-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2017; 7(1): 10-12
doi:10.5923/j.ajb.20170701.03

Auto Immune Antibody Titres in Hypothyroid Disorders
Sajimon Thomas1, Jithesh TK2, Suresh S3, Sudheesh M4
1Department of Biochemistry, Al Azhar Medical College, Thodupuzha, Kerala, India
2Department of Biochemistry, MES Medical College, Perinthalmanna, Kerala, India
3Department of Biochemistry, School of Medical Education, Mahatma Gandhi University, Kottayam, Kerala, India
4Indiragandhi Dental College, Department of Biochemistry, Kothamangalam, Ernakulam, Kerala, India
Correspondence to: Jithesh TK, Department of Biochemistry, MES Medical College, Perinthalmanna, Kerala, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Thyroid disorders are quite common in both males and females. Hypo thyroidism is more widely present than hyper thyroidism, especially among females. Materials and methods: The determinations of serum triiodothronine (T3), tetraiodothyronine (T4), thyroid-stumulating hormone (TSH), free triiodothyronine (FT3), free tetraiodothyronine (FT4), antithyroperoxidase (anti-TPO) and antithyroglobulin (anti-Tg) antibodies were done by using the chemiluminescent immunoassay (CLIA). The data from the above investigations of the case group and the control group were statistically analyzed employing the unpaired Student’s t test. Result: Approximately one third of the hypothyroid patients had increased titres of anti-TPO and anti-Tg antibodies. The positivity of anti Tg antibodies was about half of that of anti TPO, while positivity of both the antibodies was about one sixth of anti-TPO antibodies. Conclusion: The incidence of thyroid disorders is on the high side among the world population affecting both sexes, but with a female predominance. It can be concluded from this study that hypothyroid condition is a frequent thyroid disorder among different age groups.
Keywords: Hypothyroidism, Tri triodothyronine (T3), Tetra tetraiodothyronine (T4), Thyroid-stimulating hormone (TSH), Free triiodothyronine (FT3), Free tetraiodothyronine (FT4), Anti-thyroperoxidase (anti-TPO) and anti-thyroglobulin (anti-Tg) antibodies
Cite this paper: Sajimon Thomas, Jithesh TK, Suresh S, Sudheesh M, Auto Immune Antibody Titres in Hypothyroid Disorders, American Journal of Biochemistry, Vol. 7 No. 1, 2017, pp. 10-12. doi: 10.5923/j.ajb.20170701.03.
1. Introduction
- Current estimates suggest that thyroid disorders affect as many as 9-15% of the adult female population and a smaller percentage of adult males. This gender-specific prevalence almost certainly results from the underlying autoimmune mechanism for the most common forms of thyroid disease, which include both Graves’ and Hashimoto’s disease [1, 2]. Hypothyroidism and hyperthyroidism are the two primary disorders that involve the thyroid gland. Hypothyroidism is a common disorder that occurs in mild or severe forms in 2 to 15% of the population. Hypothyroidism can also occur less frequently from the lack of stimulation by thyroid-stimuating hormone (TSH) from the pituitary. Tertiary hypothyroidism, due to hypothalamic dysfunction is rare [3-5]. Hashimoto’s thyroiditis is one of the common causes of primary hypothyroidism, which is 5-10 times more common in women than in men and most often starts in adulthood [6-9]. In North America, the most common cause of thyrotoxicosis due to hyperthyroidism is Grave’s disease, an autoimmune disease, which accounts for 60 to 80% of thyrotoxicosis [10]. The disorder rarely begins before adolescence and typically occurs between 20 and 50 years of age, though it also occurs in the elderly [2]. Overproduction of thyroid hormones can also result from autonomous production by solitary or multiple thyroid nodules or from excessive TSH secretion by pituitary tumours [11, 12].Abnormalities in thyroid functions are one of the commonest endocrine disorders observed in the general population. Females are predominantly affected more than males, especially in auto immune thyroid disorders. The massive iodination of common salt programmes of the Government is to prevent this menace, but unfortunately, this plan alone could not eradicate hypothyroidism at least in certain sections of the population. It has been observed that hypothyroidism may occur even when the thyroid hormone levels are normal. This has been attributed to the presence of anti-thyroid antibodies and goitrogenic factors [13, 14]. There is considerable evidence that abnormalities of circulating thyroid hormones and TSH characteristic of the euthyroid--sick syndrome are associated with adverse outcome regarding morbidity and mortality related to other illnesses [15]. This association undoubtedly reflects the influence of ‘non-thyroidal’ illnesses of increasing severity on thyroid hormone metabolism and TSH secretion. Studies on thyroid dysfunction and other risk factors are scanty from this area even though the prevalence is reportedly higher [16, 17]. The present study was undertaken to evaluate the thyroid hormone status along with the presence of autoantibodies in hypothyroid subjects.
2. Materials and Methods
- Subjects: The study was conducted in association with the Department of Medicine, Medical College Hospital, Kottayam, India. Informed consent was obtained from the outpatient volunteers for the study, and the Clinical Proforma of each participating person was completed and collected. After getting clearance from the Institutional Ethics Committee (IEC), the blood samples taken from the volunteers were processed and analysed at Dianova Laboratories, a fully automated speciality clinical laboratory at Kottayam. The subjects for the study were selected primarily based on the following inclusion-exclusion criteria.Hypothyroid Group:- Both men and women in the age group of 31 to 50 years who were having the symptoms of hypothyroidism like fatigue or lack of energy, weight gain, cold intolerance, heavy menstrual periods, constipation and slowed thinking, but who were not on any treatment for thyroid disorders were selected in the hypothyroid group (N=200).Control Group: Asymptomatic, apparently healthy men and women subjects in the age group of 31 to 50 years having none of the symptoms mentioned above was included in the control group (N=100). The final selection of subjects in the hypothyroid as well as the control group was based on serum triiodothyronine (T3), tetraiodothyronine (T4), and TSH levels.Specimen collection and processing: We collected 5 ml of blood in a clot activator vacutainer. Then we allowed the blood to clot at room temperature. Afterwards, we centrifuged and collected the serum, which was stored at -20to -80°C for assay in the same day or at -200°C if the storage was expected to be more than one day.Methods: The determinations of serum T3, T4, TSH, free triiodothyronine (FT3), free tetraiodothyronine (FT4), anti-thyroperoxidase (anti–TPO) and anti-thyroglobulin (anti-Tg) antibodies were done by using chemiluminescent immuno assay (CLIA) in an Advia Centaur-fully automated CLIA analyzer of Siemens Health Care Diagnostics, India, Ltd., using their reagents, calibrators, controls and standards. Quality Control was performed by participating in the BIO-RAD EQUAS International Quality Control programmes [vendor and location]. The data from the above investigations of the case group and the control group were statistically analysed employing the unpaired Student’s t-test. All statistical procedures and tests were conducted using Sigma Stat 6.5 Version Software (Sigma-Aldrich Co., St. Louis, USA).
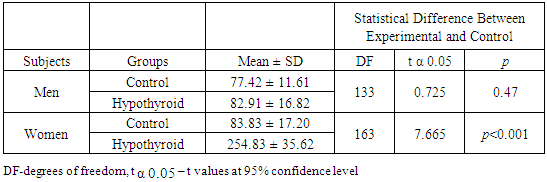
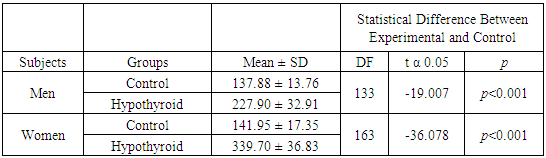
3. Results
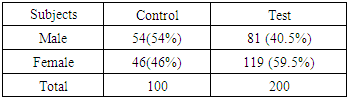
- The sex-wise distribution of the test and control subjects is given in Table 1.
|
|
|
4. Discussion
- The incidence of thyroid disorders is on the high side among the world population affecting both sexes, but with a female predominance. It can be concluded from this study that hypothyroid condition is a common thyroid disorder among different age groups in both males and females with an approximate frequency of 20% and 30% respectively. Several studies on the prevalence of thyroid dysfunction and its relation to thyroid autoantibodies in apparently healthy people reported that the thyroid autoantibodies were positive in 13.8% of females [18]. There was an age-related increase in the prevalence of positive thyroid autoantibodies, and the frequency was about 7% below 30 years of age, and 14% above 30. The overall prevalence of Hashimoto’s thyroiditis in females in the general Japanese population was 13%. In the present study, more than 55% women had autoimmune causes for their hypothyroidism as against 12% in men. There is a preponderance of hypothyroid women subjects in the age group of 31-40 than those in the 41-50 age groups. Results of this study also indicate that autoimmune causes of hypothyroidism are far more common in women of 31-40 age group compared with those in the 41-50 age group [19]. The thyroid autoantibodies are significantly elevated in hypothyroidism, indicating an autoimmune cause of hypothyroidism.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML