity size. J. Dent., vol. 21, pp. 305-11, 1993 |
| [7] | Ralph, H. and Esquivel, J., Phillips’ science of dental materials., 10thed., Mosby Co., Chapter 15, pp. 399-420, 1998 |
| [8] | Beun, S.,Glorieux, T., Devaux, J., Vreven, J. and Leloup, G., Characterization of nanofilled compared to universal and microfilled composites. Dental Materials, vol. 23, No. 1, pp. 51-59, 2007 |
| [9] | Turssi, C.P., Ferracane, J.L. and Serra, M.C., Abrasive wear of resin composites as related to finishing and polishing procedures. Dental Materials,vol. 21, pp. 641–648, 2005 |
| [10] | Lee, Y.-K., Lu, H., Oguri, M. and Powers, J.M., Changes in gloss after simulated generalized wear of composite resins. J.Prosthet. Dent., vol. 94, No. 4, pp. 370-376, 2005 |
| [11] | Bhimaraj, P., Burris, D.L., Action, J., Sawyer, W.G., Toney, C.G., Siegel, R.W. and Schadler, L.S., Effect of matrix morphology on the wear and friction behavior of alumina nanoparticle/poly(ethylene) terephthalate composites. Wear, vol. 258,pp. 1437–1443, 2005 |
| [12] | Silikas, N., Kavvadia, K., Eliades, G. and Watts, D., Surface characterization of modern resin composites: a multitechnique approach., Am. J. Dent., vol.18, No. 2, pp. 95-100, 2005 |
| [13] | Braem, M. Finger, W. Van Doren, V.E.Lambrechts andP.Vanherle, G., Mechanical properties and filler fraction of dental composites. Dent. Mater., vol. 5, pp. 346-349, 1989 |
| [14] | Condon, J.R. and Ferracane, J.L., Reduced polymerization stress through non-bonded nanofiller particles. Biomaterials,vol. 23, pp. 3807–3815, 2002 |
| [15] | Perdigao, J., Baratieri, L.N. and Lopes, M., Laboratory evaluation and clinical application of a new one-bottle adhesive. J.Esthet. Dent., vol.11, No. 1, pp. 23-35, 1999 |
| [16] | Tay, F.R., Moulding, K.M. andPashley, D.H., Distribution of nanofillers from a simplified-step adhesive in acid-conditioned, Dentin. J.Adhes. Dent., vol. 1, No. 2, pp. 103-117, 1999 |
| [17] | Musanje, L. and Ferracane, J.L., Effects of resin formulation and nanofiller surface treatment on the properties of experimental hybrid resin composite.Biomaterials, vol. 25,pp. 4065–4071, 2004 |
| [18] | de Andrade, An.K.M., Duarte, R.M., e Silva, F.D.S., Batista, A.U.D., Lima, K.C., Pontual, M.L.A. and Montes, M.A.J., 30-Month randomised clinical trial to evaluate the clinical performance of a nanofill and a nanohybrid composite. Journal of Dentistry, vol. 39, pp. 8–15, 2011 |
| [19] | Takahashi, H., Finger, W.J., Wegner, K., Utterodt, A., Komatsu, M., Wöstmann, B. and Balkenhol, M., Factors influencing marginal cavity adaptation of nanofiller containing resin composite restorations. Dental Materials, vol. 26, pp. 1166–1175, 2010 |
| [20] | Scheibenbogen A., Manhart J., Kunzelman H.K. and Hickel, R., One year clinical evaluation of composite and ceramic inlays in posterior teeth. J.Prosth. Dent., vol. 80, pp.410-16, 1998 |
| [21] | Rosin M., Urban D., Gartner C., Splieth C. and Meyer G., Polymerization shrinkage–strain and microleakage in dentin-bordered cavities.J.Dent. Mat.,vol. 18,pp. 521-528, 2002 |
| [22] | Idriss, S., Habib, C. Abdul Jabar, T. and Omar, R., Marginal adaptation of class II resin composite restoration using incremental and bulk placement techniques an SEM study. J. Oral Rehabil., vol. 30, pp. 1000-1007, 2003 |
| [23] | Thonemann, B.M., Federlin, M., Schmalz, G. and Hiller, K.A., SEM analysis of marginal expansion and gap formation in Class II composite restorations. Dent. Mat., vol. 13, pp. 192-197, 1993 |
| [24] | Krejci, I., Lutz, F. and Gaustschi, L., Wear and marginal adaptation of composite resin inlays. J.Prosthet. Dent., vol. 72, pp. 233-44, 1994 |
| [25] | Makishi, P., Shimada, Y., Sadr, A., Tagami, J., Sumi, Y., Non-destructive 3D imaging of composite restorations using optical coherence tomography: Marginal adaptation of self-etch adhesives. Journal of dentistry, vol. 39, pp. 316–325, 2011 |
| [26] | Fróes-Salgado, N.R., Silva, L.M., Kawano, Y., Francci, C., Reis, A. and Loguercio, A.D., Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dental Materials, vol. 26, pp. 908–914, 2010 |
| [27] | Opdam, N.J., Roeters, F.J., Feilzer, A.J. and Smale, I., A radiographic and scanning electron microscopic study of aproximal margins of class II resin composite restorations placed in vivo. J. Dent., vol. 26, pp. 319-327, 1998 |
| [28] | Shortal, A.C.,Microlekage, marginal adptation of composite resin restoration. Br. Dent. J., vol. 153, pp. 223-27, 1982 |
| [29] | Peutzfeldt, A. and Assmussen, E., Influence of flowable and self-curing composite lining on microleakage in vitro.Oper. Dent., vol. 27, pp. 569-75, 2002 |
| [30] | Yap, A., Shah, K. and Chew, C., Marginal gap formation of composites in dentine: Effect of water storage. J. Oral Rehabil.,vol. 30, pp. 236-42, 2003 |
| [31] | Rahiotis, C., Tzoutzas, J. and Kakaboura, A., In vitro marginal adaptation of high viscosity resin composite restorations bonded to dentine cavities. J. Adhesive Dent., vol. 1, pp. 49-53, 2004 |
| [32] | Turkun, L.S., Turkun, M. and Ozata, F., Clinical performance of packable resin composite for a period of 3 years. Quint. Int.,vol. 36, pp. 365-72, 2005 |
| [33] | De Souza, F.B., Guimaraes, R.P. and Silva, C.H., A clinical evaluation of packable and microhybrid composite restorations: one year report. Quint.Int.,vol. 36, pp. 41-48, 2005 |
| [34] | Poon, E.C., Smales, R.J. and Yip, K.H., Clinical evaluation of packable and conventional hybrid posterior resin-based composites: results at 3.5 years.JADA, vol. 136, pp. 1533-40, 2005 |
| [35] | Spreafico, R.C., Krejci, I. and Dietschi, D., Clinical performance and marginal adaptation of class II direct and semidirect composite restorations over 3.5 years in vivo. Journal of Dentistry, vol. 33, pp. 499–507, 2005 |
| [36] | Nejatidanesh, F., Lotfi, H.R. and Savabi, O., Marginal accuracy of interim restorations fabricated from four interim autopolymerizing resins. J.Prosthet. Dent., vol. 95, pp. 364-367, 2006 |
| [37] | Frankenberger, R. andTay, F.R., Self-etch vs etch-and-rinse adhesives: Effect of thermo-mechanical fatigue loading on marginal quality of bonded resin composite restorations. Dent. Mater., vol. 21, pp. 397-412, 2005 |
| [38] | Dhillon, N., Kumar, M. and D’Souza, Effect of water temperature and duration of immersion on the marginal accuracy of provisional crowns., Medical Journal Armed Forces India (MJAFI), vol. 67, No 3, pp. 237-240, 2011 |
| [39] | Martínez-Rus, F., Suárez, M.J., Rivera, B. and Pradíes, G., Evaluation of the absolute marginal discrepancy of zirconia-based ceramic copings. J. Prosthet. Dent., vol. 105, pp. 108-114, 2011 |
| [40] | Ehrenberg, D., Weiner, G.I. and Weiner, S., Long-term effects of storage and thermal cycling on the marginal adaptation of provisional resin crowns: A pilot study. J.Prosthet. Dent., vol. 95, pp. 230-236, 2006 |
| [41] | Yoshikawa, T., Burrow, M.F. andTagami, J., A light curing method for improving marginal sealing and cavity wall adaptation of resin composite restorations. Dental Materials,vol. 17,pp. 359-366, 2001 |
| [42] | Koike, T. Hasegawa, T. Manabe, A. Itob, K. andWakumoto,S.,Effect of water sorption and thermal stress on cavity adaptation of dental composites. Dent. Mater.,vol. 6, pp. 178-180, 1990 |
| [43] | Han, B., Attin, T., Grofke, M. and Hellwig, E., Influence of resin cement viscosity on microlekage of ceramic in lays. Dent. Mat., vol. 17, pp. 191-196, 2001 |
| [44] | Brend, D. and Geurner, W., Molar fracture resistance after adhesive restoration with ceramic in lays or resin based composite., Am. J. Dent., vol. 14, pp. 216-220, 2001 |
| [45] | Krejici, I., Lutz, F. and Reimer, M., Marginal adaptation and fit of adhesive ceramic in lay., J. Dent., vol. 21, pp. 39-46, 1993 |
| [46] | Stephen, C. and Duane, F., Dental materials, the art and science of operative dentistry.3rded., Mosby Co., pp. 206-288, 1998 |
| [47] | Norpert, N., Noszner, S. and Simone, K., Nanotechnology for dental composite. Dent. Mat., vol. 19, pp. 725-55, 2004 |
| [48] | Tung, F.F., Estafan, D. and Scherer, W.,Microleakage of condensable resin composite: an in vitro investigation. Quint. Int., vol. 31, pp. 430-34, 2000 |
| [49] | Deborah, S., Katherine, M., Marcos, A. and Grald, A., The physical properties of packable and conventional posterior resin-based composites: A comparison. JADA, vol. 131, pp. 1610-1615, 2000 |
| [50] | Al-Salehi, S.K., Sturb, J.R. and Lü, X.Y., Wear of composite resin veneering materials in a dual axis chewing simulator. J. Oral Rehabil., vol. 26, pp. 147-58, 1989 |
| [51] | Mandras, R.S., Retief, D.H. and Russell, C.M, The effect of thermal and occlusal stresses on the microlekage of the scotch bond to dentinal bonding system.Dent. Mat., vol. 7, pp. 63-67, 1991 |
| [52] | Feilzer, A.J., Bcgee, A.J. and Davidsson, C.L., Increased wall to wall curing contraction in thin bonded resin layers. J. Dent. Res., vol. 68, pp. 48-50, 1989 |
| [53] | Söderholmk, J.M., Yanng, M.C.K. and Garcea, I., Filler particle leachability of experimental dental composite. EUR J. Oral Sci., vol. 68, pp. 555-560, 2000 |
| [54] | Boyde, M. and Kight, W., The use of SEM in clinical dental research. Br. Dent. J., vol. 127, pp. 313-22, 1969 |
| [55] | Martin, N. and Jedynakiewicz, N., Measurement of water sorption in dental composites. J. Biomaterials, vol. 19, pp. 77-85, 1998 |
| [56] | Koike, T., Hasegawa, T., Manate, A., Itoh, K. and Wakumoto, S., Effect of water sorption and thermal stress on cavity adaptation of dental composite. Dent. Mat., vol. 3, pp. 178-80, 1990 |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML