-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2018; 8(3): 56-59
doi:10.5923/j.ajb.20180803.02

A Study to Evaluate Alterations in Liver Function Tests in Uncomplicated Malaria
C. Suvarna Devi 1, H. A. Nadiger 2, D. Rajarajeswari 3, M. Krishnamma 4, M. Prasad Naidu 5
1Assistant Professor, Department of Biochemistry, Narayana Medical College, Nellore, Andhra Pradesh, India
2Professor, Department of Biochemistry, University Sultan Zainal Abidin Medical Campus, Jalan Sultan Mahmud, India
3Professor, Dept of Biochemistry, Narayana Medical Collage & Hospital, Nellore, Andhra Pradesh, India
4Professor and HOD Dept of Biochemistry, Narayana Medical Collage & Hospital, Nellore, Andhra Pradesh, India
5Assistant Professor in Dept of Biochemistry, Narayana Medical Collage & Hospital, Nellore, Andhra Pradesh, India
Correspondence to: C. Suvarna Devi , Assistant Professor, Department of Biochemistry, Narayana Medical College, Nellore, Andhra Pradesh, India.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Malaria is endemic throughout most of the tropics. Malaria is a major cause of mortality in India. Abnormal Liver Function Tests (LFT) have been documented in severe malarial infections. Altered LFT in uncomplicated malaria have not been well documented. The present study is aimed to study alterations in LFT in uncomplicated malaria. Materials and Methods: This study included a total of 100 subjects (40 malaria patients, 30 age and sex matched controls and 30 non-malarial patients with fever). Venous blood sample (5ml) was collected from all subjects and serum was used for estimating LFT by auto analyser VITROS 250. Results: Data were analysed using appropriate statistical methods. In liver function tests, total bilirubin and direct bilirubin were highly significantly elevated (p<0.001), but the total protein and serum albumin levels were highly significantly decreased (p <0.001) in malaria patients when compared with control and non malarial group. AST level was significantly increased (p value 0.026) in non malarial group and in malaria group (p -value 0.019) when compared with control group, but there was no significant difference (p-value 1.000) between non malarial and malaria groups. There was moderately significant increase (p <0.01) in ALT level in non malarial group and highly significant elevation (p<0.001) of ALT level seen in malaria group when compared with control group. When compared with non malarial group there was moderately significant elevation (p value <0.01) of ALT in malaria group. There were no significant difference (p>0.05) in ALKP and GGT levels between three groups. In this study significant elevation of bilirubin and liver enzymes AST and ALT were observed. Conclusion: This concludes that the assessment of alteration in the liver function tests in malaria patients could represent additional and useful parameters in determining the clinical and prognostic aspects of the disease.
Keywords: Uncomplicated Malaria, Serum Bilirubin, Serum total protein, Serum albumin, Hepatic enzymes
Cite this paper: C. Suvarna Devi , H. A. Nadiger , D. Rajarajeswari , M. Krishnamma , M. Prasad Naidu , A Study to Evaluate Alterations in Liver Function Tests in Uncomplicated Malaria, American Journal of Biochemistry, Vol. 8 No. 3, 2018, pp. 56-59. doi: 10.5923/j.ajb.20180803.02.
Article Outline
1. Introduction
- Malaria is endemic throughout most of the tropics. India alone contributes about 70% of the 2.5 million reported cases in South East Asia [1, 2]. Indian towns are increasing in size and population at the cost of environmental safety [3]. Poor urban town planning without sanitary disposal of solid and liquid wastes from dwellings is leading to breeding of mosquitoes. The result is mosquito preponderance and diseases. Very few cities are having underground drainage facilities for sewage disposal [4].Malaria is difficult to diagnose clinically. Based on statistics more than two third Indian population lives in malarial zones [5]. The diagnosis of malaria is made, with an identification of malaria parasite with signs and symptoms associated with the disease [6]. Abnormal liver function tests (LFT) have been documented in severe malarial infections [7]. Altered LFT in uncomplicated malaria have not been well documented. The present study is aimed to evaluate alterations in LFT in uncomplicated malaria.
2. Material and Methods
- This was a cross sectional study included a total of 100 subjects (40 malaria patients, 30 age and sex matched controls and 30 non-malarial patients with fever). 5ml of venous blood sample was collected from all subjects after taking their consent and ethical clearance. Serum was used for estimating LFT by auto analyser VITROS 250. INCLUSION CRITERIA: All malaria positive (smear/strip positive) cases. Patients with non-malarial febrile illness. EXCLUSION CRITERIA: Patients with non-malarial hemorrhagic febrile illness (Eg: Dengue) and complicated malaria.
3. Results
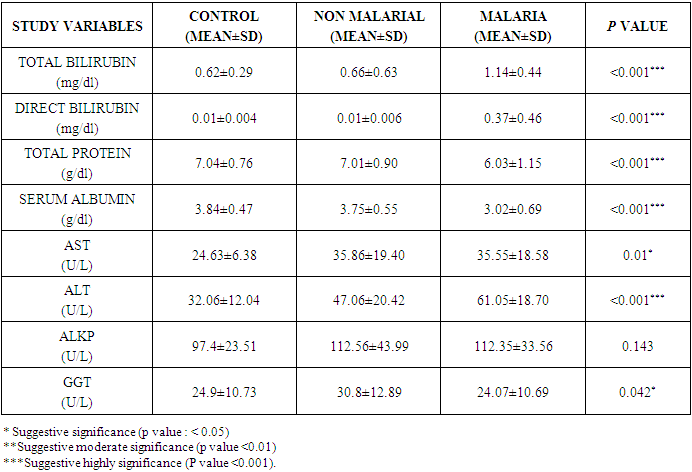
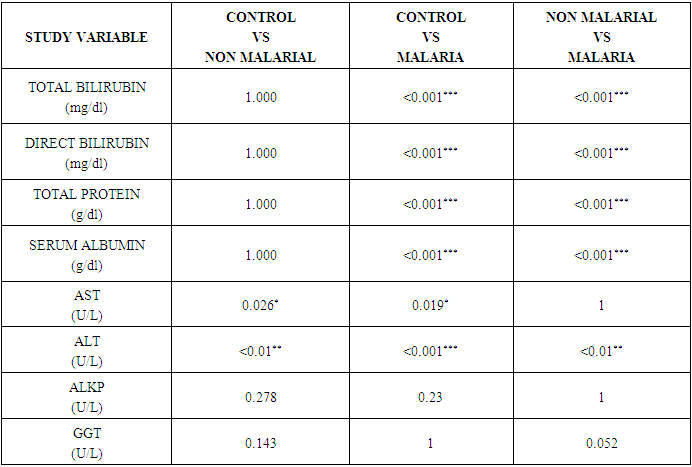
- Results were analysed using SPSS 20 version software. Comparisons between the groups were done by one way analysis of variance (ANOVA) to compare the mean values in all groups followed by multiple comparison post- hoc tests and P value <0.05 was considered significant.Table 1 and 2, Figure 1 shows that The mean values of total bilirubin (1.14±0.44) and direct bilirubin (0.37±0.46) in malaria patients with fever were highly significantly elevated (p<0.001) when compared with control total bilirubin (0.62±0.29) & direct bilirubin (0.01±0.004) and non malarial groups total bilirubin (0.66±0.63) & direct bilirubin (0.01±0.006). The mean values of total protein (6.03±1.15) and albumin (3.02±0.69) in malaria patients with fever were highly significantly decreased when compared with control total protein (7.04±0.76) & albumin (3.84±0.47) and non malarial groups total protein (7.01±0.90) & albumin (3.75±0.55). The mean AST level was significantly elevated in malaria group (35.55±18.58) when compared with control group (24.63±6.38) and no significant difference when compare with non malarial group (35.86±19.40). The mean value of ALT (61.05±18.70) in malaria patients was significant elevated when compared with control group (32.06±12.04) and non malarial groups (47.06±20.42). There was no significant increase in mean values of ALKP (112.35±33.56) and GGT (24.07±10.69) in malaria patients when compared with control ALKP (97.4±23.51) & GGT (24.9±10.73) and non malarial groups ALKP (112.56±43.99) & GGT (30.8±12.89).
|
|
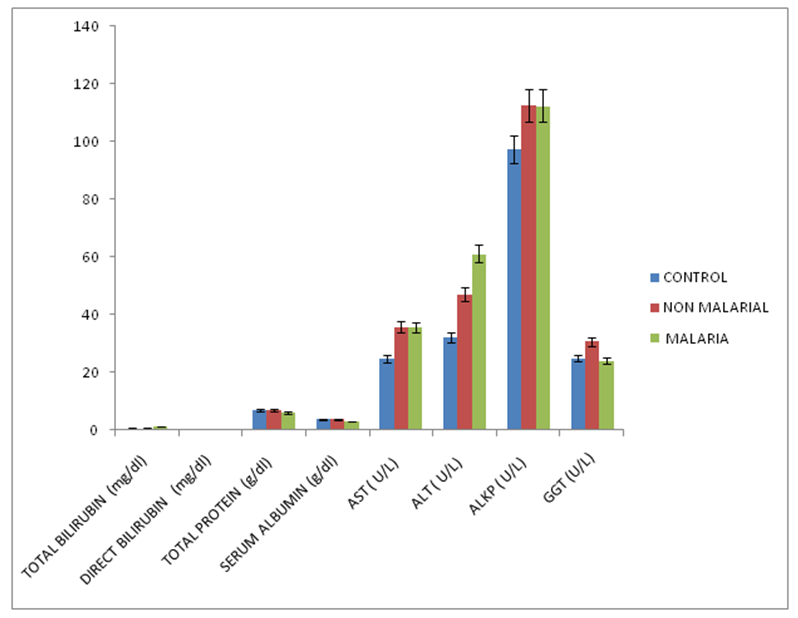 | Figure 1. Bar Diagram Showing Mean Biochemical Parameters Values between Three Groups |
4. Discussion
- The present study showed that liver dysfunctions also occurred in the uncomplicated malaria patients, without clinically significant complications. The mean values of total bilirubin (1.14±0.44) and direct bilirubin (0.37±0.46) in malaria patients were highly significantly elevated (p<0.001) when compared with control total bilirubin (0.62±0.29) & direct bilirubin (0.01±0.004) and non malarial groups total bilirubin (0.66±0.63) & direct bilirubin (0.01±0.006) [8]. Invasion of the human erythrocytes by the malaria parasite is accompanied by a variety of biological responses. These include the reactive oxygen species generated in the major host-parasite interactions [9]. Increase in ROS and decrease in antioxidants has been reported in malaria patients. Alterations in the major antioxidants of the erythrocytes and the peroxide mediated lysis of the erythrocytes may result in elevation of serum bilirubin [10, 11]. The elevated total bilirubin is due to elevation in both conjugated and unconjugated bilirubins suggesting that the ‘subclinical jaundice’ (hepatocelluar type) as yellow discoloration manifests only beyond 2.0 mg/dL. In the present study the mean values of total protein (6.03±1.15) and serum albumin (3.02±0.69) in malaria patients were highly significantly decreased (p <0.001) when compared with control group total protein (7.04±0.76) & serum albumin (3.84±0.47) and non malarial group total protein (7.01±0.90) & serum albumin (3.75±0.55). There was decreased total protein and serum albumin because majority of the patients attending PES hospital come from rural areas with poor literacy [12]. The decrease in serum albumin observed in malaria patients might be due to either malnutrition before treatment or the malaria infection itself. At present, there is no study showing increased vascular permeability in malaria infection and causing hypoalbuminemia.In the present study the mean AST value was significantly increased (p < 0.05) in malaria patients (35.55±18.58) and also in non malarial group (35.86±19.40) when compared with control group (24.63±6.38), but there was no significant difference between malaria and non malarial groups (p >0.05) [13]. The rise in AST both in malaria and non-malaria cases appears to be nonspecific since in both cases the levels were within reference range. The mean ALT value was highly significantly increased (p <0.001) in malaria patients (61.05±18.70) and moderate significantly increased (p <0.01) in non malarial group (47.06±20.42) when compared with control group (32.06±12.04) and also there was moderate significance (p <0.01) between malaria and non malarial group. The rise in ALT in malaria cases appears to be significant and could support mild hepatic involvement [14]. However, since RBCs also have a high ALT activity this study does not confirm the origin of the elevated ALT. The liver damage may have been caused by the free radicals generated by Plasmodium falciparum malaria. Increased production of hydroxyl and peroxide radicals induced by Plasmodium falciparum parasites may be responsible for the changes in AST and ALT levels. Transaminases are the important markers of hepatocellular damage. The alanine aminotranferase is more specific to the liver damage because it is predominantly produced within the liver cells [14]. There were no significant difference (p <0.05) in ALKP and GGT levels between three groups [15].
5. Conclusions
- Involvement of liver in complicated cases of malaria is well known fact. This study concludes that the assessment of alteration in the liver function tests in uncomplicated malaria cases could represent additional and useful parameters in determining the clinical and prognostic aspects of the disease. The results of our study provide valuable information and association between hepatic biochemical derangements in malaria patients. This study was performed on a small sample size and provided useful information in these subjects, there is a need to conduct study on large sample size and correlate the extent of altered LFTs with parasite load and severity of the disease.
ACKNOWLEDGEMENTS
- Cooperation with Department of Biochemistry, PES Institute of Medical Sciences and Research, Kuppam, Andhra Pradesh.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML