-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2022; 12(1): 8-11
doi:10.5923/j.ajb.20221201.03
Received: Aug. 31, 2022; Accepted: Nov. 16, 2022; Published: Nov. 24, 2022

Evaluation of the Metabolic Syndrome in Patients Undergoing Opiate Substitution Treatment with Methadone at the Center for Integrated Addiction Management in Dakar
Kandji Pape Matar1, Djite Moustapha1, 2, Barry Nene Oumou Kesso1, 2, Thioune Ndeye Mareme1, Najah Fatou Coly-Gueye2, Zongo Cindy1, Samba Omar3, Djiba-Ndiaye Mbayang3, Ndiaye Ibrahima3, Ba Makhtar3, Gueye-Tall Fatou2, Lopez-Sall Philomene2, Gueye Papa Madieye1, 2
1Laboratory of Biochemistry-Hematology, National University Hospital of Fann, Dakar, Senegal
2Laboratory of Pharmaceutical Biochemistry, Faculty of Medicine, Pharmacy, Cheikh Anta Diop University, Dakar, Senegal
3Center for Integrated Care of Addictions, Center Hospitalier National Universitaire de Fann, Dakar, Senegal
Correspondence to: Kandji Pape Matar, Laboratory of Biochemistry-Hematology, National University Hospital of Fann, Dakar, Senegal.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Methadone is a full μ-opioid receptor agonist, used as first-line treatment in the treatment of heroin addicts. However, in recent years its use seems to be associated with metabolic and endocrine alterations. The objective of this study was to assess the prevalence of metabolic syndrome (SM) in patients undergoing opioid substitution treatment (OST) with methadone. This is a prospective and analytical study. Patients were recruited at the Center for Integrated Addiction Management in Dakar (CEPIAD) and the analyzes carried out at the Biochemistry laboratory of the CHNU in Fann. To define the metabolic syndrome (MS), we used the criteria of the International Diabetes Federation (IDF) 2009. Fifty patients were included in our studywith an average age of 50.18 years with a male predominance. The mean daily methadone dose was 64.5 mg and the mean follow-up time was 2.67 years. The frequency of metabolic syndrome was estimated at 6% of our study population. Hypertension was the most found component of MS (22%) followed by abdominal obesity (18%), hypo HDL-cholesterolemia (14%), hypertriglyceridemia (10%) and hyperglycemia (2%). The results show that the chronic administration of methadone could actually promote the onset of the metabolic syndrome.
Keywords: Metabolic syndrome, Methadone, IDF 2009, HTA, Diabetes
Cite this paper: Kandji Pape Matar, Djite Moustapha, Barry Nene Oumou Kesso, Thioune Ndeye Mareme, Najah Fatou Coly-Gueye, Zongo Cindy, Samba Omar, Djiba-Ndiaye Mbayang, Ndiaye Ibrahima, Ba Makhtar, Gueye-Tall Fatou, Lopez-Sall Philomene, Gueye Papa Madieye, Evaluation of the Metabolic Syndrome in Patients Undergoing Opiate Substitution Treatment with Methadone at the Center for Integrated Addiction Management in Dakar, American Journal of Biochemistry, Vol. 12 No. 1, 2022, pp. 8-11. doi: 10.5923/j.ajb.20221201.03.
1. Introduction
- The phenomenon of opioid addiction is a public health problem and is encountered all over the world. It affects approximately 34.3 million individuals, including 19.4 million heroin users (UNODC, 2018). Currently, the recommended treatment in the management of opioid addiction is that using methadone because of the results compared to detoxification. Methadone is a full μ-opioid receptor agonist, considered the first-line treatment in the management of drug addiction. Indeed, methadone treatment has demonstrated its effectiveness in patients who regularly follow detoxification treatments. In fact, during treatments using methadone, there is good therapeutic compliance and a reduction in the use of other opioids. In addition, there is a reduction in risky behavior linked to infectious diseases (AIDS, hepatitis), criminal behavior linked to fatal overdoses, thus improving the patient's quality of life [1]. Moreover, the clinical use of methadone has often been implicated in the occurrence of metabolic and endocrine alterations [2]. Weight gain very often appears in the first months or years following the start of methadone treatment; and although not systematic, it can be serious for the subject treated [3]. It is in this context that we set ourselves the objective of evaluating the prevalence of the metabolic syndrome in subjects who were under OST with methadone at CEPIAD.
2. Materials and Methods
- This is a prospective and analytical study carried out at the Biochemistry Laboratory of the Fann National University Hospital between November 2018 and May 2019. The patients were recruited from the Center for Integrated Addiction Management in Dakar. Under OST with methadone, matched with healthy controls according to sex and age ± 2 years. Subjects included after informed consent. Patients not on methadone, non-compliant patients and non-consenting subjects were excluded from the study. Blood samples were collected from subjects fasting for 12 h, at rest and Venipuncture in a tube with sodium fluoride for the measurement of fasting blood glucose and a dry tube for the measurement of lipid profile parameters. The dosage of the different biochemical parameters (glycaemia and lipid balance) was carried out with the BA400 automaton (BioSystems, Barcelona, Spain) using enzymatic techniques. LDL-c concentration was calculated using Friedewald's formula: (LDL-c (g/L) = CT - (HDLc+TG/5)). Data recording was done with Excel software, and exploration was done with XLSTAT 2019. Student's T-test was used to compare means and the Chi2 test to compare frequencies. A P-value of less than 0.05 was considered a statistically significant difference.
3. Result
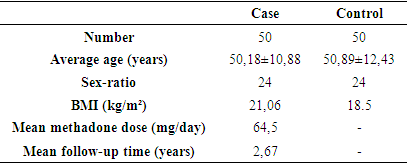
- Fifty subjects were included in our study under OST by methadone. The average age of patients was 50.18 ± 10.88 years with extremes of 30 and 71 years and the age group of 50 to 60 years was the most represented with a rate of 36% of subjects. In the study population men were in the majority with a frequency of 96%. The average BMI was 21.06 kg/m² and the average duration of patient follow-up was 2.67 years (Table 1).
|
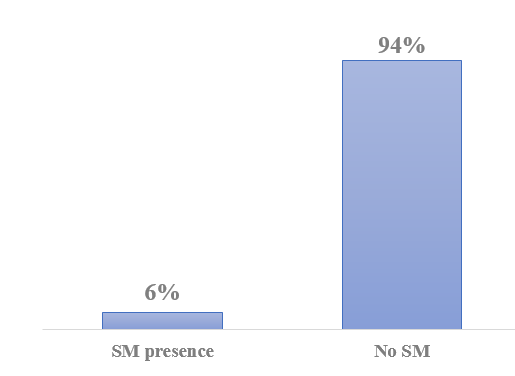 | Figure 1. Frequency of metabolic syndrome in the study population |
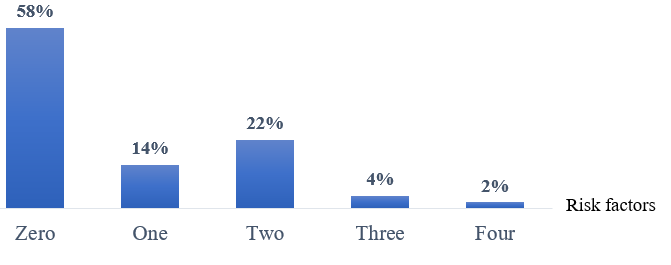 | Figure 2. Distribution of risk factors in patients |
|
|
|
4. Discussion
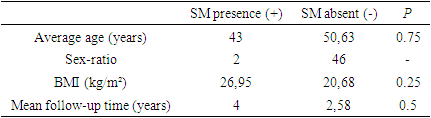
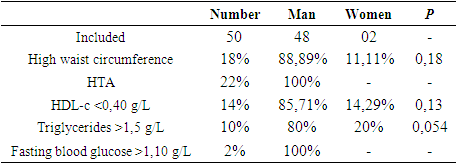
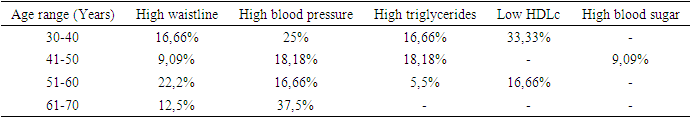
- Methadone is a synthetic opioid used in the treatment of chronic pain and the management of opioid addiction. Its use has recently increased due to its effectiveness, long duration of action and low cost. However, its clinical use has been implicated in the occurrence of metabolic and endocrine alterations. The objective of our study was to evaluate the metabolic syndrome in patients under OST with methadone at CEPIAD. The average age of our study population was 50.18 years with extremes of 30 and 71 years. In addition, most of the subjects included in our study (82%) were under the age of 60, which demonstrates the youth of our study population but especially that of the subjects followed at the CEPIAD level. This result is corroborated with that of Vallecillo et al in a similar study with an average age of 46.1 years [4]. Similarly, Marcuello et al found results comparable to ours [5]. The distribution according to the sex of our population showed a great male predominance with a rate of 96%. This result thus consolidates what has been found in the literature which reports the low rate represented by women at the level of drug addiction treatment centres. In Canada, the study by Maruyama et al found a frequency of 71.9% for men [6]. This male predominance found during our study could be explained by the fact that in Africa women are less exposed than men to smoking and drug taking. In the present study, the evaluation of the metabolic syndrome was made according to the criteria proposed by the IDF in partnership with the AHA (American Heart Association), the NHLBI (National Heart Lung and Blood Institute), the International society of Atherosclerosis and the International Association for the Study of Obesity. It is intended to "harmonize the criteria for defining the metabolic syndrome" and provides a much more consensual definition than that proposed by the various learned societies working in this field, such as the WHO and NCEP/ATP III. Thus, we found population a frequency of 6% of the metabolic syndrome with respect to the criteria of the IDF of 2009. This rate is below the values reported in the literature on the work carried out in similar centers. In southern Iran, Mattoo et al found a frequency of 29.3% in 2013 and Yousefzadeh G et al, in 2015 had found a rate of 39% [7-8]. In the United States in 2016, Vallecillo et al, in a study on the prevalence and factors associated with the metabolic syndrome in subjects on methadone replacement therapy had found a frequency of 29.5% [4]. In Africa and mainly in our region, no study of this kind has been found. The underestimation of the prevalence found in our study could be explained mainly due to the small size, which was 3 times larger in studies carried out elsewhere. In addition, in our context, the average duration of follow-up of the subjects was 2.67 years, while elsewhere it exceeds 10 years. The evaluation of BMI in our study and according to the presence or absence of the metabolic syndrome showed a higher average value in SM+ subjects than in SM- subjects, although the comparison did not have showed significant difference (P=0.25). In addition, 18% of the study population had a larger than normal waist circumference. However, this BMI found in SM+ subjects (26.95 kg/m²) testifies to an excess weight present in the latter. This finding is consistent with that found in the study by Fenn et al, where the mean BMI increased from 27.2 ± 6.8 to 30.1 ± 7.7 kg/m² [9]. This could be because the opioid system is linked to food intake and obesity risk. Therefore, the activation of the mu-opioid receptor increases the preference for sweet taste and therefore the ingestion of sweet foods that can lead to weight gain [10-11]. Furthermore, a study by Peles et al, showed that patients under OST with methadone did not show notions of weight gain with an average BMI still within the normal range (22.5 ± 3.4 to 23.7 ± 4.1) [12]. Indeed, for them the change in lifestyle from that of "street drug addict" to that of "patient under treatment" is directly responsible for the magnitude of the changes occurring during the first year of treatment. Continued weight gain could be related to increased desire for sweets [11], but could just as well be a common phenomenon comparable to that of the general population [13]. The prevalence of blood pressure was the highest among the factors associated with metabolic syndrome in our population with a frequency estimated at 22%. Such a result has already been reported by Maruyama et al who found a prevalence of 21.1% [6]. Much higher frequencies ranging from 44.9 to 62.3% have been found in other similar studies [14-15].In the exploration of lipid balance abnormalities, hypo HDL-cholesterolemia and hypertriglyceridemia were respectively represented at frequencies of 14 and 10% in our study population. These frequencies, although high and worrying, are far lower than those found in other studies [8]. The analysis of the carbohydrate component of the SM revealed that hyperglycemia was the most weakly represented determinant with a frequency of 2%. On this component, the data in the literature are relatively controversial. Indeed, authors such as Maruyama et al found a prevalence of hyperglycaemia estimated at 4.5%, while other studies carried out in the United States have shown that patients under OST with methadone had a prevalence of high blood sugar in the range of 11.4 to 43.0% [14-15]. Indeed, current use of opiates, including heroin and methadone, has been associated with decreased levels of secreted insulin, which may therefore contribute to hyperglycemia [16]. In addition, it seems that opiates can stimulate the secretion of glucagon, which is a hyperglycemic hormone.
5. Conclusions
- The results of our study show that the chronic administration of methadone could actually promote the onset of the metabolic syndrome. However, these results should be confirmed by additional studies on a larger scale on the follow-up of these patients over time.CONFLICT OF INTERESTS: The authors have not declared any conflict of interest.CONSENT: Written and informed consent was obtained from each participant.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML