-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2023; 13(1): 1-7
doi:10.5923/j.ajb.20231301.01
Received: Aug. 14, 2023; Accepted: Aug. 25, 2023; Published: Sep. 12, 2023

Interest of Ultrasensitive Reactive Protein C in Cardiovascular Risk Assessment in Senegal
Doupa Dominique1, Gnonhouri Yahi Antoinette Marie Ange1, Thiam Souleymane2, Makalou Demba1, Cissé Fatou2, Dia Diatou Gueye3, Beye Serigne Mor4, Sy Mathieu4, Diop Mamadou1, Sagna Helene Ange Thérèse5, Pape Matar Kandji5, Djite Moustapha5, Kane Adama4, Dieye Pape Madieye5, Diagne Ibrahima1
1Laboratory of Biochemistry-Hematology, UFR of Health Sciences Gaston Berger University of Saint-Louis, Senegal
2Laboratory of Biochemistry-Molecular Biology, Cheikh Anta Diop University of Dakar, Senegal
3Service of Internal Medicine, UFR of Health Sciences Gaston Berger University of Saint-Louis, Senegal
4Pharmaceutical Biochemistry Laboratory, Cheikh Anta Diop University of Dakar, Senegal
5Service of Cardiology, UFR of Health Sciences Gaston Berger University of Saint-Louis, Senegal
Correspondence to: Doupa Dominique, Laboratory of Biochemistry-Hematology, UFR of Health Sciences Gaston Berger University of Saint-Louis, Senegal.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

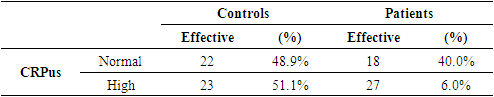
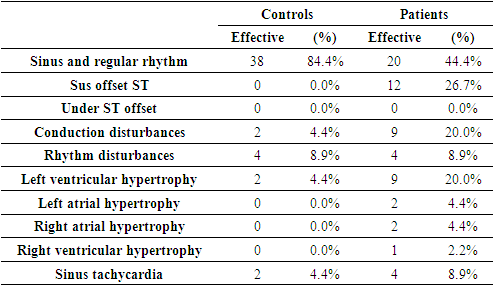
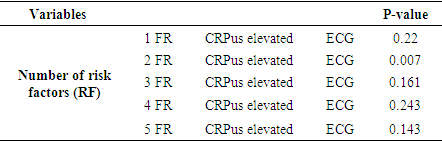
Cardiovascular diseases (CVD) are one of the leading causes of death in developed countries and their incidence is increasing in developing countries. Recently other biological markers are an alternative in the assessment of cardiovascular risk in particular: ultra-sensitive CRP. The CRP control of the inflammatory reaction essential component in the process of atherogenesis has a lower limit of detection than the conventional dosage of CRP. It is in this context that the present study was conducted with the objective of showing the interest of CRPus in the assessment of cardiovascular risk in the population of Saint-Louis. This was a prospective cross-sectional analytical study and involved 90 patients including 45 patients and 45 controls. Socio-demographic, clinical and paraclinical data were collected from a questionnaire and biological data from blood samples. Our study population had an average age of 60± 14 for patients and 56.7±18 for controls. There was also female predominance in both patients. The most predominant cardiovascular risk factor was hypertension with 86.4%. The most observed electrocardiographic abnormalities in patients were dominated by ST excess shift (26.7%) unlike controls where they were dominated by rhythm disorders (8.9%). The average CRPus was relatively higher in patients than in controls with respectively (20.3mg/l vs 13.7mg/l). A relationship between elevated CRPus and cardiac impact was observed in patients with 2 cardiovascular risk factors. Based on these preliminary results, CRPus could be a promising marker for early detection of patients at risk but also for follow-up.
Keywords: Assessment, Ultrasensible Reactive Protein C, Cardiovascular risk, Senegal
Cite this paper: Doupa Dominique, Gnonhouri Yahi Antoinette Marie Ange, Thiam Souleymane, Makalou Demba, Cissé Fatou, Dia Diatou Gueye, Beye Serigne Mor, Sy Mathieu, Diop Mamadou, Sagna Helene Ange Thérèse, Pape Matar Kandji, Djite Moustapha, Kane Adama, Dieye Pape Madieye, Diagne Ibrahima, Interest of Ultrasensitive Reactive Protein C in Cardiovascular Risk Assessment in Senegal, American Journal of Biochemistry, Vol. 13 No. 1, 2023, pp. 1-7. doi: 10.5923/j.ajb.20231301.01.
Article Outline
1. Introduction
- Cardiovascular diseases (CVD) according to the HAS (High Health Authority) correspond to various chronic pathologies or events having in common a pathophysiology related to atherosclerosis [1]. According to the World Health Organization (WHO), cardiovascular diseases are the leading causes of death worldwide with nearly 17.9 million victims each year [2]. About 80% of deaths occur in low- and middle-income countries, and many of them involve adults [2]. CVD is currently a public health problem especially in developing countries where financial resources are lacking. They kill as much as AIDS, malaria, cancer, diabetes, pneumonia, tuberculosis. As a result, they constitute a real obstacle to the emergence of our countries [3]. Cardiovascular diseases have a pathophysiology related to atherosclerosis which is a multifactorial disease in which inflammation plays a key role both in the pathogenesis of the disease and in the weakening of plaque and thrombo-events occlusive conditions that follow [4]. The appearance of atheroma is related to the presence of several risk factors that can be physiological such as age, sex or pathological such as hypertension, dyslipidemia, diabetes. Among the classic risk factors, lipids and especially hypercholesterolemia play an important role in triggering lesions [5]. High triglyceride levels are also associated with an increased risk of cardiovascular disease [5,6]. Recently other biological markers are an alternative in the assessment of cardiovascular risk in particular: ultra-sensitive CRP.The CRPus control of the inflammatory reaction, an essential component in the atherogenesis process, has a lower limit of detection than the conventional dosage of CRP.Ultrasensitive CRP (CRPus) is mainly proposed in the screening and evaluation of cardiovascular risk in primary prevention. Numerous descriptive epidemiological investigations have highlighted the existence of a relationship between this marker and the increase in the incidence of cardiovascular diseases, however, the pathophysiological mechanisms of this association are not clearly established and their relevance at the individual level remains controversial. In recent years there has been significant progress in the field of research on cardiovascular diseases in the world, nevertheless this field remains poorly explored in our countries. It is in this context that this study proposes to show the interest of CRPus in the evaluation of cardiovascular risk in the population of Saint-Louis with the specific objectives of:• describing elements of cardiovascular risk in the Saint Louis population,• assessing cardiovascular impact of study patients• correlating cardiovascular impact with ultra-sensitive CRP (CRP us).
2. Methodology
- Ø Type of studyThis is a prospective case-control study conducted in the cardiology department of the Saint-Louis Regional Hospital Center (CHRSL) from 16/01/23 to 21/02/23.Ø Study populationThe study was conducted on patients received in consultation or hospitalized in the cardiology department of the Saint-Louis Regional Hospital Center (CHRSL) and described two types of populations:• Patients: patients with at least one cardiovascular event such as myocardial infarction, stroke, peripheral arterial disease (PAD) and cardiovascular risk factors.• Controls: patients with cardiovascular risk factors but without cardiovascular events such as myocardial infarction; stroke, PAD.Ø Inclusion criteriaIncluded in this study were:• patients with cardiovascular risk factors with or without cardiovascular events.• 16 years of age at least.• volunteers to participate in the study according to the Helsinki II amendments and criteria with signature of the consent form.• follow study protocol (at least 12 hours of fasting mandatory).Ø Non-inclusion criteria• all persons refusing to sign the consent form.• people who were not fasting at the time of the study.Ø SamplingThe recruitment was exhaustive including systematically all admitted during the study period and fulfilling the inclusion criteria defined above.Ø Data collectionData were collected using a questionnaire with the following parametersü Socio-demographic dataThe socio-demographic data used were: age, sex, marital status, occupation, level of education, locality.ü Personal history• Modifiable cardiovascular risk factors: dyslipidemia; hypertension (hypertension); diabetes; smoking; sedentary lifestyle.• History of stroke (stroke), peripheral arterial disease, myocardial infarctionü Clinical data• Clinical and anthropometric data were collected: weight, height, body mass index, right and left arm blood pressure.• Some symptoms such as: anginal chest pain, pain in the calf, the presence of headaches, blurred vision, dyspnea were sought at the interrogation.ü Paraclinical dataThe paraclinical data included in this study were:• Ultrasensitive Reactive Protein C (CRPus)• Fasting blood glucose• Total cholesterol• Triglyceridemia• HDL cholesterol• LDL-cholesterol• ElectrocardiogramThe parameters of the biological balance that are: total cholesterol, HDL-Cholesterol, triglycerides, blood sugar were measured by the usual enzymatic methods. The reading is made on spectrophotometer using the Biosystems Kit and the results expressed in (g/l). Serum LDL-cholesterol concentrations were obtained by calculation using the Friedewald Method [7]. When the triglyceride level was above 3.4 g/l, the LDL was determined by the direct method. CRPus was assayed by immunoturbidimetric method on multiparameter ARCHITECTØ Data entry and analysisData capture and analysis was performed using Excel 2013 and SPSS VERSION 22. Qualitative variables were expressed in frequency and quantitative on average, with description of the standard deviation. Averages and percentages were compared using the Chi2 test. Any difference lower than 0.05 was considered statistically significant.Ø Ethical considerationsThe data collection was authorized by the head of the cardiology department. The management of the information was done in strict respect of medical secrecy and anonymity. Ethical principles were applied throughout this study.
3. Results
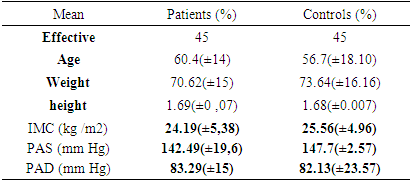
- 90 individuals were included in our study including 45 patients and 45 controls. The average age of patients was 60.4 years (± 14) years with extremes ranging from 26 to 83 years, while the average age of controls was 56.7 years (±18.10) years with extremes ranging from 16 to 85 years. The most representative age group was the one whose age was between 66 and 70 years in both patients and controls (Figure 1).
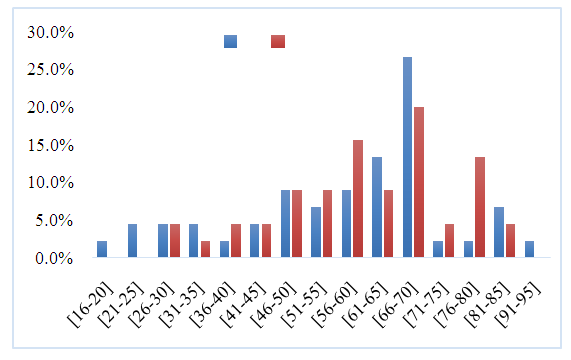 | Figure 1. Distribution of the population by age |
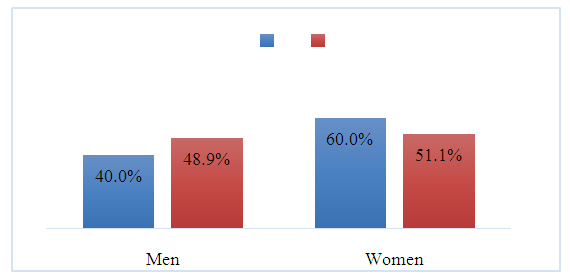 | Figure 2. Distribution of population by sex |
|
|
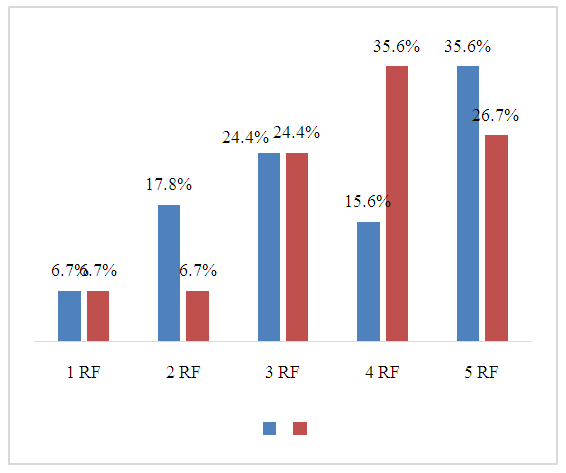 | Figure 3. Population distribution by number of risk factors |
|
|
|
|
|
4. Discussion
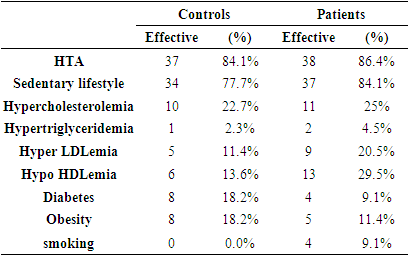
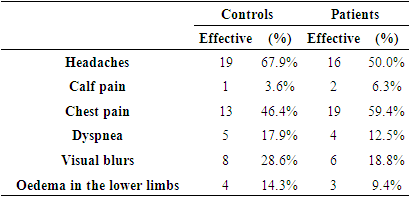
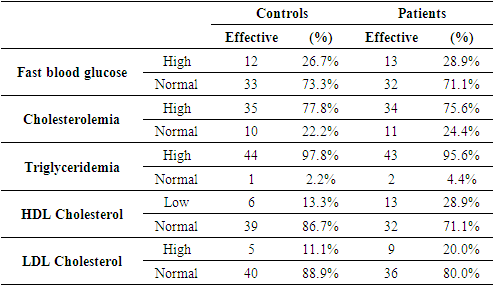
- Ø AgeOur study population had an average age of 60.4 years for patients and 56.7 years for controls. The 66-70 age group was the most represented in our population. These results are similar to those found by: Hira and al [13] with 58 years for cases and 50 years for controls, El Oudi and al [14] 61.5 years for patients and 52.4 years for controls, in their Tunis studies. Schulze et al [15] in America had a mean age of 65.4 years for patients and 62.7 years for controls.Our results confirm that patients who had a cardiovascular event were older than those who had not. This could be explained by the fact that the frequency of cardiovascular diseases increases with age.Ø SexA female predominance was observed in our study with a sex ratio of 0.9 in patients versus 0.6 in controls. Our results are superimposed with those of Doupa and al (Senegal) [16] and El Oudi et al (Tunisia) [14] which found respectively a sex ratio M/F 0.60 and 0.66. This same trend was found by Hrira et al [13] with a sex ratio of 0.8 [46]. However, Gupta et al [17] found in their study, a male predominance with an M/F sex ratio of 5.74.This female predominance in most studies could be explained by the emigration of men to the capital on the one hand, and by the interest that women give to these types of surveys on the other.Ø Cardiovascular risk factorsHigh blood pressure was the predominant risk factor in our two populations with patients and controls respectively: 86.4% versus 84.1%; followed by sedentary lifestyle with 84.1% versus 77.7%; and hypercholesterolemia, with 25% versus 22.7%.In the work of M Oudi and al (Tunisia) [14], hypertension was also recognized as the most frequent risk factor with 66%, followed by obesity, 37.5% and hypercholesterolemia 20.83%. These results are also superimposed on those performed by Pessinaba et al (Saint-Louis, Senegal) [18] where high blood pressure (46%) was the most predominant factor.However, Gupta et al (India) [17] and Doupa and al (Senegal) [16] found dyslipidemia in the foreground. Amit Khera et al (Dallas) [8] reported smoking (29.9%) as the predominant risk factor, followed by high blood pressure (21.6%). then diabetes (5.6%).This heterogeneity in the prevalence of risk factors could be explained on the one hand by lifestyles and habits that vary from one country to another and on the other hand by the lack of awareness of populations about the impact of poor eating habits on the occurrence of cardiovascular diseases.Ø Cardiac abnormalitiesThe patients who did not have a cardiovascular event, had mostly a normal electrocardiogram (84.5%) unlike the cases that they had cardiovascular abnormalities in the ECG (55.6%). The electrocardiographic abnormalities found were:• ST offset (26.7%) in patients;• Conduction disorders (26.7%) in patients versus (4.4%) in controls;• Rhythm disorders (8.9%) in both populations;• Sinus tachycardia (8.9%) in patients vs. (4.4%) in controls;• Left ventricular hypertrophy (20.0%) in cases vs (4.4%) in controls.Our results are comparable to those of Kafata et al who found (Brazzaville) [19] as abnormalities in the electrocardiogram: left ventricular hypertrophy (9%); conduction disorders (9%); ST sus shift (8%). Kouchab et al (Morocco) [20] mainly found rhythm disorders followed by left ventricular hypertrophy, ST sus shift and conduction disorders as abnormalities on the ECG. These cardiovascular abnormalities at the electrocardiogram could be explained by the accumulation of cardiovascular risk factors in our populations.The majority of controls and patients had at least two cardiovascular risk factors.Ø SymptomsSymptoms frequently encountered in our study were approximately similar in patients and controls with headache type (50.0%) vs (67.9%); chest pain (59.4%) vs (46.4%); visual blurring (18.8%) vs (28.6%).These symptoms found in the majority of patients in our study are also described in the study of Damourou et al [21], with a predominance of chest pain (16.2%), headache (11.1%), visual disorders (0.4%).These symptoms could be related to complications of high blood pressure; which for the most part, is not monitored or treated in our populations.Ø Biological parametersü CRPusPatients had higher CRPus (60%) compared to controls (51%).The mean CRPus in patients was 20.27 mg/l and 13.28mg for controls. Our results were similar to those of Hrira and al [13], which showed that the average CRPus levels were in the order of 3 mg/L and 6.9mg/L respectively in controls and cases. Another study by M Oudi et al [14] found that patients who developed cardiovascular complications had higher values of ultra-sensitive CRP compared to patients who had no complications. Similarly, Paul Ridker and David Morrow in their work in Boston found that initial concentrations of CRPus, were significantly higher in people who suffered a stroke than in those who did not [4].These high levels of CRPus in patients, could be explained by the pro-inflammatory properties of ultra-sensitive CRP on monocytes and macrophages, thus inducing a deleterious effect on the vascular wall.ü Blood glucoseAverage blood glucose was 1.02 in patients and 1.06 in controls.Hyperglycemia (>1.10 g/ l) was found in 26.7% of controls and 28.9% of patients.In the Hrira and al [13] study, hyperglycemia was found in 22% of controls and 54% of patients. As for Rizzo et al [22], they found hyperglycemia in 17% of the controls and 35% of the cases.This low prevalence of hyperglycemia in our study could be explained by the policy of awareness and promotion of diabetes screening conducted in the commune of Saint-Louis.ü Lipid profileHypercholesterolemia was the most common dyslipidemia in both populations. The prevalence of hypercholesterolemia was higher in patients (24.4%) than in controls (22.2%). El Oudi et al in their study in Tunisia found a prevalence of hypercholesterolemia lower than ours (20.83%) [14]. Pessinaba et al showed in their study in Saint-Louis; a high prevalence of hypercholesterolemia (36.3%) [18].These results could be explained by the westernization of the way of life of our African populations which, marked by a dietary change favoring diets rich in saturated fatty acids, cholesterol at the expense of traditional diets [56].ü CRPus and cardiac abnormalitiesIn our study, elevated CRPus in patients and controls was significantly associated with cardiac echo (P=0.00). Other studies have shown that CRPus is not only a marker of inflammation but also, was a direct cause of cardiovascular disease [23,24]. An eight-year study of 543 men with MI, cerebral infarction or thrombosis compared to 543 apparently healthy men, showed that increased CRPus was associated with increased risk of cardiovascular complications. Other studies have confirmed that high CRPus is an independent risk factor for cardiovascular disease [25].It is possible to explain this correlation between CRPus and cardiac echo, by the fact that CRPus could be a predictive element of the occurrence of cardiovascular events.ü Relationship between CRPus elevation, number of risk factors and cardiac impactIn our study, only the increase in the rate of ultrasensitive CRP combined with two risk factors, were associated with cardiac impact, with a statistically significant difference (p=0.007).While Hrira et al in Tunis, in their study of 146 subjects, divided into two groups, showed that the increase in the rate of CRPus was related to the association of several risk factors [13]. Other authors such as Yu and Rifai [60] demonstrated that the rate of CRPus was associated with the number of risk factors and correlated with cardiovascular complications. Our results are partially in agreement with those of the literature and would be explained by our low sampling, the age difference and the general health status of our populations.Ø Limits of the studyThis preliminary work has a number of limitations:• a larger sample and longitudinal follow-up would have helped to better highlight the impact of elevated CRPus on cardiovascular complications;• the association of CRPus with other biological markers such as troponin, homocysteine, D-dimers would have been more relevant to assess cardiac impact;• paraclinical tests such as: cardiac ultrasound, arterial echodoppler in all patients in the study, would have improved the assessment of cardiovascular impact.
5. Conclusions
- This study confirms the high prevalence of cardiovascular risk factors in the population of Saint-Louis. Because of the high mortality associated with these diseases, early diagnosis is therefore necessary. Based on these preliminary results, CRPus could be a promising marker for early detection of patients at risk but also for follow-up. However, additional studies with a large cohort would support these preliminary results.
AKNOWLEDGMENTS
- The authors thank the Director of the hospital, the medical staff of the cardiology clinic and the patients who voluntarily agreed to participate in this work.
Funding
- This study was funded by the research support fund of the Health Sciences Training and Research Unit of the Gaston Berger University of Saint Louis.
Author Contribution
- The author participated in the development of the protocol, the exploration of patients, the exploitation of the results and finally in the writing of this article.
Conflict of Interest
- The authors declare that there is no conflict of interest.
Consent
- Written and verbal consent was obtained for each participant.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML