-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2020; 10(1): 1-4
doi:10.5923/j.ajb.20201001.01

Assessment of Serum Immunoglobulin E Level in Children with Bronchial Asthma in North West Rajasthan
Gajanand Joshi, R. K. Vyas, Yogita Soni, Ghanshyam Gahlot
Department of Biochemistry, S.P. Medical College, Bikaner (Rajasthan), India
Correspondence to: Gajanand Joshi, Department of Biochemistry, S.P. Medical College, Bikaner (Rajasthan), India.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bronchial Asthma (BA) is the most prevalent chronic respiratory disease among children causing considerable morbidity and mortality. Immunoglobulin E (IgE) is known to be associated with type I hypersensitivity reactions. Objective of this study was to determine the correlation of IgE with bronchial asthma in children. A case control study was conducted on 50 newly diagnosed asthmatic patients and 50 healthy individuals of both sexes. Having age between 3 to 15 years over a period of two years. Serum immunoglobulin E was estimated by ELISA. Mean age of patients under study (n=50) was 8.14 ± 3.65 years. Out of the total (50) patients, 54% (27/50) were males with a male/female ratio of 1.17/1; 48% of patients (24/50) had age between 6-10 years. Mean serum concentration of IgE was calculated to be 268.72 ± 130.14 IU/L in patient group while control group had a mean of 97.58 ± 25.10 IU/L. The difference was observed to statistically significant (P<0.0001) by student’s t-test. Serum immunoglobulin E (IgE) level has direct correlation with bronchial asthma among children.
Keywords: Bronchial asthma (BA), Immunoglobulin E (IgE), ELISA
Cite this paper: Gajanand Joshi, R. K. Vyas, Yogita Soni, Ghanshyam Gahlot, Assessment of Serum Immunoglobulin E Level in Children with Bronchial Asthma in North West Rajasthan, American Journal of Biochemistry, Vol. 10 No. 1, 2020, pp. 1-4. doi: 10.5923/j.ajb.20201001.01.
Article Outline
1. Introduction
- Bronchial asthma (BA) is a type I hypersensitivity reaction where immunoglobulin E (IgE) antibodies along with various allergens produce airway inflammation and symptoms of bronchial asthma. IgE is a trace protein and normally accounts for less than 0.001% of total serum immunoglobulin. IgE is capable of triggering the most powerful immune reactions. Because IgE is a mediator of allergic response, quantitative measurement of IgE, when integrated with other clinical indicators, can provide valuable information for the differential clinical diagnosis of atopic and non-atopic diseases. IgE evaluation is valuable in the diagnostic assessment of patients with recognized or suspected allergic diseases. [1] Studies have shown that condition such as BA, allergic rhinitis, eczema, urticaria, atopic dermatitis and some parasitic infections lead to increased IgE levels. The evidence for a causal relationship between allergens and BA hinges on epidemiologic findings showing a strong association between specific Immunoglobulin E (IgE) antibodies or total IgE and BA. [2] The present study was designed to assess and compare serum IgE level in childhood bronchial asthmatics and in healthy control subjects and to obtain the correlation of serum IgE levels with bronchial asthma.
2. Subjects and Method
- A case-control observational analytic study was carried out in the Department of Biochemistry in collaboration with the Out Patient Department of Pediatrics at S.P. Medical College and attached group of hospitals, Bikaner during a period from the beginning of August 2016 to the end of July 2018. A total of 100 subjects were divided into two groups. Group I / bronchial asthmatic patients consisted of 50 randomly selected, newly diagnosed subjects of both the sexes aged between 3 to 15 years with clinically confirmed diagnosis of bronchial asthma (as per Global Initiative for Asthma - GINA guidelines) but not being on any treatment for bronchial asthma. Group II / control group consisted of age and sex matched 50 healthy subjects having similar socio-economic status. All subjects were interviewed before being clinically examined in the outpatient department based on a questionnaire. The questionnaire contained data on demographic factors, types of habits, detailed clinical history and general physical examination. Venous blood samples (5ml) were collected from each of the study and control group subjects under universal aseptic precautions and transferred to pre-labeled, clean, metal free, plain test tubes (having no anticoagulants). These samples were left at room temperature for 20 minutes (allowing to be clotted), centrifuged at 2500 rpm for 15 minutes and supernatant serum was sent to Immuno Assay Lab for the evaluation of immunoglobulin E by means of Enzyme Linked Immuno Sorbent Assay (ELISA).Results were recorded and analyzed using Microsoft Excel 2007 and Biostatistics OPSTAT Software. Quantitative variables were summarized as mean ± standard deviation. Student’s T – test was applied to assess statistical significance. P value <0.05 was considered as significant.
3. Results
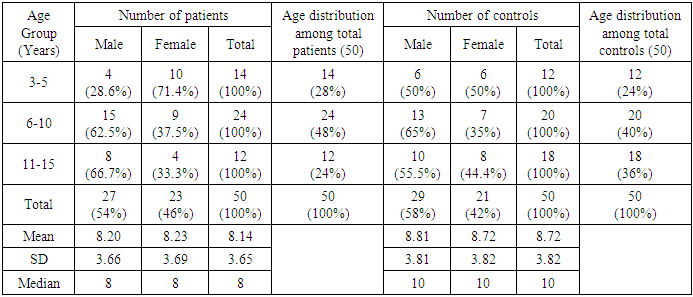
- In present study, we observed that mean age of patients with childhood asthma (n=50) was 8.14 ± 3.65 years and median age was 8 years, age range being 3 to 15 years (Table 1). 28% of the asthmatic patients (14/50) were between the age of 3-5 years and 48% (24/50) between 6-10 years old, while 24% (12/50) were between 11-15 years age (Figure 1 & 2). Out of the total (50) patients, 54% (27/50) were males and 46% (23/50) were females (i.e. male/female ratio 1.17/1) (Figure 3). A corresponding number of healthy subjects with same age and sex were selected as a control group (n=50).
|
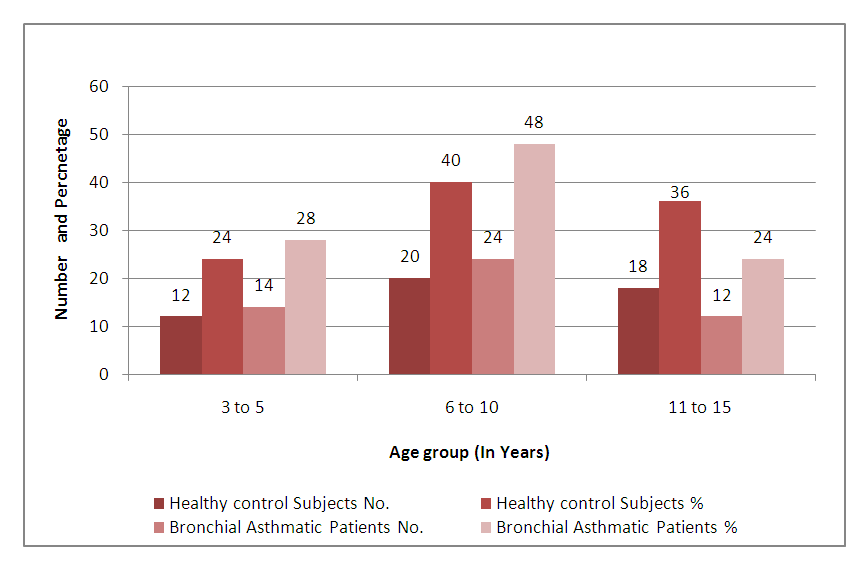 | Figure 1. Comparison of Healthy control subjects and Bronchial Asthmatic Patients on the basis of their Age |
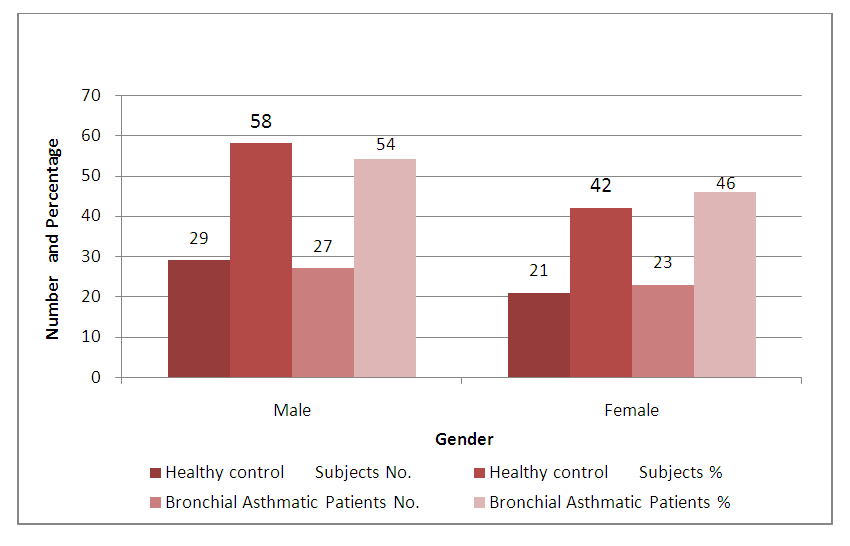 | Figure 2. Comparison of Healthy control subjects and Bronchial Asthmatic Patients on the basis of their Gender |
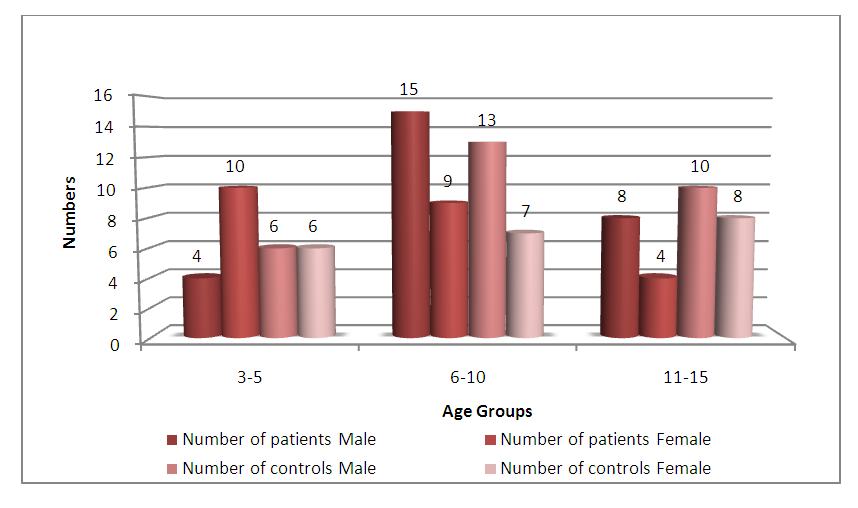 | Figure 3. The distribution of age and sex for both patients and controls |
|
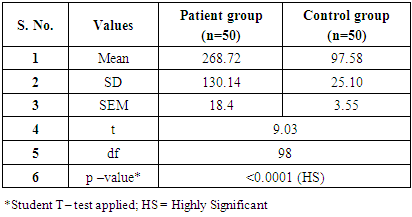
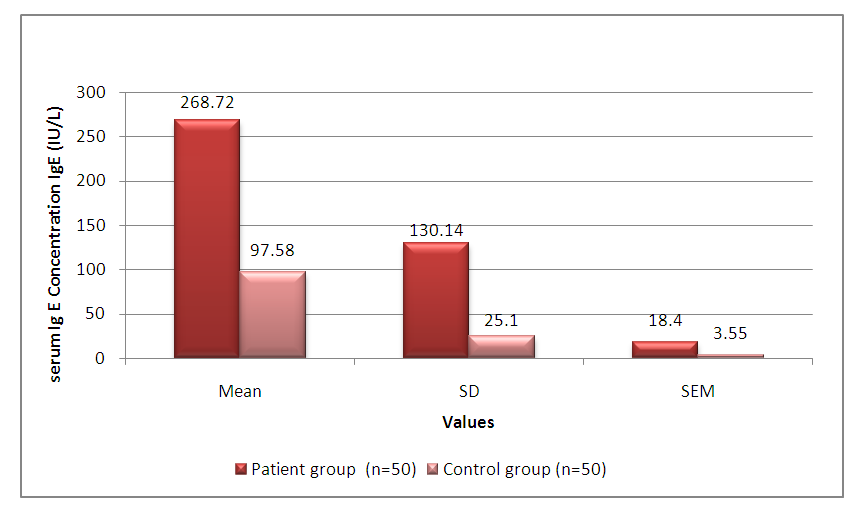 | Figure 4. Comparison of mean serum levels of IgE among the patients with childhood asthma against the control group |
4. Discussion
- The present study had shown that among the patients with childhood asthma, 27 (54%) of individuals were males, which is comparable with other studies done by Kakaras & Al-Rabaty [3] (54% males), Mahmood [4] (70% males patients), Hazim [5] (71% males), Kalyoncu et al [6] (73% males) and Hasan [7] (62% male asthmatic patients). Ghaffari et al [8] also reported high significant levels of IgE in BA patients, which is in accordance with the present study. I-Jen Wang wt al [9] and Joseph et al [10] suggested that excessive production of IgE might increase the risk of asthma among children who were basically being screened for serum lead (Pb) levels. The increase of serum total IgE level could be due to assess of allergic base of asthma (expression of TH2 cytokines such as IL4). [11]All the above results and whole discussion leads us to the fact that trace protein Immunoglobulins E (IgE) definitely have its effects on body immunity and alteration in its levels can contribute to induce or could have a strong correlation with bronchial asthma among children.
5. Conclusions
- Serum Immunoglobulin E (IgE) level has a strong direct correlation with bronchial asthma among children. Serum IgE levels being highly significant among the patients (P <0.0001) with childhood asthma when compared with healthy individuals of similar age and sex. In conclusion, the elevated level of serum IgE may exhibit the allergic etiology of asthma in the subjects studied. Increase in severity of asthma leads to increase in the level of immunoglobulin level. Consequently elevation in serum IgE levels contributes to asthma and is considered a potent predictor of the development of asthma. This study is a preliminary investigation and it has of course certain limitations. Lack of local references levels in another limiting factor. Further wider scale studies are required for better assessment of IgE status in childhood bronchial asthma.
ACKNOWLEDGEMENTS
- Authors are extremely grateful to Principal & Controller, S.P. Medical College, Associated Group of Hospitals, Bikaner and all indoor and outdoor patients making it possible for us to conduct this work in this institution.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML