-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Biochemistry
p-ISSN: 2163-3010 e-ISSN: 2163-3029
2017; 7(1): 6-9
doi:10.5923/j.ajb.20170701.02

Vitamin D Deficiency and Inflammatory Marker in Subjects with Dyslipidemia
Shifa K.1, Jithesh T. K.1, Mirshad P.2, Supriya Simon A.3
1Dept. of Biochemistry, MES Medical College, Peritnthalmanna, India
2Dept of Pharmacology, MES Medical College, Peritnthalmanna, India
3Government Medical College, Thrissur, India
Correspondence to: Jithesh T. K., Dept. of Biochemistry, MES Medical College, Peritnthalmanna, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

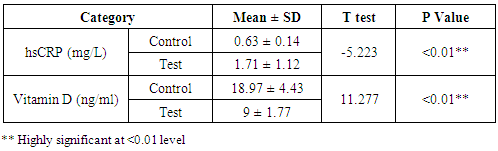
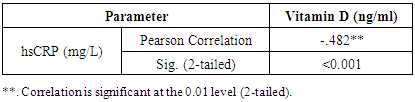
Background: Aim of this study was to compare the levels of inflammatory marker and vitamin D in subjects with and without dyslipidemia. An attempt was also made to correlate the inflammatory changes with vitamin D levels in the study subjects. Material and Method: A cross-sectional study was conducted in a tertiary care teaching hospital. Twenty-nine subjects with dyslipidemia were included as test and 30 age and sex matched healthy individuals without dyslipidemia were selected as control population. Five ml of the fasting blood samples were collected from all the subjects and used for the analysis of vitamin D, Lipid profiles (Total cholesterol, triglycerides, HDL, LDL, VLDL) and high-sensitivity C-reactive protein (hsCRP). Result: The levels of hsCRP were significantly high (p<0.01) whereas vitamin D levels were significantly low (p<0.01) in subjects with dyslipidemia compared to the control subjects. The Pearson Correlation between hsCRP and Vitamin D showed statistically significant negative correlation suggesting that a decrease in vitamin D increase the inflammatory process. Conclusion: Vitamin D levels are low and hsCRP levels are high in subjects with dyslipidemia. The negative correlation between the vitamin D level and hsCRP among the test population indicates that vitamin D deficiency may contribute to the inflammatory process.
Keywords: Vitamin D, Dyslipidemia, Cardiovascular diseases, Inflammatory marker, Lipid profiles, High-sensitivity C-reactive protein
Cite this paper: Shifa K., Jithesh T. K., Mirshad P., Supriya Simon A., Vitamin D Deficiency and Inflammatory Marker in Subjects with Dyslipidemia, American Journal of Biochemistry, Vol. 7 No. 1, 2017, pp. 6-9. doi: 10.5923/j.ajb.20170701.02.
1. Introduction
- Traditionally, Vitamin D is considered as a fat-soluble vitamin involved in calcium homeostasis and bone mineral metabolism. Unlike the other fat-soluble vitamins, it is synthesized endogenously and shares the properties of hormones; hence, Vitamin D is also considered as a pro hormone. [1] Recent researches on Vitamin D revealed that it is not only involved in the homeostasis of bone but also take part in various physiological functions in the body. It is now documented that vitamin D receptors are present on a large variety of cell types, including osteoblasts, immunologic cells, nerve cells, pancreatic beta cells, vascular endothelial cells, and possibly myocytes and cardiac muscle cells. [2] Latest evidence indicates that low levels of vitamin D may adversely affect the functions of various organs, therefore impact total survival. [2] Deficiency of vitamin D is now recognized to be highlyprevalent in worldwide, impacting between 30% and 50% of the general population. Traditionally, vitamin D deficiency has been associated primarily with development of rickets in children and osteomalacia in adults. However, the recent findings reveal that deficiency of vitamin D may cause autoimmune diseases, infections, increase the risk for hypertension, diabetes mellitus, coronary artery disease, stroke, cancer etc. [3]Vitamin D plays an important role in the modulation of the immune and inflammatory system. Several studies have associated lower vitamin D status with increased risk and unfavorable outcome of acute infections. Inflammation is involved in many chronic diseases and concern has been raised about the influence of vitamin D deficiency on inflammatory processes. Some of the studies have recommended vitamin D supplementation in inflammatory diseases due to strong correlation with vitamin D deficiency. [4] The association between vitamin D deficiency and susceptibility to infections of the respiratory tract has been suggested for many years, but has not been clearly proven. Children with nutritional rickets used to develop rachitic lung due to infections of the respiratory tract and cod liver oil was used to treat tuberculosis.Apart from the inflammatory diseases, the studies also reported that vitamin D deficiency is associated with increased risk of cardiovascular diseases including hypertension, heart failure, ischemic heart disease. [5] A growing body of data suggests that low 25-hydroxy Vitamin D levels may adversely affect cardiovascular health. Vitamin D deficiency increases the risk of developing incident hypertension or sudden cardiac death in individuals with pre existing cardiovascular diseases. [6] Dyslipidemia is an independent risk factor for cardiovascular and cerebrovascular diseases in individuals. [7, 8] Current studies have observed that low 25-hydroxyvitamin D is associated with dyslipidemia. [9, 10]C-reactive protein (CRP) has been used as an inflammatory marker in various clinical conditions. Increased CRP level may increase the risk not only for cardiovascular diseases but also for cancer, diabetes, inflammation etc. Findings from various studies have shown that deficiency of vitamin D hasten the inflammatory process and thereby increase the risk for CVD. [11] Some of the previous studies conducted in our area showed high prevalence of vitamin D deficiency in the locality. [12] This study was undertaken to compare the levels of inflammatory marker and vitamin D in subjects with and without dyslipidemia. An attempt was also made to correlate the inflammatory changes with vitamin D levels in the study subjects.
2. Material and Method
- A cross-sectional study was conducted in a tertiary care teaching hospital after obtaining approval from institutional ethics committee (IEC/MES/42/2014). Blood samples were collected from people who attended a medical camp conducted by the hospital. Written informed consent was obtained from all the participants. Total 59 cases were enrolled to the study, grouped into test (n=29), and control (n=30). Subjects with dyslipidemia as per the NCEP- ATP III criteria were included in test population. [13] Age and sex matched 30 healthy individuals without dyslipidemia were selected as control population.The demographic parameters like age, height, body weight, sex, and BMI were noted and recorded. The collected samples were prepared to analyze biochemical parameters. Fully automated analyzer (Mindray BS200) used to analyze the biochemical parameters like vitamin D, lipid profiles (Total cholesterol, triglycerides, HDL, LDL, VLDL) and high-sensitivity C-reactive protein (hsCRP). Statistical analysis was performed using SPSS (version 17.0). The analysis was performed on the set of all eligible subjects enrolled in the study according to the study protocol. Probability values of p < 0.05 were considered statistically significant. A statistical program called Minitab 15, that allows data entry and analysis were also used to analyze the data.
3. Results
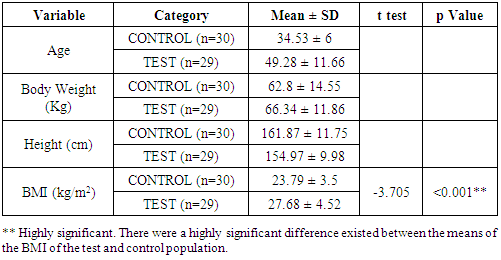
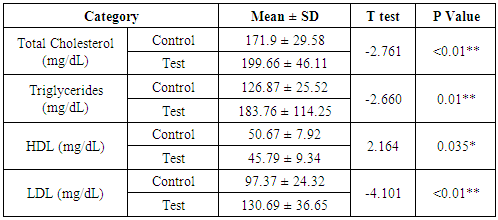
- The blood samples and demographic details were collected from people who attended the medical camp. A total of 59 people were enrolled as subject and out of these, 30 were control and 29 were test population. There were eighteen (62.0%) males and eleven (37.9%) females in the test group and fifteen (50%) males and fifteen (50%) females in the control group. The average age was 49.28 years among the test population and that of the control group was 34.53 years. The average body weight of the test population was slightly higher (66.34 kg) when compare to that of control group (62.8kg). The result showed that the BMI of test population is higher than that of control group (Table 1). The result of Student’s t-test performed between the control and test population clearly revealed the significant difference in values of total cholesterol, triglycerides, HDL and LDL level (Table 2).
|
|
|
|
4. Discussion
- This study investigated the level of inflammatory marker and Vitamin D in subjects with and without dyslipidemia . We found that the Vitamin D level was low in the test population compared to the control population where as CRP was higher in the test population when compared to the control. The findings were similar with the findings of Wang TJ et al and Anderson JL, et al. [14, 15] There were a statistically significant negative correlation observed between the CRP and vitamin D suggesting that a decrease in vitamin D hasten the inflammatory process. Vitamin D acts as an anti-inflammatory agent by decreasing the production of proinflammatory cytokines and modulation of tissue specific immune response. [16] Similar result was obtained in a study conducted by Liu C et al. They found an inverse correlation between 25(OH) D and hsCRP levels. [17] Elevated hsCRP level has been associated with higher risk for cardiovascular events in older patients without preexisting cardiovascular disease. An earlier study conducted by unrevealed that the hsCRP level is higher in patients with metabolic syndrome with higher risk for cardiovascular diseases. [18]This study clearly indicates that vitamin D levels are significantly low whereas hsCRP levels are significantly high in subjects with dyslipidemia. We also observed that as the vitamin D levels decreases the levels of inflammatory marker increases in dyslipidemia. Relatively small sample size (n= 59) is the main limitation of the study. These findings should be confirmed in a larger sample size and in a prospective manner.
5. Conclusions
- Vitamin D levels are low and hsCRP levels are high in subjects with dyslipidemia. The negative correlation between the vitamin D level and hsCRP among the test population indicates that vitamin D deficiency may contribute to the inflammatory process. Further studies with larger study population are required to establish the role vitamin D in the inflammatory process and role in cardiovascular diseases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML